Table of Contents

- [What Does a Doctor of Osteopathic Medicine (DO) Do?](#what-does-a-doctor-of-osteopathic-medicine-do)
- [Average Doctor of Osteopathic Medicine Salary: A Deep Dive](#average-doctor-of-osteopathic-medicine-salary-a-deep-dive)
- [Key Factors That Influence a DO's Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth for DOs](#job-outlook-and-career-growth)
- [How to Become a Doctor of Osteopathic Medicine](#how-to-get-started-in-this-career)
- [Conclusion: Is a Career in Osteopathic Medicine Right for You?](#conclusion)
Are you drawn to the idea of a medical career that combines the rigorous, evidence-based practices of modern science with a hands-on, holistic approach to patient care? Do you envision yourself not just treating symptoms, but healing the whole person? If so, the path of a Doctor of Osteopathic Medicine (DO) may be your calling. It's a profession that offers immense personal fulfillment and, as we will explore in detail, significant financial rewards. The national average salary for physicians, including DOs, often exceeds $208,000 per year, with top specialists earning well over $500,000 annually.
However, the journey to becoming a physician is a marathon, not a sprint, and understanding the financial landscape is a critical part of planning your future. When my own cousin was weighing his options between an M.D. and a D.O. program, his deciding factor was a shadowing experience with a family medicine DO who used Osteopathic Manipulative Treatment (OMT) to resolve a patient's chronic back pain, avoiding the need for surgery. He saw firsthand how the osteopathic philosophy translates into a powerful, patient-centered clinical tool that sets this path apart.
This comprehensive guide is designed to be your definitive resource for understanding a Doctor of Osteopathic Medicine's salary and career trajectory. We will dissect every factor that influences your earning potential, from your chosen specialty and practice location to the type of healthcare system you work in. We'll explore the robust job outlook, map out the step-by-step educational journey, and provide the data-driven insights you need to make an informed decision about this exceptional career.
---
What Does a Doctor of Osteopathic Medicine (DO) Do?

A Doctor of Osteopathic Medicine (DO) is a fully licensed and practicing physician in the United States. This is the single most important concept to understand: DOs have the exact same legal and professional rights and responsibilities as their Allopathic (MD) colleagues. They can prescribe medication, perform surgery, deliver babies, and specialize in any medical field, from family medicine to neurosurgery.
So, what makes the DO designation unique? The distinction lies in the philosophy and training. Osteopathic medicine was founded in the late 19th century by physician Andrew Taylor Still, who pioneered a "whole person" approach to care. This philosophy is built on the core tenet that all parts of the body are interconnected and that the body possesses an innate ability to heal itself.
This philosophy manifests in a few key ways:
- Holistic Perspective: DOs are trained to look beyond the symptoms to understand the patient's entire system. They consider how lifestyle, environment, and mental well-being impact physical health, treating the patient as an integrated whole.
- Focus on the Musculoskeletal System: Osteopathic medicine places special emphasis on the musculoskeletal system—the intricate network of nerves, muscles, and bones. It posits that structural problems in this system can cause or exacerbate illness.
- Osteopathic Manipulative Treatment (OMT): This is the hallmark of osteopathic training. DOs receive an additional 200+ hours of training in a set of hands-on techniques used to diagnose, treat, and prevent illness or injury. OMT involves moving a patient's muscles and joints using techniques like stretching, gentle pressure, and resistance. It can be used to alleviate pain, improve mobility, and promote healing for a wide range of conditions, from headaches and back pain to asthma and sinus disorders.
### A Day in the Life of a Family Medicine DO
To make this tangible, let's imagine a typical day for Dr. Evelyn Reed, a DO specializing in family medicine in a suburban private practice.
- 8:00 AM - 9:00 AM: Morning Huddle and Chart Review. Dr. Reed meets with her nurse and medical assistant to review the day's patient schedule. She examines lab results that came in overnight, flags charts that need follow-up calls, and prepares for her first appointments.
