For those drawn to a career that blends profound human impact with high-level medical skill, few paths are as compelling as neonatal nursing. To be a Neonatal Intensive Care Unit (NICU) nurse is to be a guardian at the very beginning of life, providing critical care to the most vulnerable patients: premature and critically ill newborns. It's a role that demands immense knowledge, steady hands, and a compassionate heart. If you're considering this demanding yet deeply rewarding career in the Golden State, your first practical question is likely: "What is the typical NICU nurse salary in California?"
The answer is encouraging. California stands as the highest-paying state in the nation for registered nurses, and this premium extends robustly to specialized roles like NICU nursing. A qualified NICU nurse in California can expect to earn a salary that not only provides financial stability but also reflects the high level of expertise required. Average salaries regularly exceed $130,000, with top earners in high-demand areas pushing past the $180,000 mark.
Years ago, a close friend of mine spent three long months in the NICU with her son, who was born 14 weeks early. She often said that while the doctors were brilliant, it was the nurses—the ones who were there for 12-hour shifts, who taught her how to hold her impossibly tiny son, and who celebrated every gram of weight gained—that got her family through the ordeal. They were her son's caregivers, her educators, and her emotional anchors. This article is for anyone who aspires to be that anchor for another family.
This guide will serve as your definitive resource, breaking down every facet of a NICU nurse's salary in California. We will explore the data-backed numbers, the factors that drive your earning potential, and the precise steps you can take to enter and excel in this vital profession.
### Table of Contents
- [What Does a NICU Nurse in California Do?](#what-does-a-nicu-nurse-do)
- [Average NICU Nurse Salary in California: A Deep Dive](#average-salary-deep-dive)
- [Key Factors That Influence a NICU Nurse's Salary](#key-factors)
- [Job Outlook and Career Growth for NICU Nurses](#job-outlook)
- [How to Become a NICU Nurse in California](#how-to-get-started)
- [Conclusion: Is a NICU Nursing Career in California Right for You?](#conclusion)
What Does a NICU Nurse in California Do?

A NICU nurse is a registered nurse (RN) who has specialized in the care of newborn infants facing a range of health challenges. These can include prematurity, low birth weight, congenital disorders, cardiac malformations, infections, and respiratory distress. The NICU environment is a world of advanced technology and meticulous, moment-to-moment care, but at its heart, the role is about nurturing new life and supporting families during a time of intense stress and uncertainty.
The responsibilities of a NICU nurse are vast and varied, blending technical proficiency with compassionate caregiving. They operate within a structured hierarchy of care, typically in NICUs designated by level:
- Level II NICU (Special Care Nursery): Cares for infants born at or after 32 weeks' gestation or who are recovering from more serious conditions. Nurses here manage feeding issues, breathing support like nasal cannula oxygen, and thermoregulation.
- Level III NICU (Neonatal Intensive Care Unit): Cares for infants born before 32 weeks, critically ill newborns, or those needing advanced respiratory support like high-frequency ventilation or surgery. Nurses here manage complex equipment, life-sustaining medications, and critical interventions.
- Level IV NICU (Regional Neonatal Intensive Care Unit): The highest level of care. These units are typically in major academic medical centers and can provide the most complex care, including advanced surgical procedures like open-heart surgery and extracorporeal membrane oxygenation (ECMO), a form of heart-lung bypass.
Core Responsibilities and Daily Tasks:
- Continuous Monitoring: Closely observing vital signs, including heart rate, respiratory rate, blood pressure, and oxygen saturation, using sophisticated monitoring equipment.
- Administering Medications and Treatments: Calculating and administering precise dosages of medications, including intravenous (IV) drugs and antibiotics.
- Managing Life-Support Systems: Operating and troubleshooting equipment such as ventilators, incubators (isolettes), IV pumps, and feeding tubes.
- Performing Procedures: Assisting physicians with or independently performing procedures like placing IV lines, drawing blood, and providing respiratory suctioning.
- Feeding and Nutrition Management: Administering nutrition via IV (total parenteral nutrition, or TPN), gavage (tube) feeding, or assisting mothers with breastfeeding or bottle-feeding when the infant is stable enough.
- Developmental Care: Implementing strategies to protect the fragile developing brain of the infant. This includes minimizing stress from noise and light, promoting "kangaroo care" (skin-to-skin contact), and using specific positioning techniques.
- Family Education and Support: This is a cornerstone of the role. NICU nurses educate parents on their infant's condition, teach them how to participate in their baby's care, provide emotional support, and prepare them for a potential long-term stay and eventual discharge.
