Are you seeking a career that masterfully blends deep medical expertise with compassionate, patient-centered care? Do you envision yourself as a leader in healthcare, diagnosing illnesses, prescribing treatments, and managing the overall well-being of your patients? If you're drawn to a profession with significant autonomy, immense personal fulfillment, and outstanding financial rewards, the role of a Nurse Practitioner (NP) may be your calling. This career is not just a job; it is a commitment to advancing healthcare, and it comes with a compensation package that reflects its critical importance. With a national median salary soaring well over the six-figure mark, becoming an NP is one of the most promising and lucrative paths in the medical field today.
I still vividly recall a conversation with a family member who was struggling with a complex, chronic autoimmune disease. For years, she felt like a number in a vast healthcare system, shuttled between specialists who rarely spoke to one another. Everything changed when a Nurse Practitioner took over her primary care. This NP didn't just manage medications; she coordinated care, listened intently to subtle symptoms, and empowered my relative with the knowledge to manage her own health. That blend of clinical authority and genuine human connection is the hallmark of an exceptional NP, and it’s a value that the healthcare industry is increasingly willing to pay a premium for.
This comprehensive guide is designed to be your definitive resource on the Nurse Practitioner salary. We will dissect every factor that influences your earning potential, from your educational choices to your geographic location and area of specialization. Whether you are a student considering this path, a registered nurse planning your next step, or a current NP looking to maximize your income, this article will provide the authoritative, data-driven insights you need to navigate your career with confidence.
### Table of Contents
- [What Does a Nurse Practitioner Do?](#what-does-a-nurse-practitioner-do)
- [Average Nurse Practitioner Salary: A Deep Dive](#average-nurse-practitioner-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion: Is a Nurse Practitioner Career Worth It?](#conclusion-is-a-nurse-practitioner-career-worth-it)
What Does a Nurse Practitioner Do?
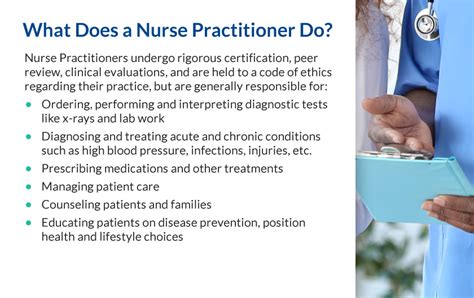
A Nurse Practitioner is an Advanced Practice Registered Nurse (APRN) who has completed advanced graduate-level education, either a Master of Science in Nursing (MSN) or a Doctor of Nursing Practice (DNP). This advanced training equips them with the expert knowledge and clinical competency to provide a wide range of healthcare services, often similar to those of a physician. NPs are trained to assess patients, order and interpret diagnostic tests, make diagnoses, and initiate and manage treatment plans—including prescribing medications.
The core of the NP role is a holistic, patient-centered model of care. While they possess profound medical knowledge, their nursing foundation emphasizes disease prevention, health education, and health promotion. They work to empower patients to be active participants in their health and well-being.
The scope of an NP's practice can vary significantly from state to state, which is a critical concept for any aspiring NP to understand. States are generally categorized into three levels of practice authority:
1. Full Practice Authority: In these states, NPs are permitted to evaluate patients, diagnose, order and interpret tests, and initiate and manage treatments under the exclusive licensure authority of the state board of nursing. This is the highest level of autonomy and allows NPs to establish their own independent practices.
2. Reduced Practice Authority: In these states, NPs are required to have a regulated collaborative agreement with a physician to provide patient care, or limits are placed on the setting or scope of one or more elements of NP practice.
3. Restricted Practice Authority: These states require career-long supervision, delegation, or team management by a physician in order for the NP to provide patient care.
Core responsibilities and daily tasks often include:
- Performing comprehensive physical examinations and health histories.
- Diagnosing and treating acute and chronic conditions, such as diabetes, high blood pressure, infections, and injuries.
- Ordering, performing, and interpreting diagnostic studies like lab work and X-rays.
- Prescribing medications and other treatments.
- Managing patients' overall care and serving as their primary healthcare provider.
- Counseling and educating patients on disease prevention, healthy lifestyles, and managing chronic conditions.
- Performing minor procedures, such as suturing, biopsies, and joint injections (depending on specialty and training).
### A Day in the Life of a Family Nurse Practitioner
To make the role more tangible, let's walk through a typical day for a Family Nurse Practitioner (FNP) working in an outpatient primary care clinic.