- 9:00 AM - 12:00 PM: Morning Patient Appointments. The morning is a mix of cases. She sees a 65-year-old man for a routine diabetes check-up, adjusting his medication and discussing a new diet plan. Next, she sees a young mother and her infant for a well-child visit. Her third patient is a 45-year-old office worker complaining of persistent tension headaches and neck pain. After a thorough neurological exam, Dr. Reed identifies restricted motion in his cervical spine. She spends 15 minutes performing OMT, using gentle muscle energy techniques to restore motion and relieve his pain.
- 12:00 PM - 1:00 PM: Lunch and Administrative Tasks. Dr. Reed catches up on charting in the Electronic Health Record (EHR) system, answers patient messages through the online portal, and returns a call to a local pharmacist to clarify a prescription.
- 1:00 PM - 4:30 PM: Afternoon Patient Appointments. The afternoon brings a teenager for a sports physical, a patient for a minor skin biopsy, and a 55-year-old woman with acute lower back pain. After confirming there are no red-flag neurological symptoms, Dr. Reed diagnoses a lumbar strain and performs OMT to ease muscle spasms and improve function. She also prescribes a course of physical therapy and an anti-inflammatory medication.
- 4:30 PM - 5:30 PM: Finalizing the Day. Dr. Reed finishes her patient notes, signs off on prescription refills, and makes a follow-up call to the patient she saw earlier for headaches. She confirms he is feeling better and schedules a follow-up appointment to monitor his progress.
This "day in the life" illustrates how a DO seamlessly integrates all the tools of modern medicine—diagnostics, pharmacology, patient education—with the unique, hands-on modality of OMT to provide comprehensive and personalized care.
---
Average Doctor of Osteopathic Medicine Salary: A Deep Dive
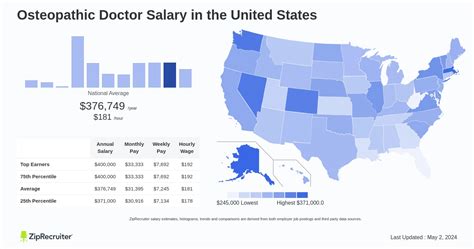
When considering a career with such a lengthy and demanding educational path, compensation is a critical factor. The financial rewards for Doctors of Osteopathic Medicine are substantial and are, for all practical purposes, on par with their MD counterparts. Salary is not determined by the letters after your name (DO vs. MD), but by factors like specialty, location, and practice setting.
According to the U.S. Bureau of Labor Statistics (BLS), the median annual wage for physicians and surgeons was $239,200 in May 2023. However, this figure groups all physicians together, from lower-paid primary care doctors to high-earning surgeons. To get a more accurate picture, we must turn to industry-specific reports.
The Medscape Physician Compensation Report 2024, one of the most respected and comprehensive surveys in the industry, provides a more granular look. It found the average overall physician compensation to be $363,000. The report highlights a key distinction:
- Average Primary Care Physician (PCP) Compensation: $274,000
- Average Specialist Compensation: $403,000
Since nearly 57% of DOs practice in primary care fields (family medicine, internal medicine, pediatrics), this distinction is crucial. However, DOs are increasingly entering high-paying specialty fields, where their earning potential is identical to MDs.
### Salary Progression by Experience Level
A physician's salary follows a distinct and predictable trajectory, beginning with the training years of residency and rising sharply upon entering practice.
| Career Stage | Typical Annual Salary Range | Key Details & Sources |
| :--- | :--- | :--- |
| Residency / Fellowship | $60,000 - $85,000 | During these 3-7+ years of post-graduate training, "residents" are paid a modest stipend. This salary is typically set by the institution and increases slightly each year. *(Source: Association of American Medical Colleges (AAMC), Medscape)* |
| Entry-Level (0-5 Years in Practice) | $200,000 - $350,000+ | Upon finishing residency, a DO's salary skyrockets. The exact starting figure is heavily dependent on specialty. A primary care DO might start around $220,000, while a new anesthesiologist or radiologist could start at $400,000 or more. *(Source: Doximity, Medscape)* |
| Mid-Career (6-20 Years) | $250,000 - $500,000+ | With experience, physicians become more efficient, build a larger patient base, and often see their compensation, especially production-based bonuses, increase. Many also take on leadership roles or become partners in their practice. *(Source: Doximity, Medscape)* |
| Senior / Late Career (20+ Years) | $275,000 - $600,000+ | Earnings typically peak in the late-career stage. While some physicians may choose to scale back their hours, those who continue in full-time clinical practice or administration command top-tier salaries based on their decades of expertise and reputation. *(Source: Medscape)* |
### Deconstructing the Compensation Package
A DO's total compensation is more than just a base salary. Understanding the full package is essential when evaluating job offers.
