Introduction

Imagine a career where cutting-edge science, profound compassion, and unwavering resilience converge every single day. A role where you are the first line of defense, the primary caregiver, and a beacon of hope for the most vulnerable patients imaginable: newborns fighting for their first breaths, their first heartbeats, their first chance at life. This is the world of the neonatal nurse. For those called to this incredibly demanding yet deeply rewarding profession, California offers not only a dynamic and challenging environment but also one of the most lucrative compensation packages in the nation. The potential for a high neonatal nurse salary in California reflects the immense skill, dedication, and emotional fortitude required for the role, with earnings often reaching well into the six-figure range.
I once had the opportunity to shadow a team in a Level IV Neonatal Intensive Care Unit (NICU). The quiet hum of ventilators and monitors was a stark contrast to the intense, focused energy of the nurses, who moved with a calm precision that was both humbling and awe-inspiring. In that environment, I saw firsthand that this career is far more than a job; it is a sacred trust placed in the hands of a highly specialized few.
This guide is designed to be your definitive resource, whether you are a student contemplating a nursing career, a Registered Nurse (RN) considering a specialization, or a seasoned professional looking to advance. We will dissect every component of a neonatal nurse's salary in California, explore the factors that drive compensation, map out your career trajectory, and provide a clear, step-by-step plan to help you enter and thrive in this exceptional field.
### Table of Contents
- [What Does a Neonatal Nurse in California Do?](#what-is-a-neonatal-nurse)
- [Average Neonatal Nurse Salary in California: A Deep Dive](#salary-deep-dive)
- [Key Factors That Influence Your Salary](#key-factors)
- [Job Outlook and Career Growth for Neonatal Nurses](#job-outlook)
- [How to Become a Neonatal Nurse in California](#how-to-start)
- [Conclusion: Is a Neonatal Nursing Career in California Right for You?](#conclusion)
---
What Does a Neonatal Nurse in California Do?

A neonatal nurse is a Registered Nurse (RN) who specializes in the care of newborn infants experiencing a range of health challenges. These can include prematurity, birth defects, infection, cardiac malformations, and surgical problems. The term "neonatal" refers to the first 28 days of life, but neonatal nurses often care for infants for weeks or even months until they are healthy enough to go home.
Their work primarily takes place in a hospital's Neonatal Intensive Care Unit (NICU), which is categorized into different levels of care based on the acuity of the infants they serve. Understanding these levels is key to understanding the scope of the role:
- Level I (Well Newborn Nursery): Cares for healthy, full-term newborns. While some RNs work here, the term "neonatal nurse" typically implies care for at-risk infants.
- Level II (Special Care Nursery): Cares for infants born moderately preterm (32 weeks gestation or later) or those with less severe health issues who are expected to resolve them quickly. These babies may need help with feeding, temperature regulation, or require specialized medication.
- Level III (Neonatal Intensive Care Unit - NICU): Cares for infants born at less than 32 weeks gestation, as well as infants of all gestational ages with critical illnesses. These NICUs have a full range of respiratory support (including high-frequency ventilation) and can provide advanced life support. The majority of neonatal nurses work in Level III environments.
- Level IV (Regional NICU): These units provide the highest, most acute level of neonatal care. They are typically located in large, academic medical centers and have the capability to perform complex neonatal surgeries on-site (e.g., heart surgery). They care for the most complex and critically ill infants.
Core Responsibilities and Daily Tasks:
The duties of a neonatal nurse are multifaceted, blending highly technical skills with deep compassion and communication.
- Continuous Monitoring and Assessment: Constantly assessing vital signs (heart rate, respiratory rate, blood pressure, temperature), oxygen saturation, and neurological status.
- Life Support Management: Managing ventilators, incubators (isolettes), and other sophisticated medical equipment designed to support fragile infants.
- Medication and Fluid Administration: Calculating and administering precise dosages of medications, IV fluids, and parenteral nutrition. A small miscalculation can have significant consequences for a one-kilogram infant.
- Feeding and Nutrition: Assisting with feeding, which can range from gavage (tube) feeding to helping mothers with breastfeeding or bottle-feeding as the infant grows stronger.
