For those driven by a unique blend of scientific rigor, profound compassion, and the ability to remain calm under immense pressure, the field of pediatric anesthesiology represents a pinnacle of medical practice. It is a career that asks for everything—years of dedicated study, unwavering focus, and a deep understanding of the most vulnerable patients—but in return, it offers immense personal and financial rewards. Aspiring physicians are often drawn to the challenge and the impact, but they also have a practical question: what does a pediatric anesthesiologist salary truly look like?
This guide will provide a definitive answer. We will move beyond simple averages to explore the complex tapestry of factors that shape compensation in this elite specialty. The national average salary for a pediatric anesthesiologist is substantial, often ranging from $380,000 to over $550,000 annually, with top earners in high-demand locations and practice models exceeding this considerably.
I still vividly recall the overwhelming fear in my cousin's eyes when, at age six, he needed emergency surgery. The surgeon was a distant, technical figure, but the anesthesiologist knelt down to his level, explaining in simple terms how he would get some "superhero sleeping gas" to take a nap and wake up all better. That moment of human connection, of providing safety and dispelling fear in a terrifying environment, is the intangible heart of this profession—a value that complements its impressive financial compensation.
This article is your comprehensive roadmap. We will dissect every component of a pediatric anesthesiologist's salary, explore the long-term career outlook, and provide a step-by-step guide for those ready to embark on this challenging but incredibly fulfilling journey.
### Table of Contents
- [What Does a Pediatric Anesthesiologist Do?](#what-does-a-pediatric-anesthesiologist-do)
- [Average Pediatric Anesthesiologist Salary: A Deep Dive](#average-pediatric-anesthesiologist-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion: Is This Demanding Path Right for You?](#conclusion-is-this-demanding-path-right-for-you)
What Does a Pediatric Anesthesiologist Do?

A pediatric anesthesiologist is a fully trained anesthesiologist who has completed at least one additional year of specialized fellowship training in the care of infants and children. Their role is far more nuanced than simply "putting a child to sleep" for a procedure. They are the perioperative physicians for the pediatric population, responsible for the child's safety, comfort, and physiological stability before, during, and after surgery.
The core principle of this specialty is that children are not just small adults. Their physiology is fundamentally different. An infant's heart rate, blood pressure, airway anatomy, drug metabolism, and temperature regulation vary dramatically from an adult's—and even from a teenager's. A pediatric anesthesiologist possesses an expert-level understanding of these differences across the entire spectrum of development, from premature neonates weighing only a few pounds to robust adolescents.
Core Responsibilities Include:
- Preoperative Assessment: This involves a thorough evaluation of the child's medical history, a physical examination, and a careful review of any lab work or imaging. Crucially, it also involves building rapport with both the child and their parents or guardians. They must explain the anesthetic plan in an accessible, reassuring way, obtain informed consent, and manage preoperative anxiety, which can have a significant impact on a child's recovery.
- Anesthetic Planning and Administration: Based on the child's health status, age, weight, and the nature of the surgery, the anesthesiologist devises a tailored anesthetic plan. This could involve general anesthesia, regional anesthesia (like an epidural or nerve block), or sedation. They are masters of various techniques, including difficult airway management, which is more common in children with congenital syndromes.
- Intraoperative Management: Once the surgery begins, the pediatric anesthesiologist becomes the child's guardian angel in the operating room. They continuously monitor vital signs—heart rate, breathing, blood pressure, oxygen levels, and temperature. They manage fluid and blood replacement, administer medications to control pain and maintain physiological balance, and are prepared to respond instantly to any life-threatening emergency, such as an allergic reaction, breathing complications, or sudden blood loss.
- Postoperative Care: Their responsibility does not end when the surgery is over. They oversee the child's immediate recovery in the Post-Anesthesia Care Unit (PACU), managing pain, nausea, and any other side effects of anesthesia. For complex cases, they may continue to be involved in the child's pain management on the pediatric ward or in the intensive care unit (ICU).