- Base Salary: This is the guaranteed annual income. In some models, particularly private practice, this might be a smaller portion of the total pay, acting as a "draw" against future earnings. In most hospital-employed models, it's the largest and most stable component.
- Production Bonuses (RVU-Based Compensation): This is a critical and highly common component of physician pay. Most work performed by a physician is assigned a "Relative Value Unit" (RVU). Hospitals and practices often set an RVU threshold, and physicians earn a bonus for every RVU they generate above that target. This model rewards productivity and efficiency. An experienced DO who can see more patients or perform more procedures efficiently will have a significantly higher income.
- Sign-On Bonus: To attract top talent, especially in high-need specialties or locations, healthcare systems offer substantial sign-on bonuses. These can range from $15,000 to over $100,000 and are often paid out in the first year of employment.
- Relocation Assistance: Often called a "relocation stipend," this is a payment (e.g., $10,000 to $20,000) to help a new physician move to the area.
- Quality & Performance Bonuses: As healthcare shifts toward value-based care, some compensation is tied to quality metrics, such as patient satisfaction scores, adherence to clinical guidelines (e.g., cancer screening rates), and positive patient outcomes.
- Retirement Benefits: This typically includes a 401(k) or 403(b) plan with an employer match. This is a vital part of long-term wealth building.
- Malpractice Insurance: The employer almost always covers the full cost of medical malpractice insurance, which can be a massive expense ($10,000 to over $100,000 per year depending on specialty and state).
- Continuing Medical Education (CME) Stipend: Physicians are required to complete a certain number of hours of continuing education each year to maintain their license. Employers provide an annual allowance (typically $3,000 - $7,500) to cover the cost of conferences, courses, and materials.
- Health and Disability Insurance: Comprehensive health, dental, vision, life, and long-term disability insurance are standard parts of the benefits package.
When considering a job offer, it's crucial to look at the *total value* of the package, not just the base salary. A lower base salary with a strong production bonus model and excellent benefits can often be more lucrative than a higher base salary with no upside potential.
---
Key Factors That Influence a DO's Salary
While the national averages provide a useful benchmark, a DO's actual salary is determined by a complex interplay of several powerful factors. This is where you can strategically plan your career to maximize your earning potential.
###
Area of Specialization: The Single Biggest Driver of Income
Without question, your choice of medical specialty is the most significant factor influencing your salary. The demand, length and competitiveness of training, and the nature of the procedures performed create a vast income disparity between different fields. DOs have access to every specialty, and their compensation within those fields is identical to that of MDs.
The Medscape Physician Compensation Report 2024 provides a clear hierarchy of earnings.
Top-Earning Specialties (Average Annual Compensation):
1. Orthopedics: $558,000
2. Plastic Surgery: $536,000
3. Cardiology: $525,000
4. Urology: $515,000
5. Gastroenterology: $512,000
6. Otolaryngology (ENT): $497,000
7. Radiology: $491,000
8. Oncology: $477,000
9. Anesthesiology: $472,000
10. Dermatology: $454,000
Lower-Earning (though still high-income) Specialties (Average Annual Compensation):
1. Public Health & Preventive Medicine: $254,000
2. Pediatrics: $258,000
3. Family Medicine: $270,000
4. Internal Medicine: $282,000
5. Diabetes & Endocrinology: $282,000
6. Infectious Disease: $286,000
7. Psychiatry: $321,000
8. Neurology: $322,000
As the data shows, procedural and surgical specialties that require longer training (e.g., a 5-year orthopedic surgery residency followed by a 1-year fellowship) command salaries that are often double that of primary care fields.