- 8:00 AM - 8:30 AM: The day begins by reviewing the schedule and patient charts. The FNP looks over lab results that came in overnight, flags any that require immediate follow-up, and prepares for the first few appointments, noting key concerns or necessary health maintenance screenings.
- 8:30 AM - 12:00 PM: Patient appointments begin. The morning is a mix of cases: a 45-year-old for an annual wellness exam, a child with an ear infection, a 65-year-old for a follow-up on their hypertension management, and a walk-in patient with a persistent cough. For each patient, the FNP performs an exam, discusses symptoms, formulates a diagnosis, develops a treatment plan (which may include new prescriptions or referrals), and thoroughly documents the encounter in the Electronic Health Record (EHR).
- 12:00 PM - 1:00 PM: Lunch break, which often doubles as administrative time. The FNP catches up on phone calls to patients, consults with a specialist about a complex case, and reviews and signs prescription refill requests.
- 1:00 PM - 4:30 PM: The afternoon brings another round of diverse patient cases. This could include a teenager's sports physical, a mental health check-in for a patient with anxiety, management of a diabetic patient's blood sugar levels, and a minor procedure like removing stitches.
- 4:30 PM - 5:30 PM: Patient appointments are finished, but the workday is not. This final hour is dedicated to "chart closure"—finishing all clinical notes from the day, sending referrals, responding to patient messages through the online portal, and ensuring all orders have been placed correctly. This administrative work is crucial for continuity of care and proper billing.
This example highlights the dynamic, challenging, and deeply rewarding nature of the NP role, which requires a blend of sharp clinical judgment, efficiency, and profound empathy.
Average Nurse Practitioner Salary: A Deep Dive

The financial compensation for Nurse Practitioners is one of the most compelling aspects of the career, reflecting the high level of responsibility and expertise the role demands. Salaries are consistently robust across the nation, making it a financially secure and rewarding profession.
According to the most recent data from the U.S. Bureau of Labor Statistics (BLS) Occupational Outlook Handbook, the median annual wage for nurse practitioners was $128,490 as of May 2023. This "median" figure means that half of all NPs earned more than this amount, and half earned less.
However, the median only tells part of the story. The full salary spectrum for NPs is quite broad, influenced by a multitude of factors we will explore in the next section. The BLS data from May 2023 also provides a look at the typical salary range:
- Lowest 10% earned less than $94,930. This often represents entry-level positions, roles in lower-paying geographic areas, or certain non-profit settings.
- Highest 10% earned more than $168,030. These top earners are typically highly experienced NPs, those in high-demand specialties, individuals in leadership positions, or those working in high-paying states or metropolitan areas.
Salary aggregator websites provide further granularity and slightly different figures based on their proprietary data models, but they all paint a similar picture of a strong six-figure profession.
- Salary.com, as of late 2023, reports the average Nurse Practitioner salary in the United States to be $127,113, with a typical range falling between $117,965 and $137,959.
- Payscale.com indicates a similar average base salary of around $112,000, but also highlights the significant impact of experience on earnings over time.
- The American Association of Nurse Practitioners (AANP) conducts a comprehensive national survey, which is a gold-standard resource. Their 2020 survey (the most recent publicly detailed) reported a median total income of $117,000 for full-time NPs, which includes base salary plus any bonuses. This number has undoubtedly risen in the years since, aligning more closely with current BLS data.
### NP Salary by Experience Level
One of the most predictable drivers of salary growth is experience. As NPs gain more clinical confidence, autonomy, and efficiency, their value to an employer increases significantly. Here is a general breakdown of what you can expect at different stages of your career, compiled from aggregator data and industry trends:
| Experience Level | Typical Base Salary Range (Annual) | Key Characteristics |
| :--- | :--- | :--- |
| Entry-Level (0-2 Years) | $105,000 - $118,000 | New graduates, often require more mentorship. Focus is on building clinical confidence and efficiency. May receive lower initial productivity bonuses. |
| Mid-Career (3-9 Years) | $119,000 - $135,000 | Fully autonomous and highly efficient. Manages complex patient loads. Often begins to take on roles like precepting students or leading clinic initiatives. |
| Senior/Experienced (10+ Years) | $136,000 - $155,000+ | A clinical expert in their field. May have sub-specialty knowledge. Often holds leadership roles (e.g., Lead NP, Clinic Director) or has a highly productive patient panel. |
| Late Career (20+ Years) | $140,000 - $170,000+ | Top of the earning potential. Often in administrative, academic, or specialized high-acuity roles. May own their own practice. |
*Note: These are national averages and can be significantly higher or lower based on the factors discussed in the next section.*
### Beyond the Base Salary: Understanding Total Compensation
A savvy professional knows that base salary is just one piece of the compensation puzzle. The total compensation package for a Nurse Practitioner is often far more valuable than the base salary alone. When evaluating a job offer, it's critical to consider the full suite of benefits, which can add tens of thousands of dollars in value annually.
