Introduction

Embarking on a career in medicine is a monumental decision, often fueled by a deep-seated desire to heal, serve, and make a tangible impact on people's lives. Among the many specialties, family medicine stands out as the cornerstone of healthcare, the very bedrock upon which patient-doctor relationships are built. If you're drawn to the idea of being a community's trusted health advisor, guiding families through every stage of life, then you're considering a path that is as rewarding as it is demanding. But beyond the profound sense of purpose, a practical question looms large for any aspiring physician: What is the financial reality of this career? What is the average salary for a family medicine physician?
This guide is designed to provide a definitive answer to that question and many more. We will move beyond a single number to explore the complex tapestry of factors that determine a family doctor's earnings, from geographic location and practice type to the invaluable impact of experience. You can expect to see an average salary range that typically falls between $220,000 and $280,000 per year, with top earners and practice owners exceeding $350,000. These figures, supported by data from the most reputable sources in the industry, paint a picture of a stable, lucrative, and highly respected profession.
As a career analyst, I've seen countless individuals weigh their passion against practicality. I recall a conversation with a newly matched resident who, after years of grueling study, was most excited not by the future salary, but by the prospect of working in the same clinic where her own family doctor had treated three generations of her family. That enduring legacy and community trust is the intangible income of this profession; our goal here is to illuminate the tangible compensation that makes such a dedicated career possible.
This comprehensive article will serve as your ultimate resource, whether you are a high school student contemplating a pre-med track, a medical student choosing a specialty, or a practicing physician considering a career pivot.
### Table of Contents
- [What Does a Family Medicine Physician Do?](#what-they-do)
- [Average Salary for a Family Medicine Physician: A Deep Dive](#salary-deep-dive)
- [Key Factors That Influence Salary](#key-factors)
- [Job Outlook and Career Growth](#job-outlook)
- [How to Get Started in This Career](#how-to-start)
- [Conclusion](#conclusion)
What Does a Family Medicine Physician Do?

A family medicine physician, often called a family doctor, is a medical generalist who provides comprehensive healthcare for individuals and families across all ages, genders, and stages of life. They are the quintessential primary care providers (PCPs), serving as the first point of contact for patients navigating the complexities of the healthcare system. Unlike specialists who focus on a specific organ or disease, a family physician's specialty is the patient themselves, viewed within the context of their family and community.
The scope of family medicine is exceptionally broad, encompassing elements of internal medicine (adults), pediatrics (children), obstetrics and gynecology (women's health), geriatrics (the elderly), and even behavioral health. This "cradle-to-grave" continuity of care is the hallmark of the profession, allowing physicians to build long-term, trusting relationships that are fundamental to effective healthcare.
Core Roles and Responsibilities:
- Diagnosis and Treatment of Acute Illness: This includes everything from common colds, influenza, and infections to injuries like sprains and minor lacerations. They are the front line for unscheduled, urgent health concerns.
- Management of Chronic Conditions: A significant portion of a family physician's work involves helping patients manage long-term diseases such as hypertension (high blood pressure), diabetes, asthma, heart disease, and arthritis. This includes prescribing medication, monitoring progress, and counseling on lifestyle changes.
- Preventative Care and Health Promotion: This is a proactive and vital part of the role. It involves conducting annual physicals, wellness checks, and cancer screenings (e.g., Pap smears, mammograms, colonoscopies). They are also responsible for administering immunizations and educating patients on nutrition, exercise, and smoking cessation.
- Coordination of Care: When a patient requires specialized treatment, the family physician acts as the central coordinator, referring them to specialists like cardiologists, oncologists, or surgeons and ensuring that all aspects of their care are integrated and communicated effectively.
- Performing Minor In-Office Procedures: Many family doctors are trained to perform procedures such as joint injections, skin biopsies, cryotherapy (freezing warts), suturing minor wounds, and inserting long-acting contraceptives.
- Administrative and Documentation Tasks: Like all modern physicians, a significant amount of time is dedicated to maintaining accurate electronic health records (EHR), responding to patient messages, refilling prescriptions, and handling insurance-related paperwork.
### A Day in the Life of a Family Medicine Physician
To make this role more tangible, let's walk through a typical day for a hospital-employed family physician.
- 7:00 AM - 8:00 AM: Hospital Rounds & Administrative Prep
The day might begin at the local hospital, checking on a few admitted patients—perhaps an elderly patient with pneumonia or a newborn for a well-child check before discharge. Back at the office, the physician reviews the day's schedule, looks over lab results that came in overnight, and responds to urgent messages in the EHR patient portal.