- Developmental Care: Implementing strategies to minimize stress and promote healthy brain development in a high-tech environment. This includes managing light and sound levels, providing "kangaroo care" (skin-to-skin contact), and proper positioning.
- Family Support and Education: This is a cornerstone of the role. Neonatal nurses are the primary point of contact for terrified, exhausted parents. They explain complex medical information in understandable terms, provide emotional support, celebrate small victories, and teach parents how to care for their baby, preparing them for the eventual transition home.
- Collaboration: Working closely with a multidisciplinary team that includes neonatologists, respiratory therapists, pharmacists, social workers, and lactation consultants.
> ### A Day in the Life of a NICU Nurse (7 PM - 7 AM Shift)
>
> * 7:00 PM - Shift Handoff: You arrive and receive a detailed report from the day-shift nurse on your assigned patients—typically one to three infants, depending on acuity. You review their charts, lab results, and the plan for the night.
> * 8:00 PM - Initial Assessments: You perform a head-to-toe assessment on each baby, checking every line and tube, listening to their heart and lungs, and documenting everything meticulously. You check ventilator settings and IV pump rates.
> * 9:00 PM - Medication and Feeding: You administer scheduled medications. One of your babies is due for a gavage feeding of fortified breast milk, which you deliver slowly and carefully while monitoring for any signs of distress.
> * 11:00 PM - Family Interaction: The parents of your most critical infant arrive after work. You provide them with an update, answer their questions, and encourage them to touch and speak to their baby through the isolette portholes. You offer comfort and reassurance during a difficult time.
> * 1:00 AM - A Sudden Change: An alarm sounds. Your smallest patient, born at 25 weeks, is having apneic spells (pauses in breathing). You immediately provide stimulation, and when that's not enough, you use a bag-valve mask to provide breaths while calling the neonatologist and respiratory therapist for support.
> * 3:00 AM - Documentation and Rounds: The crisis has passed. You spend the next hour charting every detail of the event and your interventions. You prepare for "middle of the night" rounds with the on-call physician.
> * 5:00 AM - Lab Draws and Final Tasks: You perform a scheduled heel-stick to draw blood for lab tests. You tidy your area, restock supplies, and prepare the infants for their morning care routine.
> * 6:45 AM - Preparing Report: You organize your thoughts and data from the past 12 hours to give a clear, concise, and thorough report to the incoming day-shift nurse.
> * 7:15 AM - Heading Home: You leave the unit, emotionally and physically drained but knowing you made a difference in the most critical hours of a tiny life.
---
Average Neonatal Nurse Salary in California: A Deep Dive
California is consistently ranked as one of the highest-paying states for Registered Nurses, and this trend holds true—and is often amplified—for specialized roles like neonatal nursing. The high cost of living, strong nursing unions, and intense demand for highly skilled professionals all contribute to a robust salary landscape.
While the U.S. Bureau of Labor Statistics (BLS) provides excellent data for Registered Nurses as a broad category, specific neonatal nurse salary data is best aggregated from sources like Salary.com, Glassdoor, and Payscale, which analyze real-world job postings and self-reported data.
### National vs. California Averages
To appreciate the California advantage, it's essential to first look at the national picture.
- National Average for Registered Nurses: According to the BLS Occupational Employment and Wage Statistics, the median annual wage for all registered nurses in the United States was $86,070 as of May 2023. The lowest 10 percent earned less than $63,720, and the highest 10 percent earned more than $132,680.
- National Average for Neonatal Nurses: Salary aggregators suggest that neonatal nurses, due to their specialization, typically earn more than the general RN median. Payscale reports a national average base salary for a Neonatal Intensive Care Unit (NICU) Nurse of approximately $83,600 per year, with a typical range falling between $64,000 and $115,000.
Now, let's turn our focus to the Golden State.
- California Average for Registered Nurses: The BLS data for May 2023 shows California as the highest-paying state for RNs, with an annual mean wage of $137,690.
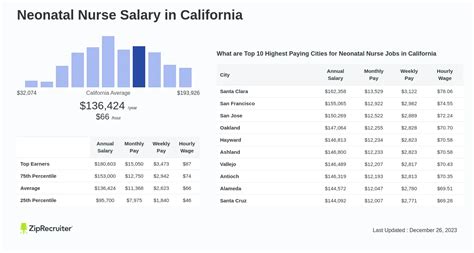
- Average Neonatal Nurse Salary in California: When we drill down to the neonatal specialty within California, the numbers are even more impressive.