- Collaboration and Communication: Working as part of a large interdisciplinary team that includes neonatologists, respiratory therapists, pharmacists, social workers, and lactation consultants. Clear, precise communication during rounds and shift changes is critical.
### A Day in the Life of a NICU Nurse (Level III)
7:00 AM - Shift Handoff: You arrive and get a detailed report from the night-shift nurse on your assigned patients—perhaps a 26-week preemie on a ventilator and a 34-weeker with feeding difficulties. You review their charts, lab results, and overnight events.
8:00 AM - First Assessment: You perform a meticulous head-to-toe assessment on each baby, checking every system, evaluating their breathing, listening to their heart and lungs, and assessing their neurological status. You document everything precisely.
9:30 AM - Rounds with the Medical Team: The neonatologist, resident, pharmacist, and respiratory therapist come by. You present your patient's status, discuss the plan for the day, and advocate for any changes you believe are necessary based on your close observation.
11:00 AM - Medications and Feedings: You carefully draw and administer multiple IV medications. For the 34-weeker, you attempt a bottle feed, working on coordinating their suck-swallow-breathe pattern. The 26-weeker receives nutrition through their IV and a feeding tube.
1:00 PM - Family Time and Education: The parents of the 26-weeker arrive. You update them on the morning's progress and help them perform "kangaroo care," carefully transferring the tiny infant, with all their wires and tubes, onto the parent's chest. You answer their questions and reassure them.
3:00 PM - Charting and Care Plan Updates: You spend significant time documenting every intervention, assessment finding, and patient response. This legal and medical record is critical for continuity of care.
5:00 PM - Responding to an Unplanned Event: An alarm sounds. A different baby is having an apneic (breathing pause) episode. You rush to the bedside with another nurse to provide stimulation and, if needed, breathing support, stabilizing the infant quickly and efficiently.
6:30 PM - Preparing for Handoff: You ensure your patients are stable, all tasks are complete, and your charting is finalized. You prepare a thorough report for the incoming night-shift nurse, ensuring a safe and seamless transition of care.
7:00 PM - Shift End: You leave, emotionally and physically tired, but knowing your vigilance and expertise made a direct difference in the lives of your tiny patients and their families.
Average NICU Nurse Salary in California: A Deep Dive
California is renowned for its high cost of living, but it compensates its nursing professionals with the highest wages in the United States. This holds true for NICU nurses, whose specialized skills command a significant premium. While salary figures can vary based on the data source, they consistently paint a picture of lucrative financial opportunity.
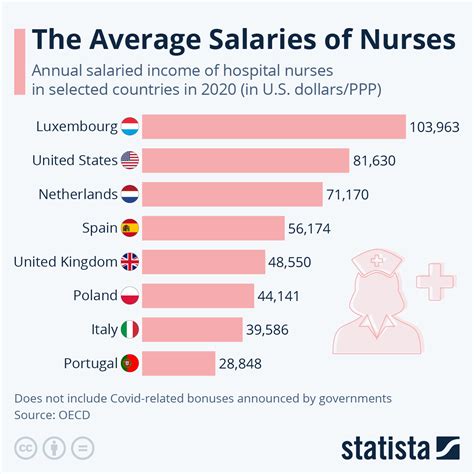
First, let's establish a baseline. According to the U.S. Bureau of Labor Statistics (BLS) Occupational Employment and Wage Statistics report from May 2023, the national average annual wage for all Registered Nurses was $94,480. However, California blows this number out of the water. The BLS reports the statewide annual mean wage for Registered Nurses in California is $137,690, making it the top-paying state in the country.
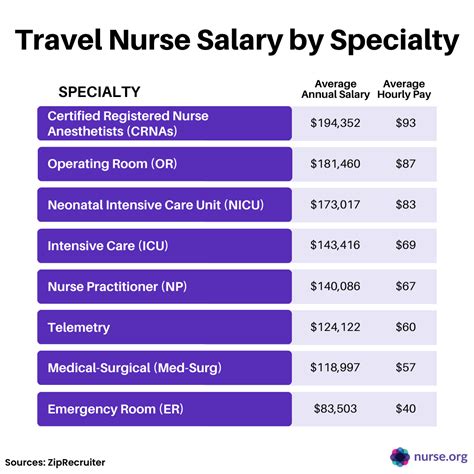
Specialized nurses, like those in the NICU, typically earn at or above this state average due to the increased complexity and stress of their role. Let's look at what major salary aggregators report for this specific career path in California.
California NICU Nurse Salary Averages (as of late 2023/early 2024):
- Salary.com: Reports the average Neonatal Nurse salary in California is $134,103, with a typical range falling between $122,236 and $146,086. This data often includes a robust set of employers and is highly specific to the job title.