### A Day in the Life of a Pediatric Anesthesiologist
5:45 AM: The alarm goes off. Dr. Evans arrives at the children's hospital by 6:30 AM, changing into scrubs and grabbing a coffee. The first order of business is reviewing the day's caseload. The list includes a 2-year-old for ear tube placement, a 9-year-old with a broken arm needing hardware placement, and the most complex case: a 3-month-old infant with a congenital heart defect scheduled for a multi-hour open-heart surgery.
7:00 AM: Dr. Evans heads to the preoperative holding area to meet her first patient, the 2-year-old. She kneels down, showing the child a flavored anesthesia mask and letting him play with it. She speaks with the anxious parents, confirming the child has had nothing to eat or drink, answering their questions, and reassuring them with a calm, confident demeanor.
7:30 AM: In the operating room, she ensures all her equipment—the anesthesia machine, monitors, emergency airway cart—is checked and ready. She administers the anesthetic, often while the child is sitting on a parent's lap, to make the transition as gentle as possible. Once the child is asleep, the parent leaves, and Dr. Evans expertly secures the airway and stabilizes the child for the short procedure.
8:30 AM: While the first patient is waking up comfortably in the PACU, Dr. Evans is already preparing for the 9-year-old. This case involves a regional nerve block to ensure excellent postoperative pain control. Using an ultrasound machine, she meticulously guides a needle to place numbing medication around the specific nerves of the arm, a skill that significantly improves the patient's recovery experience.
10:00 AM - 4:00 PM: The main event: the infant cardiac surgery. Dr. Evans works in concert with a pediatric cardiac surgeon, a perfusionist (who runs the heart-lung machine), and a team of specialized nurses. This is where her expertise shines. She places complex intravenous and arterial lines in tiny vessels, manages massive fluid shifts and blood transfusions, and carefully titrates powerful drugs to protect the infant's brain and other organs while the heart is stopped for repair. She is in a state of hyper-vigilance for hours, interpreting subtle changes in monitors and responding instantly.
4:30 PM: The cardiac surgery is a success. Dr. Evans meticulously transports the stable but critically ill infant to the Pediatric ICU, giving a detailed and thorough handover to the intensive care team who will manage the next phase of recovery.
5:30 PM: After checking on her other patients and completing extensive electronic charting for the day, Dr. Evans finally heads home, mentally exhausted but deeply satisfied, knowing her skills made a life-saving surgery possible for a sick child.
Average Pediatric Anesthesiologist Salary: A Deep Dive
The compensation for pediatric anesthesiologists is among the highest in the medical field, reflecting the extensive training, high-stakes nature of the work, and significant demand for their specialized skills. While salaries can vary widely, the data consistently points to a robust and lucrative career path.
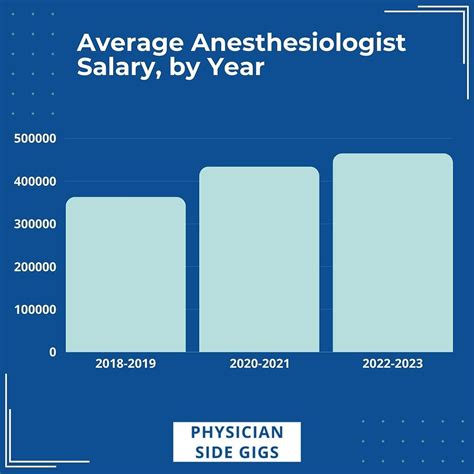
According to the 2023 Medscape Physician Compensation Report, the average salary for general anesthesiologists is $448,000. Pediatric anesthesiologists, due to their subspecialty fellowship training, typically command salaries at or often above this average. Data from salary aggregators further refines this picture for the pediatric subspecialty.
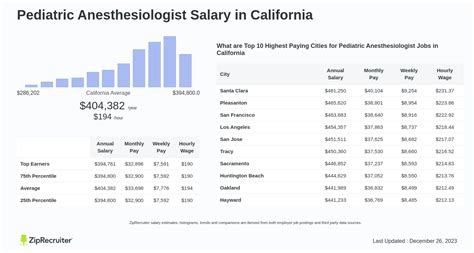
Salary.com, which provides granular data based on employer-reported surveys, states that the median annual salary for a Pediatric Anesthesiologist in the United States is approximately $456,861 as of late 2023. The typical salary range falls between $395,739 and $518,011. However, this range represents the core bulk of earners; the top 10% can earn $579,158 or more, while the bottom 10% (likely representing those just out of fellowship or in lower-paying academic roles) start around $334,467.