###
Geographic Location: Where You Practice Matters
Physician supply and demand dynamics create significant salary variations across different states and between urban, suburban, and rural areas. Often, areas that are less "desirable" to live in must offer higher compensation to attract physicians. Conversely, highly desirable major metropolitan areas may have a surplus of doctors, which can suppress salaries.
Top-Paying States for Physicians:
According to the Doximity 2023 Physician Compensation Report, the states with the highest average compensation are:
1. Oklahoma: $423,546
2. Tennessee: $416,134
3. Alabama: $414,978
4. Missouri: $411,465
5. Indiana: $407,575
Lowest-Paying States for Physicians:
1. Maryland: $341,940
2. District of Columbia: $343,767
3. Massachusetts: $351,668
4. New Mexico: $352,246
5. Delaware: $353,249
It's crucial to balance this data with the cost of living. A $400,000 salary in rural Indiana may provide a higher quality of life than a $350,000 salary in Boston or Washington D.C.
The Urban vs. Rural Dynamic:
A consistent trend is that physicians in rural communities earn more than their urban counterparts. A report from Merritt Hawkins noted that recruiting incentives are often higher in smaller communities. Why? Because the need is greater and the physician pool is smaller. A DO willing to practice in a rural or underserved area can often secure a higher starting salary, significant student loan repayment assistance (from federal or state programs), and a lower cost of living.
###
Practice Setting and Employment Type: Who Signs Your Paycheck?
The structure of your employment has a profound impact on both your salary and your work-life balance.
- Private Practice (Physician-Owned): This model offers the highest long-term earning potential. As a partner or owner, you not only earn a clinical salary but also share in the profits of the practice. The Medscape report shows that self-employed physicians (including practice owners and partners) earn an average of $402,000, compared to $351,000 for employed physicians. However, this comes with the responsibilities of running a business: managing staff, billing, overhead, and marketing.
- Hospital or Health System Employee: This is the most common employment model today. It offers stability, a predictable salary (often with production bonuses), and excellent benefits without the administrative headaches of running a practice. This is an attractive option for many DOs who want to focus purely on patient care.
- Academic Medical Center: Working for a university-affiliated hospital involves a three-part mission: clinical care, teaching medical students and residents, and research. Compensation in academia is typically lower than in private practice. However, it offers other rewards: intellectual stimulation, the prestige of a faculty appointment, and the fulfillment of training the next generation of doctors.
- Government Employment: DOs working for government entities like the Department of Veterans Affairs (VA), the military, or the Public Health Service often have lower top-end salaries. However, they receive exceptional benefits, including generous retirement pensions, excellent job security, and a more predictable work schedule with less call duty.
- Locum Tenens: This means "to hold the place of." Locum tenens physicians are independent contractors who take on temporary assignments (from a few days to several months) to fill in for other doctors. This path offers incredible flexibility and often very high daily or weekly pay rates, but it doesn't include benefits like health insurance or retirement plans.
###
Years of Experience and Career Trajectory
As detailed in the previous section, experience is a significant factor, but it functions differently than in many other professions. The initial jump in salary after residency is the most dramatic leap of a DO's career. From there, growth is more incremental and often tied to productivity.
An experienced DO is generally more efficient. They can diagnose conditions more quickly, perform procedures with greater speed and precision, and manage a larger patient panel. In a compensation model with an RVU component, this increased efficiency translates directly into higher income. Furthermore, with experience comes reputation. A well-regarded specialist will receive more referrals, keeping their schedule full and their productivity high. Senior physicians also have more opportunities to move into lucrative administrative leadership roles, such as a Department Chair or Chief Medical Officer (CMO), which often come with executive-level compensation packages.
###
In-Demand Skills and Procedural Abilities
Beyond the choice of specialty, proficiency in specific skills and procedures can further enhance a DO's value and income.
- Advanced Procedural Skills: A gastroenterologist who is skilled in advanced endoscopic procedures like ERCP (Endoscopic Retrograde Cholangiopancreatography) will earn more than one who only performs routine colonoscopies. Similarly, an orthopedic surgeon with fellowship training in a high-demand area like spine surgery or hip replacement will command a higher salary.