- Indeed.com: Calculates the average base salary for a Neonatal Intensive Care Unit (NICU) RN in California to be approximately $142,670 per year. Indeed's data is compiled from a large pool of job postings and user-submitted information.
- Glassdoor.com: Estimates the total pay for a NICU RN in California to be around $131,529 per year, with a likely range between $111,000 and $157,000. "Total pay" often includes base salary plus additional compensation like bonuses.
- ZipRecruiter.com: States the average annual pay for a NICU Nurse in California is $130,495, with the majority of salaries ranging between $111,500 (25th percentile) and $149,000 (75th percentile). Top earners in the 90th percentile reach $168,500.
Consolidated Salary Snapshot for NICU Nurses in California:
| Source | Average Annual Salary | Typical Salary Range |
| :--- | :--- | :--- |
| U.S. BLS (All CA RNs) | $137,690 | N/A (Statewide Mean) |
| Salary.com | $134,103 | $122,236 - $146,086 |
| Indeed.com | $142,670 | Varies by job posting |
| Glassdoor.com | $131,529 | $111,000 - $157,000 |
| ZipRecruiter.com | $130,495 | $111,500 - $149,000 |
From this data, it's safe to conclude that a NICU nurse in California can reasonably expect a base salary in the $125,000 to $145,000 range, with significant potential to earn more based on the factors we'll discuss next.
### Salary Progression by Experience Level
Your salary as a NICU nurse is not static; it grows significantly with experience. As you accumulate skills, certifications, and a proven track record of handling complex cases, your value to an employer increases dramatically.
- Entry-Level NICU Nurse (0-2 Years): A nurse who has recently completed a new graduate residency program or transitioned into the NICU can expect to be at the lower end of the pay scale. However, "lower end" in California is still substantial.
- Estimated Salary Range: $95,000 - $120,000 per year.
- Hospitals often use a structured "clinical ladder" or step-based pay scale, so even in the first couple of years, you will see predictable annual raises.
- Mid-Career NICU Nurse (3-9 Years): This is where earning potential truly accelerates. A nurse with several years of direct NICU experience is a highly valuable asset. They can act as a preceptor (training new nurses), take on more complex patient assignments, and work with greater autonomy.
- Estimated Salary Range: $120,000 - $155,000 per year.
- Many nurses in this bracket will have obtained their primary specialty certification (RNC-NIC), which often comes with a pay differential.
- Senior/Experienced NICU Nurse (10+ Years): A nurse with a decade or more of experience is a unit expert. They often take on leadership roles like Charge Nurse, serve on hospital committees, and mentor entire teams. Their deep knowledge base makes them indispensable.
- Estimated Salary Range: $150,000 - $180,000+ per year.
- Top earners in this category are often working in high-cost, high-demand metropolitan areas, may have advanced degrees, and hold multiple certifications.
### Beyond the Base Salary: Understanding Total Compensation
Your annual salary is only one piece of the puzzle. Hospital compensation packages, especially in competitive markets like California, are often rich with additional financial benefits that can significantly boost your overall earnings and quality of life.
- Shift Differentials: This is a major component of a nurse's pay. Hospitals pay a premium for working undesirable hours.
- Evening/PM Shift: Can add $3 - $7+ per hour.
- Night/NOC Shift: Often the most lucrative, adding $8 - $20+ per hour. A full-time night shift nurse could easily add $16,000 - $40,000 to their annual income.
- Weekend Differential: An additional premium on top of the base and shift differential for working on Saturdays and Sundays.
- Overtime Pay: All hours worked over 8 in a day or 40 in a week are typically paid at 1.5 times the base hourly rate. In California, daily overtime rules are strict, benefiting the employee.
- On-Call Pay: Nurses on-call for a potential shift receive a small hourly stipend (e.g., $5-10/hour) just for being available. If called in, they are paid their full overtime rate, often with a minimum number of hours guaranteed.
- Charge Nurse/Preceptor Pay: Taking on the responsibility of leading a shift or training a new nurse almost always comes with an hourly pay differential.
- Sign-On Bonuses: To attract talent in a competitive market, hospitals frequently offer sign-on bonuses for experienced NICU nurses, which can range from $5,000 to $25,000 or more, often tied to a 2-3 year commitment.
- Clinical Ladder Bonuses/Raises: Many hospitals have a structured advancement program (e.g., Clinical Nurse I, II, III, IV). Moving up the ladder by completing projects, earning certifications, and demonstrating leadership results in a significant base pay increase.