- 8:30 AM - 12:00 PM: Morning Clinic Session
The first patient is a 45-year-old man for his annual physical, which involves discussing preventative screening, updating vaccinations, and counseling on his slightly elevated cholesterol. The next is a 6-year-old with a sore throat and fever, requiring a physical exam and a rapid strep test. This is followed by a 68-year-old woman with well-controlled diabetes for her quarterly check-up, where they review her blood sugar logs and adjust her medication. The morning might end with a 30-year-old woman seeking consultation for anxiety, involving a compassionate discussion and the development of a treatment plan that includes therapy and possibly medication.
- 12:00 PM - 1:00 PM: Lunch and Administrative Catch-Up
Lunch is often a working period. The physician might use this time to return calls to specialists, sign prescription refills, and complete chart notes from the morning's appointments. They may also attend a quick departmental meeting or a "lunch-and-learn" session sponsored by a pharmaceutical company.
- 1:00 PM - 4:30 PM: Afternoon Clinic Session
The afternoon brings a new set of diverse cases. A 25-year-old athlete needs a knee injection for bursitis. A follow-up visit with a 55-year-old man recently diagnosed with high blood pressure reveals that the new medication is working well. A teenager comes in for an acne consultation. The physician might also perform a small skin biopsy on a suspicious mole.
- 4:30 PM - 5:30 PM: Charting and Final Tasks
With the last patient gone, the final hour is a race against the administrative clock. Every visit must be meticulously documented in the EHR for clinical accuracy, legal protection, and billing purposes. The physician reviews the last of the day's lab results, signs off on charts, and creates a to-do list for the next day. Depending on the practice's schedule, this physician might be "on-call" tonight, meaning they are responsible for answering urgent after-hours patient calls.
This snapshot illustrates the incredible variety and demanding pace of family medicine. It is a career that requires vast medical knowledge, exceptional communication skills, deep empathy, and remarkable efficiency.
Average Salary for a Family Medicine Physician: A Deep Dive
The compensation for a family medicine physician is a reflection of their extensive education, rigorous training, and the critical role they play in the healthcare ecosystem. While salaries can vary significantly, the profession offers substantial financial security and a strong return on the immense investment of time and tuition.
It's important to understand that different data sources may report slightly different averages. This is due to variations in methodology—some rely on employer-reported data, others on physician self-reported surveys, and some include only base salary while others incorporate bonuses and production incentives. By synthesizing information from the industry's most trusted reports, we can build a highly accurate and nuanced picture of earning potential.
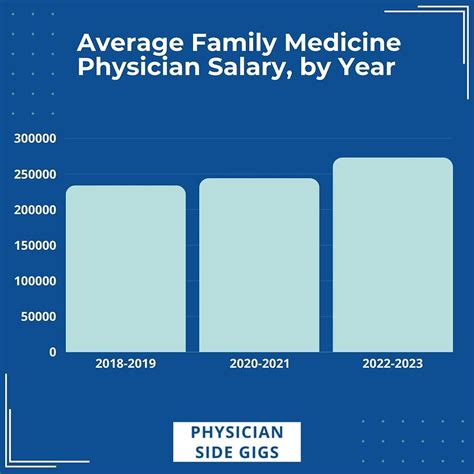
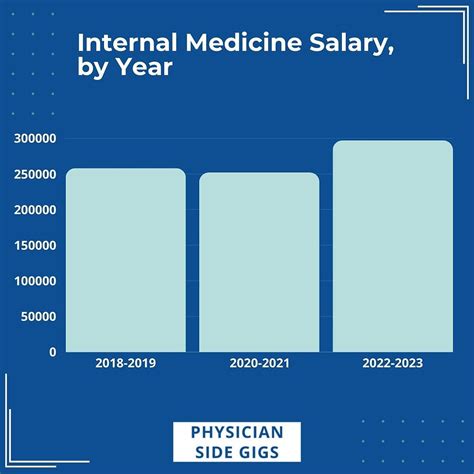
National Average Salary and Typical Range
According to the most recent and widely cited industry reports, the national average salary for a family medicine physician is firmly in the six-figure range.
- Medscape's 2023 Physician Compensation Report, one of the most comprehensive surveys in the field, places the average annual compensation for family physicians at $255,000.
- Doximity's 2023 Physician Compensation Report, another major industry study, reports a slightly higher average of $273,040 for family medicine physicians.