- Osteopathic Manipulative Treatment (OMT): For DOs in primary care, pain management, or physical medicine, building a practice with a strong OMT focus can be a significant differentiator. It can attract patients seeking non-pharmacological, non-surgical solutions, creating a dedicated patient base and a valuable niche in the market.
- Telehealth Proficiency: The COVID-19 pandemic accelerated the adoption of telehealth. Physicians who are comfortable and efficient with virtual consultations can increase their patient volume and accessibility, which can positively impact their income, particularly in RVU-based systems.
- Leadership and Administrative Skills: DOs who develop skills in management, finance, and operations can transition into leadership roles. A Medical Director of a large clinic or a hospital CMO is responsible for quality oversight, physician management, and strategic planning, and is compensated accordingly.
###
Level of Education and Advanced Training
For physicians, "education" is synonymous with "training." The baseline is the four-year Doctor of Osteopathic Medicine degree. The critical differentiators that dictate salary are the subsequent training steps:
- Residency: The length and field of residency are paramount. A 3-year Family Medicine residency leads to a primary care salary, while a 5-year General Surgery residency followed by a 3-year Cardiothoracic Surgery fellowship leads to a top-tier surgeon's salary.
- Fellowship: This is post-residency training to sub-specialize. For example, after a 3-year Internal Medicine residency, a DO can pursue a 3-year fellowship in Cardiology. This act of sub-specializing is what elevates their earning potential from an internist's salary (~$282,000) to a cardiologist's salary (~$525,000). Completing a competitive fellowship is the primary pathway to entering the highest-paid fields in medicine.
---
Job Outlook and Career Growth

The career outlook for Doctors of Osteopathic Medicine is exceptionally strong. The demand for physicians in the United States continues to outpace supply, ensuring robust job security and high earning potential for the foreseeable future.
The U.S. Bureau of Labor Statistics (BLS) projects that overall employment for physicians and surgeons will grow by 3 percent from 2022 to 2032. While this may seem modest, it's important to understand the context. This percentage translates to approximately 23,800 job openings for physicians and surgeons projected each year, on average, over the decade. Most of those openings are expected to result from the need to replace workers who transfer to different occupations or exit the labor force, such as to retire.
Several key trends are driving this sustained demand:
- An Aging Population: The large baby-boomer generation is aging, leading to increased demand for medical services, particularly for chronic conditions like heart disease, diabetes, and cancer.
- Growth in Primary Care: There is a recognized national shortage of primary care physicians. As the healthcare system increasingly emphasizes preventive care and management of chronic illness, the demand for family physicians, internists, and pediatricians will remain high. This is a significant advantage for the osteopathic profession, as a majority of DOs choose to enter these fields.
- Physician Retirement: A significant portion of the current physician workforce is nearing retirement age, which will create a wave of job openings that will need to be filled by new graduates.
- Increased Recognition of Osteopathic Medicine: The osteopathic profession is the fastest-growing medical field in the U.S. According to the American Osteopathic Association (AOA), the number of DOs has grown nearly 63% in the last decade. This growth reflects the increasing public demand for holistic, patient-centered care and the full integration of DOs into the mainstream medical establishment. The single accreditation system for graduate medical education (residency) has further unified the training pathways for MDs and DOs, solidifying their equal standing.
### Future Challenges and Staying Relevant
Despite the bright outlook, the profession is not without its challenges. Aspiring and practicing DOs should be aware of:
- Physician Burnout: High workloads, administrative burdens from EHRs, and insurance paperwork contribute to significant rates of burnout across all medical specialties. Maintaining a healthy work-life balance is a critical, ongoing challenge.
- Changes in Healthcare Policy: The healthcare landscape is in constant flux. Changes in insurance reimbursement, government regulations, and care delivery models can impact practice patterns and compensation.
- The Rise of AI and Technology: Artificial intelligence will likely play a growing role in diagnostics and data analysis. Physicians who embrace new technologies and learn to integrate them into their practice will be best positioned for future success.
### Advice for Career Advancement
A career in osteopathic medicine offers numerous avenues for growth beyond standard clinical practice. To advance in the field and ensure long-term career satisfaction, a DO should consider:
1. Pursuing Leadership Roles: Volunteer for committees at your hospital