- Benefits Package: The value of a strong benefits package cannot be overstated. This includes:
- Health Insurance: Comprehensive medical, dental, and vision plans.
- Retirement Savings: 401(k) or 403(b) plans, often with a generous employer match.
- Paid Time Off (PTO): A combined bank for vacation, sick days, and holidays.
- Tuition Reimbursement: Financial assistance for nurses pursuing higher education (e.g., a BSN or MSN degree).
When evaluating a job offer, it's crucial to look at the total compensation package, not just the hourly wage. A slightly lower base pay at a hospital with an exceptional night shift differential and a 5% retirement match might be financially superior to a higher base pay with minimal extras.
Key Factors That Influence a NICU Nurse's Salary in California
While the statewide averages provide a fantastic starting point, your individual salary as a NICU nurse in California will be determined by a specific and predictable set of factors. Understanding these variables empowers you to negotiate effectively and strategically guide your career toward maximum earning potential. This is the most critical section for anyone looking to optimize their income in this field.
### `
`1. Geographic Location within California`
`California is a massive and economically diverse state. Where you choose to work will have the single largest impact on your salary. The cost of living in San Francisco is vastly different from that in Fresno, and nursing salaries reflect this reality. The highest salaries are concentrated in the major metropolitan areas where demand is high and the cost of living is steepest.
Data from the BLS (May 2023) for Registered Nurses across California's metropolitan statistical areas (MSAs) provides a clear picture. Since NICU nurse pay tracks closely with general RN pay, these figures are an excellent proxy.
Top-Paying Metropolitan Areas for Nurses in California:
| Metropolitan Area | Annual Mean Wage (All RNs) | Approximate Hourly Mean Wage |
| :--- | :--- | :--- |
| San Jose-Sunnyvale-Santa Clara, CA | $161,560 | $77.67 |
| San Francisco-Oakland-Hayward, CA | $159,380 | $76.63 |
| Vallejo-Fairfield, CA | $152,730 | $73.43 |
| Sacramento-Roseville-Arden-Arcade, CA | $145,030 | $69.73 |
| Salinas, CA | $141,610 | $68.08 |
| Los Angeles-Long Beach-Anaheim, CA | $133,900 | $64.38 |
| San Diego-Carlsbad, CA | $127,110 | $61.11 |
Key Takeaways on Location:
- The Bay Area is King: The San Francisco Bay Area (including San Jose and Oakland) consistently offers the highest nursing salaries in the country, let alone the state. Competition for jobs at prestigious hospitals like UCSF Benioff Children's Hospitals, Stanford Children's Health, and Kaiser Permanente facilities is fierce, but the compensation is unparalleled.
- Sacramento is a Strong Contender: The state capital region offers a compelling balance of high salaries and a slightly lower cost of living compared to the Bay Area, making it an attractive location.
- Southern California is Vast and Varied: The massive Los Angeles metro area has a slightly lower average than Northern California, but still pays exceptionally well. Salaries can vary significantly between hospitals in Beverly Hills versus those in the Inland Empire (Riverside-San Bernardino). San Diego also offers strong, competitive wages.
- Central Valley and Rural Areas: Locations like Fresno, Bakersfield, and other parts of the Central Valley will have lower average salaries (though still high by national standards), but this is often offset by a significantly lower cost of living. For example, the BLS reports the average RN salary in the Fresno, CA MSA is $118,500.
### `
`2. Level of Education and Certification`
`Your educational qualifications are the foundation of your nursing practice and a direct driver of your salary. While you can become an RN with an Associate's Degree, the industry standard and the key to higher earnings is a Bachelor's degree and advanced certifications.
- ADN vs. BSN:
- Associate's Degree in Nursing (ADN): A two-year degree that qualifies you to take the NCLEX-RN exam. While it's the fastest path to becoming an RN, many major hospitals in California, especially Magnet® designated hospitals and university medical centers, have a strong preference or requirement for nurses to hold a Bachelor's degree. You may start at a lower pay step on the clinical ladder with an ADN.
- Bachelor of Science in Nursing (BSN): A four-year degree that is increasingly the standard for professional nursing. It provides a broader education in leadership, research, and community health. Holding a BSN is essential for career advancement and unlocks the door to higher-paying jobs, graduate studies, and leadership roles. A BSN-prepared nurse will almost always earn more than an ADN-prepared nurse in the same role.