### Salary Brackets by Experience Level
Salary progression in this field is significant. As physicians gain experience, their efficiency, ability to handle complex cases, and value to their practice group or hospital increases, directly impacting their compensation.
| Experience Level | Typical Timeframe | Average Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-3 Years Post-Fellowship | $350,000 - $420,000 | Focus on building clinical speed and confidence. Often in salaried hospital or academic positions. May have lower initial productivity-based bonuses. |
| Mid-Career | 4-10 Years | $420,000 - $510,000 | Peak clinical efficiency. Potential for partnership in private practice. Often taking on mentorship or minor administrative roles. Higher bonus potential. |
| Senior/Late-Career | 11+ Years | $480,000 - $600,000+ | Often in leadership roles (e.g., Department Chair). May be a senior partner in a private group. High earning potential, sometimes with a shift towards more administrative duties or a reduced clinical load. |
*(Source: Data compiled and synthesized from Salary.com, Medscape, and Doximity compensation reports.)*
### Deconstructing the Full Compensation Package
The base salary is only one part of the equation. A pediatric anesthesiologist's total compensation is a package that includes several other valuable components. When evaluating a job offer, it's crucial to look beyond the base number.
- Base Salary: This is the guaranteed annual income. In hospital-employed or academic models, this makes up the bulk of the compensation. In private practice, it may be a lower guaranteed amount, with the majority of earnings coming from productivity.
- Productivity Bonuses: This is a major component, especially in private practice and many hospital-employed models. It is often calculated using Relative Value Units (RVUs). RVUs are a measure set by Medicare to value the work involved in a medical procedure. The more complex and time-consuming the case (e.g., an 8-hour infant cardiac surgery vs. a 15-minute ear tube procedure), the more RVUs it generates. Anesthesiologists are often paid a certain dollar amount per RVU generated above a specific threshold.
- Sign-On Bonus: To attract top talent in a competitive market, many hospitals and private groups offer substantial sign-on bonuses, which can range from $20,000 to $100,000 or more. These are often tied to a commitment to stay with the employer for a set number of years (typically 2-3).
- Retirement Contributions: This is a significant factor in long-term wealth building. Employers typically offer a 401(k) or 403(b) plan with a matching contribution. A generous match (e.g., 4-6% of salary) can add tens of thousands of dollars to your savings each year. Some private practice partnerships offer even more robust profit-sharing or defined-benefit plans.
- Malpractice Insurance: This is a non-negotiable and extremely expensive necessity. Virtually all employers cover the full cost of malpractice insurance for their physicians. "Claims-made" policies are common, and a crucial benefit to negotiate is "tail coverage," which protects the physician from claims made after they leave the practice.
- Continuing Medical Education (CME) Stipend: Physicians are required to complete a certain number of educational hours each year to maintain their license and board certification. Employers provide an annual stipend, typically $3,000 to $7,000, to cover the costs of conferences, textbooks, and review courses.
- Other Benefits: A comprehensive benefits package also includes high-quality health, dental, and vision insurance; short-term and long-term disability insurance; life insurance; and a generous paid time off (PTO) policy, which typically ranges from 6 to 10 weeks per year.
Understanding these components is key. A job offer with a $420,000 base salary and a robust profit-sharing plan, full tail coverage, and an 8% retirement match may be far more lucrative in the long run than a $450,000 salary with minimal benefits and no bonus structure.
Key Factors That Influence Salary

The national averages provide a useful benchmark, but an individual pediatric anesthesiologist's salary is determined by a complex interplay of several key factors. Understanding these variables is essential for negotiating job offers and maximizing long-term earning potential. This is the most critical section for anyone looking to understand the "why" behind the numbers.