- According to Salary.com (as of late 2023), the average Neonatal Nurse salary in California is $123,028, with a typical salary range falling between $111,811 and $138,061.
- Glassdoor (as of late 2023) reports a similar figure, estimating the total pay for a Neonatal Nurse in California to be around $143,500 per year, with an average base salary of approximately $128,000.
- Indeed's aggregated data suggests an average base salary of $135,115 per year for NICU nurses in California.
It's crucial to understand that these are averages. An entry-level nurse in a lower-cost-of-living area of California will earn less than a senior nurse with advanced certifications in the San Francisco Bay Area.
### Salary by Experience Level in California
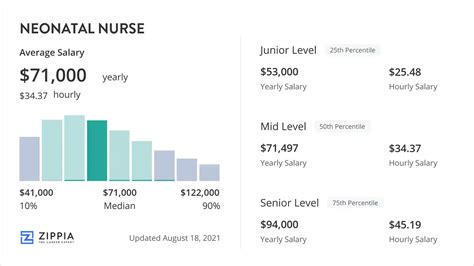
Salary progression in nursing is closely tied to experience. As a neonatal nurse gains clinical expertise, confidence, and potentially leadership skills, their earning potential increases significantly.
| Experience Level | Typical Years of Experience | Estimated Annual Salary Range (California) | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level Neonatal Nurse | 0-2 Years | $95,000 - $115,000 | New graduate or RN with recent transition to NICU. Focus on core competencies and clinical skills development. |
| Mid-Career Neonatal Nurse | 3-9 Years | $115,000 - $140,000 | Proficient and confident in caring for complex patients. May act as a preceptor for new nurses or take on charge nurse duties. Likely holds at least one certification. |
| Senior/Expert Neonatal Nurse | 10+ Years | $135,000 - $165,000+ | Highly experienced, often seen as a clinical leader. Manages the most critical patients, mentors entire teams, and may be involved in unit policy or research. |
| Neonatal Nurse Practitioner (NNP) | Master's or Doctorate | $160,000 - $220,000+ | Advanced practice role. Manages a caseload of patients, performs procedures, prescribes medications, and functions with a high degree of autonomy under physician supervision. |
*Source: Synthesized from Salary.com, Glassdoor, and Payscale data for California, cross-referenced with job postings from major California hospital systems.*
### Beyond the Base Salary: The Total Compensation Package
The annual salary figure is only one part of the equation. In a field like nursing, where shifts are long and often outside the standard 9-to-5, other forms of compensation can dramatically increase total earnings and overall job satisfaction.
- Shift Differentials: Nurses who work evenings, nights, or weekends receive a pay differential, which can add a significant amount to their hourly rate. Night shift differentials in California can range from an extra $5 to $15+ per hour.
- Overtime Pay: Working beyond a standard shift (typically 8 or 12 hours) or over 40 hours a week results in overtime pay, calculated at 1.5 times the base hourly rate. Given the nature of hospital staffing, opportunities for overtime are common.
- On-Call Pay: Some roles may require being "on-call," for which the nurse receives a small hourly stipend. If called in to work, they are then paid their full hourly rate (often with a minimum number of hours guaranteed).
- Sign-On Bonuses: To attract talent in a competitive market, many California hospitals offer substantial sign-on bonuses, sometimes ranging from $10,000 to $30,000 or more, especially for experienced NICU nurses.
- Clinical Ladder Programs: Many hospitals have a "clinical ladder" system that provides specific salary increases for nurses who achieve certain milestones, such as obtaining a certification (e.g., RNC-NIC), precepting new staff, or leading a quality improvement project.
- Benefits Package: The value of the benefits package cannot be overstated. This includes comprehensive health, dental, and vision insurance; a robust retirement plan (like a 401(k) or 403(b) with employer matching); paid time off (PTO); and tuition reimbursement, which is a massive asset for nurses looking to advance their education.
When considering a job offer, it's vital to analyze the entire compensation package, as a slightly lower base salary at a hospital with excellent benefits and differentials may be more valuable than a higher base salary with a weaker overall package.