- Master of Science in Nursing (MSN) and Doctoral Degrees (DNP/PhD):
- Pursuing a graduate degree opens up the highest echelons of neonatal nursing. An MSN can lead to roles like:
- Neonatal Nurse Practitioner (NNP): NNPs are advanced practice registered nurses (APRNs) who can diagnose conditions, prescribe medications, and manage patient care with a high degree of autonomy. NNPs in California routinely earn $150,000 to $220,000+.
- Clinical Nurse Specialist (CNS): A CNS is an expert in a specialty (like neonatology) who focuses on improving patient outcomes, mentoring staff, and driving evidence-based practice changes across a unit or hospital system. Their salaries are also well into the six-figure range, often comparable to senior-level staff nurses or nurse managers.
- A Doctor of Nursing Practice (DNP) or PhD in Nursing prepares you for top-tier leadership, academic, or research positions with commensurate salaries.
- Professional Certifications:
- Certifications are the single best way for a staff-level NICU nurse to increase their base pay and demonstrate expertise. They validate your specialized knowledge and skills.
- RNC-NIC (Registered Nurse Certified - Neonatal Intensive Care): This is the gold standard certification for NICU staff nurses, offered by the National Certification Corporation (NCC). Eligibility requires a minimum number of hours of direct practice in the specialty. Earning your RNC-NIC almost always comes with a significant hourly pay differential or an annual bonus and is a prerequisite for advancing up the clinical ladder.
- CCRN (Neonatal) (Critical Care Registered Nurse): Offered by the American Association of Critical-Care Nurses (AACN), this is another highly respected certification demonstrating expertise in caring for critically ill neonates. Some nurses hold both RNC-NIC and CCRN certifications.
- Other Certifications: Specialized certifications in areas like Electronic Fetal Monitoring (C-EFM) or transport nursing (C-NPT) can also add to your expertise and earning potential.
### `
`3. Facility Type and Size`
`The type of hospital you work for plays a crucial role in determining your salary and benefits package.
- Major University Medical Centers (e.g., UCLA Health, UCSF Health, Stanford Health Care): These are often the highest-paying employers. They are typically unionized, have large Level IV NICUs, and serve as regional referral centers for the most complex cases. They have structured, transparent pay scales and excellent benefits due to their size and prestige.
- Large Private, Non-Profit Hospital Systems (e.g., Kaiser Permanente, Sutter Health, Dignity Health): These systems are also top-tier employers. Kaiser Permanente, in particular, is famous for its high salaries and comprehensive benefits, often setting the benchmark for compensation in the regions it serves. These organizations have large, sophisticated NICUs and strong union representation.
- Government/County Hospitals: County-run facilities (e.g., LA County+USC Medical Center) serve as vital safety nets and often have very busy, high-acuity NICUs. Their pay is competitive and often union-negotiated, with excellent government pension and benefits plans that can be very attractive for long-term career stability.
- For-Profit Hospitals: While less common in some parts of California, these hospitals' pay can be competitive but may sometimes lag behind the major non-profit and university systems. It's essential to scrutinize their benefits packages and staffing ratios.
- Magnet® Designation: Hospitals that have achieved Magnet® recognition from the American Nurses Credentialing Center (ANCC) have demonstrated excellence in nursing. This status helps them attract top talent, and they often offer higher pay, better staffing, and a more positive work environment, all of which contribute to a NICU nurse's career satisfaction and compensation.
### `
`4. Area of Specialization (NICU Level) and In-Demand Skills`
`Even within the NICU specialty, your specific skill set and the acuity of the patients you care for can influence your pay and desirability as a candidate.
- NICU Level Experience: While pay scales may be the same for all nurses on a unit, those with proven experience in higher-acuity settings are more valuable and have more job mobility. A nurse comfortable managing a baby on ECMO in a Level IV NICU is a highly sought-after specialist. They are more likely to qualify for roles on transport teams or in rapid response, which may come with pay differentials.
- Charge Nurse Experience: Regularly taking on the role of Charge Nurse demonstrates leadership, problem-solving, and organizational skills. This experience is a prerequisite for management roles and comes with an hourly pay bump.
- Transport Team: Many large children's hospitals have dedicated neonatal/pediatric transport teams that travel by ambulance or helicopter to stabilize and retrieve critically ill infants from other facilities. These roles are highly competitive, require advanced skills (like intubation and managing care in a moving vehicle), and often come with a significant pay differential due to the level of autonomy and responsibility.
- ECMO Specialist: ECMO (Extracorporeal Membrane Oxygenation) is a highly complex form of life support. Nurses who are trained and certified as ECMO specialists are an elite group and are compensated accordingly for this high-risk, high-skill work.
- Precepting and Mentoring: Being a designated preceptor for new graduate nurses or new hires is a key role