### 1. Level of Education and Certification
In medicine, the educational pathway is largely standardized, but it forms the absolute foundation of earning potential. There is no shortcut.
- Medical Degree (M.D. or D.O.): This is the mandatory entry point. The four years of medical school are the start of the journey.
- Anesthesiology Residency: A four-year, intensive training program covering all aspects of general anesthesiology.
- Pediatric Anesthesiology Fellowship: This is the crucial differentiating step. The one-year (or sometimes two-year, for highly specialized areas like pediatric cardiac anesthesia) fellowship provides the subspecialty expertise that commands a premium salary. Physicians who are "grandfathered" in or only practice pediatrics occasionally without fellowship training will not have access to the top-tier jobs or salaries.
- Board Certification: After residency, anesthesiologists must pass rigorous written and oral exams to become board-certified by the American Board of Anesthesiology (ABA). After fellowship, they must then pass additional exams to achieve a subspecialty certification in Pediatric Anesthesiology. Maintaining these certifications is required for practice at any reputable institution and is a prerequisite for high earnings. Lack of board certification would be a major red flag for employers and would severely limit employment and salary options.
### 2. Years of Experience
As detailed in the previous section, experience is a primary driver of salary growth. This isn't just about time served; it's about the accumulation of skills and value.
- Early Career (0-3 years): Physicians are building speed, confidence, and a reputation for reliability. Their RVU productivity may be lower as they acclimate. Salaries are high but generally on the lower end of the specialty's range.
- Mid-Career (4-10 years): This is often the period of peak earning *growth*. Physicians have mastered their clinical skills, can handle the most complex cases efficiently, and are highly productive. In private practice, this is when they typically become a full partner, which dramatically increases their income as they transition from a salaried employee to a business owner sharing in the profits.
- Senior Career (11+ years): While clinical skills remain sharp, senior physicians often transition into roles that add value beyond direct patient care. They may become the Chief of Anesthesiology, the Medical Director of the Operating Rooms, or serve on key hospital committees. These leadership roles come with additional stipends and administrative pay that boost their overall compensation. Senior partners in private groups reap the benefits of a mature and profitable business.
### 3. Geographic Location
Geography is one of the most significant and variable factors influencing physician salary. The principle of supply and demand is in full effect. Higher salaries are not always in the most glamorous or populous cities; in fact, they are often found in areas that need to pay a premium to attract highly specialized talent.
- High-Paying States and Regions: Historically, the Midwest, Southeast, and non-coastal Western states tend to offer higher compensation for physicians. This is due to a combination of factors: fewer medical schools and residency programs (lower supply), less competition for jobs, and a greater need to attract specialists away from the major coastal hubs. States like North Dakota, Wisconsin, Alabama, Oklahoma, and Indiana often appear on lists of top-paying states for anesthesiologists.
- Lower-Paying States and Regions: Conversely, major metropolitan areas on the East and West Coasts (e.g., Boston, New York City, San Francisco, Los Angeles) tend to have lower average salaries. While the cost of living in these cities is exceptionally high, the desirability of living there, coupled with a high concentration of academic medical centers and a large supply of physicians, creates more competition and suppresses salaries.
- Rural vs. Urban: A hospital in a rural or underserved area will almost always have to pay a significant premium to recruit a pediatric anesthesiologist compared to a major children's hospital in a big city that receives hundreds of applications for every opening. This "rural premium" can sometimes amount to a difference of over $100,000 per year.
Illustrative Regional Salary Comparison for Anesthesiologists (General):
| Metro Area | Average Salary (Approximate) | Cost of Living Index (US Avg = 100) | Notes |
| :--- | :--- | :--- | :--- |
| Milwaukee, WI | $475,000 | 96.5 | High demand, lower cost of living boosts take-home pay. |
| Birmingham, AL | $468,000 | 79.1 | Strong healthcare market in the Southeast, very low cost of living. |
| Charlotte, NC | $482,000 | 100.4 | Growing city with high demand for specialists. |
| Boston, MA | $405,000 | 153.2 | Highly desirable, saturated market with many academic centers. |
| San Francisco, CA | $415,000 | 243.8 | Extremely high cost of living significantly erodes purchasing power. |
*(Source: Data synthesized from Doximity, Salary.com, and cost-of-living data from Payscale.)*
### 4. Practice Type and Employment Model
The setting where a pediatric anesthesiologist works is arguably the single most important factor in determining their salary structure and ultimate earning potential.