---
Key Factors That Influence Your Salary
A six-figure salary is the norm, not the exception, for neonatal nurses in California. However, where you fall within that broad range—from just under $100,000 to well over $170,000 for a senior RN—depends on a combination of controllable and environmental factors. Mastering these elements is the key to maximizing your earning potential.
### Level of Education & Certification
Your educational foundation and specialized credentials are among the most powerful levers for influencing your salary.
- ADN vs. BSN: While you can become an RN with an Associate Degree in Nursing (ADN), the Bachelor of Science in Nursing (BSN) is increasingly the standard, particularly in California. Many major hospital systems, especially "Magnet" hospitals (a credential recognizing nursing excellence), exclusively hire BSN-prepared nurses or require ADN nurses to obtain their BSN within a specific timeframe. A BSN not only opens more doors but also typically places you on a higher pay scale from day one.
- MSN and DNP (The NNP Path): The most significant salary leap comes from advancing your practice. By earning a Master of Science in Nursing (MSN) or a Doctor of Nursing Practice (DNP) with a specialization as a Neonatal Nurse Practitioner (NNP), you transition from an RN role to that of a licensed independent practitioner. As an NNP, you take on a much higher level of responsibility, including diagnosing conditions, prescribing treatment, and performing advanced procedures like intubation and placing central lines. Consequently, the salary reflects this. As shown in the table above, NNPs in California can easily earn upwards of $180,000, with top earners exceeding $220,000.
- Professional Certifications: Certifications are the gold standard for validating your specialty-specific expertise. They demonstrate a commitment to your craft and a high level of knowledge. For neonatal nurses, the key certifications are:
- RNC-NIC® (Low Risk Neonatal Intensive Care Nursing): Offered by the National Certification Corporation (NCC), this is the cornerstone certification for NICU nurses. It requires a minimum of 2 years and 2,000 hours of specialty experience. Earning it almost always comes with a direct salary increase or bonus and makes you a much more competitive candidate.
- CCRN® (Neonatal): Offered by the American Association of Critical-Care Nurses (AACN), this certification is for nurses working with acutely or critically ill neonatal patients. It is another highly respected credential that signifies expertise in critical care.
- Developmental Care Specialist Designation: This credential shows expertise in creating a neuroprotective environment for fragile infants, a growing area of focus in NICUs.
Holding one or more of these certifications can add thousands of dollars to your annual salary through direct pay bumps or by qualifying you for higher levels on a hospital's clinical ladder.
### Years of Experience
Nowhere is the phrase "experience pays" truer than in neonatal nursing. The learning curve is steep, and the wisdom gained from managing countless crises and caring for hundreds of infants is invaluable.
- 0-2 Years (Novice to Advanced Beginner): In this stage, you are building fundamental skills and confidence. Your salary will be at the lower end of the spectrum for the role, but it will still be substantial by any national standard. Your focus is on learning, not earning potential.
- 3-9 Years (Competent to Proficient): By now, you are a reliable and skilled member of the team. You can handle complex cases with less supervision and begin to anticipate problems before they arise. This is where you will see significant salary growth. You can increase your value by becoming a preceptor (training new nurses) or a charge nurse (managing the unit's flow and staffing for a shift), both of which often come with a pay differential.
- 10+ Years (Expert): A senior neonatal nurse is a force multiplier on the unit. You are the go-to person for the toughest cases, the calm in the storm during a crisis, and a mentor to the entire team. Your salary will be at the top of the RN pay scale. Many nurses at this stage move into formal leadership (manager, educator) or advanced practice (NNP), but many also choose to remain at the bedside as expert clinicians, where their high salary reflects their immense value.