Common Components of an NP Total Compensation Package:
- Bonuses: Many NP roles, especially in outpatient and private practice settings, include performance-based bonuses. These can be tied to productivity (e.g., number of patients seen, measured in Relative Value Units or RVUs), quality metrics (e.g., patient outcomes, satisfaction scores), or practice profitability. These bonuses can range from a few thousand dollars to over $20,000 per year.
- Profit Sharing: Some private practices offer profit-sharing plans, where a portion of the clinic's annual profits is distributed among the providers and staff.
- Health Insurance: A comprehensive employer-sponsored health, dental, and vision insurance plan is a standard and highly valuable benefit. Look for low premiums, deductibles, and out-of-pocket maximums.
- Retirement Plans: Most employers offer a retirement savings plan, typically a 401(k) for private companies or a 403(b) for non-profits (like hospitals and universities). The key factor here is the employer match. A common match is 50% of your contribution up to 6% of your salary, which is essentially free money for your retirement.
- Paid Time Off (PTO): This includes vacation days, sick leave, and holidays. A competitive PTO package is typically 3-5 weeks per year to start, increasing with seniority.
- Continuing Medical Education (CME): Because NPs must stay current with medical advancements, employers almost always provide a CME allowance. This typically includes 3-5 paid days off for conferences or training and a financial stipend of $1,500 to $3,000 per year to cover costs for registration, travel, and materials.
- Malpractice Insurance: Professional liability insurance is a necessity. Employers should provide and pay for a comprehensive "occurrence-based" or "claims-made with tail coverage" policy. This is a non-negotiable benefit that protects you from lawsuits.
- Licensing and Certification Fees: Many employers will reimburse the cost of state licensure renewal, DEA license fees, and board certification renewal fees, which can save you hundreds of dollars annually.
- Student Loan Repayment: In some high-need areas or government positions (like the National Health Service Corps), you may be eligible for significant student loan repayment programs, which can be worth tens or even hundreds of thousands of dollars.
When comparing job offers, it's essential to calculate the total value of each package, not just the number on the paycheck.
Key Factors That Influence Salary

While the national average salary provides a useful benchmark, your actual earnings as an NP will be determined by a complex interplay of several key variables. Understanding these factors is the most critical step in maximizing your income potential throughout your career. This section provides an in-depth analysis of the six primary drivers of a nurse practitioner salary.
### 1. Level of Education and Certification
Your educational foundation and the specific credentials you hold have a direct impact on your role, responsibilities, and pay.
- MSN vs. DNP: The two primary educational pathways to becoming an NP are the Master of Science in Nursing (MSN) and the Doctor of Nursing Practice (DNP). The MSN is the traditional degree, while the DNP is a terminal practice doctorate focused on clinical leadership, evidence-based practice, and systems improvement. Currently, while the DNP is promoted as the future standard for entry-to-practice, the salary difference for frontline clinical roles is often minimal to non-existent. The AANP reports that DNP-prepared NPs earn a median salary that is only slightly higher (around $5,000 more annually) than their MSN-prepared colleagues. However, the DNP becomes a significant salary driver for those seeking leadership, administrative, or academic positions. Roles like Director of Advanced Practice, Chief Nursing Officer, or university faculty often require or strongly prefer a DNP, and these positions come with substantially higher salaries.
- National Board Certification: After graduation, you must pass a national board certification exam specific to your patient population focus. The certification credential you hold (e.g., FNP-C, PMHNP-BC, AGACNP-BC) is a primary determinant of your job opportunities and, therefore, your salary. Holding multiple certifications can sometimes increase marketability and pay, especially if an employer needs a provider who can work across different departments (e.g., an NP certified in both family practice and emergency medicine).
### 2. Years of Experience
As detailed in the previous section, experience is a powerful and reliable factor in salary growth. This progression isn't just about longevity; it's about the tangible value that an experienced NP brings to a practice.
- Early Career (0-2 years): In the initial years, NPs are building speed, confidence, and procedural skills. Their patient volume may be lower as they take more time with each case and may require more frequent consultation with senior colleagues. Their salary reflects this learning phase.