- The U.S. Bureau of Labor Statistics (BLS), in its May 2022 data (released in April 2023), reports a median annual wage of $224,460 for family medicine physicians. The BLS data shows a wide range, with the lowest 10 percent earning less than $117,720 and the top 10 percent earning more than $239,200. It's important to note that the BLS often reports slightly lower figures and may not fully capture the production bonuses that make up a significant portion of physician income.
- Reputable salary aggregator Salary.com, as of early 2024, reports a median salary of $228,890, with the middle 50% of family physicians earning between $205,190 and $254,090.
Taking all sources into account, a realistic national average salary for a family medicine physician in 2024 is approximately $250,000 to $270,000. The typical salary range for an established physician is broad, generally spanning from $200,000 to over $300,000 annually.
### Salary Brackets by Experience Level
A physician's salary is not static; it grows significantly from the early years of training to the peak of their career.
| Career Stage | Typical Annual Compensation Range | Key Characteristics |
| :--- | :--- | :--- |
| Medical Resident (PGY1-3) | $60,000 - $75,000 | This is a training salary, not a full physician's salary. It covers the 3-year family medicine residency after medical school. It varies by location and institution. |
| Entry-Level (0-3 Years Post-Residency) | $190,000 - $225,000 | The physician is now a board-certified attending. They are focused on building a patient panel. Often includes a guaranteed salary for the first 1-2 years. |
| Mid-Career (4-10 Years) | $225,000 - $280,000 | The physician has an established patient base, works more efficiently, and has often transitioned from a guaranteed salary to a production-based model (e.g., wRVU). |
| Senior / Experienced (10+ Years) | $280,000 - $350,000+ | At this stage, income potential is highest. This may be due to high patient volume, practice ownership/partnership, or taking on leadership roles (e.g., Medical Director). |
### Beyond the Base Salary: Understanding the Full Compensation Package
A family physician's total compensation is rarely just a flat salary. The offer letter for a new position will contain a variety of components that contribute significantly to their overall financial picture.
- Base Salary: The guaranteed annual income, paid bi-weekly or monthly. In many employment models, this is a floor, not a ceiling.
- Production Bonuses: This is arguably the most important variable in physician compensation today. It is most often based on Work Relative Value Units (wRVUs). A wRVU is a standardized measure of the time, skill, and intensity required to provide a particular patient service, as defined by Medicare. Physicians are assigned a dollar amount per wRVU they generate (e.g., $50 per wRVU). Once they generate enough wRVUs to cover their base salary and overhead, they earn a bonus for every additional wRVU. This model incentivizes seeing more patients or performing more complex services.
- Quality and Performance Bonuses: Increasingly common in the shift towards "value-based care." These bonuses are tied to specific patient outcomes and quality metrics. Examples include achieving certain vaccination rates in their patient panel, high patient satisfaction scores, or effectively managing the A1c levels of their diabetic patients. These can add $10,000 - $30,000 or more per year.
- Sign-On Bonus: To attract top talent, especially in underserved areas, healthcare systems often offer substantial sign-on bonuses. These can range from $20,000 to $50,000 or even higher, sometimes paid out over the first couple of years.
- Profit Sharing / Partnership Track: For physicians in private practice, this is the path to the highest earning potential. After a few years as an employee, a physician may be offered the chance to "buy in" to the practice, becoming a partner. As an owner, they share in the practice's profits, which can significantly boost income beyond what's typically possible in an employed model.
- Ancillary Benefits: These are highly valuable non-salary perks.
- Malpractice Insurance: Employer-provided "claims-made" or "occurrence" policies are standard. A key negotiation point is "tail coverage," which covers claims made after the physician leaves the practice.
- Health, Dental, and Vision Insurance: Comprehensive family plans are typical.
- Retirement Plans: Access to 401(k) or 403(b) plans, often with a generous employer match (e.g., 3-6% of salary).
- Continuing Medical Education (CME) Stipend: Physicians are required to complete a certain number of hours of continuing education each year to maintain their license. Employers typically provide an annual allowance of $3,000 - $5,000 and paid time off to attend conferences.
- Relocation Assistance: A reimbursement or lump sum payment (e.g., $5,000 - $15,000) to cover moving expenses for new hires.
- Loan Repayment Programs: A powerful recruitment tool. Some employers offer direct student loan repayment assistance. Furthermore, physicians working for non-profit organizations or in designated Health Professional Shortage Areas (HPSAs) may be eligible for federal programs like Public Service Loan Forgiveness (PSLF) or the National Health Service Corps (NHSC) Loan Repayment Program, which can be worth hundreds of thousands of dollars.
When evaluating a job offer, it is crucial to look at the entire package, as a lower base salary with excellent bonuses and benefits can often be more lucrative than a higher base salary with a less comprehensive package.