### Geographic Location (Within California)
California is a massive state with vastly different economic landscapes. The salary for a neonatal nurse in San Francisco will be significantly different from one in Fresno, primarily due to the dramatic differences in the cost of living and the concentration of high-paying medical centers.
| Metropolitan Area | Annual Mean Wage for All RNs (BLS, May 2023) | Estimated Neonatal Nurse Salary Range | Notes |
| :--- | :--- | :--- | :--- |
| San Francisco-Oakland-Hayward | $164,760 | $145,000 - $180,000+ | The highest-paying region in the state and country. Extremely high cost of living. Home to top-tier medical centers like UCSF and Stanford. |
| San Jose-Sunnyvale-Santa Clara | $159,630 | $140,000 - $175,000+ | "Silicon Valley" salaries extend to healthcare. Fierce competition for talent. Very high cost of living. |
| Sacramento-Roseville-Arden-Arcade | $145,500 | $130,000 - $160,000 | State capital with major hospital systems like UC Davis Health and Sutter. Strong pay with a slightly lower cost of living than the Bay Area. |
| Los Angeles-Long Beach-Anaheim | $133,900 | $120,000 - $150,000 | A massive, sprawling market with numerous hospitals (UCLA, Cedars-Sinai). Salaries are strong but highly variable between facilities. |
| San Diego-Carlsbad | $131,310 | $115,000 - $145,000 | A desirable location with strong demand. Home to Rady Children's Hospital and UCSD Health. |
| Riverside-San Bernardino-Ontario | $122,230 | $110,000 - $135,000 | "Inland Empire" salaries are lower than coastal cities, but so is the cost of living. A growing healthcare sector. |
| Bakersfield / Central Valley | $112,040 | $100,000 - $125,000 | The lowest salaries in the state, but this is directly offset by a significantly lower cost of living. Still very high by national standards. |
*Source: BLS Metropolitan and Nonmetropolitan Area Occupational Employment and Wage Estimates for Registered Nurses, May 2023. The estimated neonatal nurse ranges are extrapolations based on the premium for specialization.*
### Facility Type & Size
The type of hospital you work for plays a major role in your compensation and work environment.
- Large, Academic University Medical Centers (e.g., UCSF, UCLA, Stanford, UC Davis): These facilities typically offer the highest salaries. They are often unionized, have Level IV NICUs, and are at the forefront of research and treatment. The work is demanding, and the patient acuity is the highest, but the compensation reflects this.
- Large, Private Non-Profit Hospital Systems (e.g., Kaiser Permanente, Sutter Health, Dignity Health): These systems are highly competitive with university hospitals in terms of pay and benefits. Kaiser, in particular, is known for its exceptional compensation packages for nurses throughout California.
- County/Public Hospitals: These hospitals are a vital part of the state's healthcare safety net. While their base pay may sometimes be slightly lower than top private hospitals, they often have very strong union contracts, excellent pension plans, and great job security.
- For-Profit Hospitals: Pay scales can be more variable in the for-profit sector. While some are competitive, others may offer lower base salaries or less robust benefits packages.
- Children's Hospitals (e.g., Children's Hospital Los Angeles, Rady Children's): These specialty hospitals are hubs of pediatric and neonatal care. They offer a unique, focused environment and competitive salaries to attract top neonatal talent.
### NICU Level of Care & High-Value Skills
While "neonatal nursing" is the specialization, further sub-specialization within the NICU can impact your role and value. Working in a higher-acuity setting like a Level IV NICU often requires a higher level of skill and experience, which in turn commands better pay or requires the experience needed to be in a higher salary bracket.
Furthermore, developing specific high-value skills can make you an indispensable member of the team and justify a higher salary or position you for promotion.
- Clinical Skills:
- ECMO (Extracorporeal Membrane Oxygenation): Being a certified ECMO specialist, managing the heart-lung bypass machine for the sickest infants, is a highly advanced and sought-after skill.
- Ventilator Management: Deep knowledge of various modes of ventilation, from conventional to high-frequency oscillation.
- Transport Nursing: Being part of a neonatal transport team that stabilizes and transports critically ill infants from other hospitals to a higher level of care.
- PICC Line Skills: Being certified to insert peripherally inserted central catheters.
- Soft & Leadership Skills:
- Crisis Management: The proven ability to remain calm and lead during a sudden patient decline.
- Family-Centered Communication: Exceptional skill in counseling and educating distressed families.
- Precepting & Mentoring: A passion for teaching and developing new nurses.
- Charge Nurse Experience: Demonstrating leadership, delegation, and problem-solving skills for an entire unit.
---
Job Outlook and Career Growth for Neonatal Nurses

For those investing the time and effort to enter this challenging field, the career outlook is exceptionally positive, offering long-term stability and numerous avenues for professional advancement.
### Job Growth and Demand
The U.S. Bureau of Labor Statistics