- Mid-Career (3-9 years): By this stage, an NP is typically a highly efficient and autonomous provider. They can handle a full patient load, manage complex cases with minimal supervision, and have likely developed a reputation for quality care. They are a practice's workhorse, and their compensation rises to reflect this productivity. They may also begin generating additional value by precepting new NP students or mentoring new hires.
- Senior Career (10+ years): Seasoned NPs are clinical experts. Their value extends beyond direct patient care. They are often leaders who contribute to practice-wide quality improvement initiatives, develop clinical protocols, and serve as a resource for the entire medical team. This leadership and expertise command top-tier salaries and often open doors to lucrative administrative or specialized roles. For example, a senior NP in a cardiology practice who can independently manage complex device patients (pacemakers, defibrillators) is far more valuable and will be compensated more highly than a junior provider.
### 3. Geographic Location
Where you choose to practice is arguably one of the most significant factors influencing your salary. Compensation varies dramatically by state, city, and even between urban and rural settings.
Top-Paying States for Nurse Practitioners: According to the May 2023 BLS data, the states with the highest annual mean wages for NPs are:
1. California: $161,540
2. New Jersey: $147,150
3. Washington: $145,710
4. Oregon: $143,180
5. Nevada: $141,360
Top-Paying Metropolitan Areas: Salaries can be even higher in specific cities. The BLS highlights these metro areas as top-paying:
1. San Jose-Sunnyvale-Santa Clara, CA: $209,740
2. San Francisco-Oakland-Hayward, CA: $193,810
3. Napa, CA: $184,830
4. Vallejo-Fairfield, CA: $178,510
5. New York-Newark-Jersey City, NY-NJ-PA: $170,320
It's crucial to balance these high salaries against the cost of living. A $160,000 salary in San Francisco may not provide the same quality of life as a $135,000 salary in Houston, Texas, where housing and taxes are significantly lower.
Another key geographical factor is the state's practice authority. States with Full Practice Authority (FPA), where NPs can practice independently, often have more competitive job markets and robust salaries. This autonomy allows NPs to open their own practices, increasing their earning potential exponentially. It also makes them more attractive to employers, as they don't require costly physician collaboration or supervision agreements.
### 4. Work Setting (Practice Type & Size)
The type of facility where you work is a major determinant of your daily responsibilities, patient population, and compensation structure.
- Outpatient Care Centers / Private Practice: These settings are often among the highest paying. According to the BLS, NPs working in outpatient care centers earn an average of $139,180. These roles are often heavily based on productivity (RVUs), meaning high-performers can earn significant bonuses.
- Hospitals (State, Local, and Private): Hospitals are the largest employers of NPs and offer competitive salaries, with a BLS-reported mean wage of $135,190. Hospital-based roles, especially in specialty or acute care units (like the ICU or surgery), often come with shift differentials for nights, weekends, and holidays, which can substantially boost income. Benefits packages at large hospital systems are also typically excellent.
- Physician Offices: These settings are very common and offer a median salary close to the national average, at $125,050 according to the BLS. Compensation may be a mix of salary and productivity bonuses.
- Academic Institutions / Educational Services: NPs who work for universities, either in student health clinics or as faculty, tend to earn less in base salary (BLS mean: $116,360). However, these positions often come with unparalleled benefits, including excellent retirement plans, generous paid time off, and tuition benefits for themselves and their families. The work-life balance can also be more favorable than in high-volume clinical settings.
- Government / VA Facilities: Working for the federal government, such as in the Veterans Health Administration (VA), provides unique benefits. While the base salary might be on par with or slightly below the private sector, the benefits are exceptional. This includes a federal pension plan (FERS), a 401(k)-style plan (TSP) with a generous match, ample leave, and job security.
- Telehealth: This rapidly growing sector offers a wide range of salaries. Some telehealth platforms pay per consult, while others offer a salaried position. The flexibility and ability to work from home are major draws, and experienced NPs can often command high hourly rates for their services.
### 5. Area of Specialization
Your chosen clinical specialty is one of the most powerful levers you can pull to increase your salary. Demand and compensation vary significantly across different patient populations.
- Psychiatric-Mental Health Nurse Practitioner (PMHNP): This is consistently one of the highest-paying and most in-demand NP specialties. Due to a nationwide shortage of mental health providers, PMHNPs can command premium salaries, often starting in the **$130,000s and easily exceeding $150