- Private Practice (Physician-Owned Group): This model offers the highest earning potential. Physicians typically join a group as a salaried employee for 2-3 years on a "partnership track." After this period, if they meet the group's standards, they are offered the chance to "buy-in" and become a partner. As a partner, they are a business owner, sharing directly in the profits of the group. This model requires more business acumen and administrative responsibility, but the financial rewards can be substantial, with senior partners often earning well above $600,000 or $700,000.
- Hospital or Health System Employee: This is the most common model today. The physician is a direct employee of the hospital or a large healthcare network. This offers greater stability, predictable hours (though still long), excellent benefits, and no administrative burden of running a business. The trade-off is a lower earning ceiling. Salaries are generous but are less likely to reach the top-tier levels of a private practice partner. Compensation is often a mix of base salary and productivity bonuses.
- Academic Medical Center: Working for a university-affiliated hospital involves a "three-fold mission": clinical care, teaching, and research. The base salaries in academia are almost always lower than in private practice or even general hospital settings. A typical "academic discount" can be anywhere from $50,000 to $150,000 per year. The trade-offs are non-monetary: the prestige of working at a renowned institution, the intellectual stimulation of teaching medical students and residents, opportunities for groundbreaking research, and often a better work-life balance and more generous benefits.
- Locum Tenens: This means "to hold the place of." Locum tenens anesthesiologists are temporary, independent contractors who fill in for physicians who are on vacation, on leave, or to cover staffing shortages. They are paid a very high daily or hourly rate (e.g., $2,500 - $4,000+ per day) and their travel and lodging expenses are covered. This offers maximum flexibility and high short-term income but comes with no benefits, no job stability, and constant travel.
### 5. Area of Sub-Subspecialization
Within the specialty of pediatric anesthesiology, there are further areas of focus that can increase complexity and, therefore, compensation.
- Pediatric Cardiac Anesthesiology: This is arguably the most demanding and highest-paid sub-subspecialty. These experts complete an additional year of fellowship (for a total of two years post-residency) focused solely on anesthesia for children undergoing surgery for congenital heart defects. The procedures are long, the patients are critically ill, and the required skill level is immense. These roles are concentrated at major tertiary care children's hospitals and command a significant salary premium.
- Pediatric Pain Management: Some pediatric anesthesiologists also become board-certified in pain medicine. They manage acute and chronic pain in children, running clinics and performing advanced interventional procedures. This dual-specialization can open up additional revenue streams and increase overall compensation.
- Pediatric Critical Care (ICU): While less common, some anesthesiologists complete fellowships in both pediatric anesthesiology and pediatric critical care, allowing them to work in both the operating room and the Pediatric ICU. This dual skillset makes them highly valuable to a children's hospital.
### 6. In-Demand Skills (Technical and Soft)
Beyond formal certifications, a specific set of skills can make a candidate more attractive and justify higher pay.
- Technical Skills: Proficiency in ultrasound-guided regional anesthesia is paramount. The ability to perform precise nerve blocks improves patient outcomes and makes a candidate highly desirable. Expertise in advanced techniques like transesophageal echocardiography (TEE) for cardiac cases is also a major value-add.
- Soft Skills: Excellence in communication is non-negotiable. The ability to reassure a terrified child and calm anxious parents is a skill that directly impacts patient satisfaction and the hospital's reputation. Leadership ability, composure under extreme stress, and a collaborative spirit are essential for functioning effectively in the high-stakes operating room environment.
Job Outlook and Career Growth

For those willing to undertake the extensive training, the career outlook for pediatric anesthesiologists is exceptionally strong and stable. The combination of an aging physician workforce, a growing population, and the increasing complexity of pediatric surgical interventions ensures a robust demand for these highly specialized professionals for the