Key Factors That Influence the Salary of a Family Medicine Physician
The national average salary provides a useful benchmark, but an individual physician's actual earnings are determined by a complex interplay of several key factors. Understanding these variables is essential for anyone looking to maximize their earning potential in this field. This section breaks down the most significant drivers of salary variation.
###
Geographic Location: The Power of Place
Where a physician chooses to practice is one of the single largest determinants of their salary. This variation exists not just between states but also between urban, suburban, and rural areas within the same state. The dynamic is often counterintuitive: salaries are frequently higher in less populated, rural areas than in major metropolitan centers. This is a simple matter of supply and demand; rural communities must offer more competitive compensation packages to attract physicians away from desirable urban centers.
According to the Medscape 2023 Compensation Report, the states with the highest average physician compensation (across all specialties, a trend that generally holds for primary care) include:
1. Wisconsin: $397,000
2. Indiana: $372,000
3. Georgia: $363,000
4. Connecticut: $362,000
5. Missouri: $361,000
Conversely, the lowest-paying states often include:
1. Maryland: $304,000
2. Colorado: $312,000
3. Virginia: $323,000
4. Massachusetts: $324,000
5. Arizona: $327,000
*(Source: Medscape Physician Compensation Report 2023, average for all physicians)*
The Urban vs. Rural Divide: A family physician in a major city like New York City or San Francisco will likely earn less than their counterpart in rural North Dakota or Mississippi. A report from Doximity highlighted this, showing that metropolitan areas like Washington D.C., Boston, and Baltimore were among the lowest-paying, while Charlotte, NC and St. Louis, MO were among the highest. Why?
- Competition: Major cities have a high concentration of physicians and academic medical centers, leading to greater competition for positions and downward pressure on salaries.
- Cost of Living: While salaries in big cities are lower, the cost of living is dramatically higher, making the real, take-home pay even less.
- Recruitment Incentives: Rural hospitals and clinics offer premium salaries, significant sign-on bonuses, and generous loan repayment assistance as essential tools to recruit and retain medical talent. A physician willing to practice in a designated Health Professional Shortage Area (HPSA) can find some of the most lucrative opportunities available.
###
Practice Setting and Ownership Model
The type of organization a physician works for profoundly impacts their compensation structure, benefits, and long-term earning potential.
- Private Practice (Physician-Owned): This model offers the highest income potential. As a partner or sole owner, the physician not only earns a salary for their clinical work but also shares in the profits of the entire practice, including revenue from lab services, imaging, and other ancillary services. However, this comes with the greatest risk and administrative burden. Owners are responsible for managing staff, billing, payroll, IT, and all other aspects of running a small business. A senior partner in a successful multi-physician private practice can easily earn $350,000 - $450,000+ annually.
- Hospital or Health System-Employed: This is the most common model for physicians today. It offers stability, predictability, and excellent benefits. The physician is a salaried employee of the hospital or a large medical group owned by the hospital. They receive a steady paycheck, a comprehensive benefits package (including malpractice insurance), and are shielded from most administrative headaches. The trade-off is a lower income ceiling compared to practice ownership. The typical salary range is $220,000 - $280,000, with bonuses tied to productivity and quality metrics.
- Academic Medical Center: Physicians who work for university-affiliated hospitals balance clinical duties with teaching medical students/residents and conducting research. Compensation in academia is notoriously lower than in private or even standard hospital-employed settings. The average salary might be 10-20% less, often in the $180,000 - $230,000 range. The "payment" comes in the form of prestige, intellectual stimulation, and a different work-life balance that is less focused on high patient volume.
- Federally Qualified Health Centers (FQHCs) & Government: Working for an FQHC, the Department of Veterans Affairs (VA), or the military offers a unique package. Base salaries are often on the lower end of the spectrum (e.g., $170,000 - $220,000). However, the benefits are exceptional: outstanding job security, federal pensions, generous paid time off, and, most importantly, eligibility for robust loan forgiveness programs like Public Service Loan Forgiveness (PSLF). The work-life balance is often better, with less pressure for high productivity.
- Urgent Care Centers: These roles are often shift-based (e.g., three 12-hour shifts per week) and can be quite lucrative. Compensation is often paid hourly (e.g., $100-$130/hour) or as a salary, and can be very competitive, often reaching $240,000 - $300,000 or more, especially for experienced physicians. However, these roles lack the continuity of care that is the hallmark of traditional family medicine.
###
Years of Experience and Career Progression
As detailed in the salary bracket table, experience is a powerful