Are you drawn to a medical career that goes beyond diagnosis and delves into the art of restoration? A field where you help patients reclaim their lives, rebuild their strength, and rediscover their independence after a life-altering injury or illness? If you’re passionate about function, quality of life, and holistic patient care, a career in Physical Medicine and Rehabilitation (PM&R), also known as physiatry, might be your calling. But passion must be paired with practicality. You're likely wondering: what is the real earning potential? A PM&R salary is not just competitive; it's one of the most robust in the medical field, reflecting the profound value these specialists bring to the healthcare system.
This guide is designed to be your definitive resource on physiatrist compensation. We will move beyond simple averages to dissect the intricate factors that determine your income, from subspecialty choices to practice settings and geographic location. We will explore not just the "what" but the "why" behind the numbers, empowering you with the knowledge to navigate your career path and maximize your financial success. I once had a conversation with a senior physiatrist who had helped a young car accident victim learn to walk again using a custom-designed orthosis. He told me, "We don't just add years to life; we add life back to years. The compensation is a byproduct of restoring a person's entire world." That powerful sentiment captures the essence of this specialty—a unique fusion of high-impact work and substantial financial reward.
This article will provide an exhaustive analysis of a PM&R salary, supported by the latest data from authoritative sources, so you can make informed decisions about your future.
### Table of Contents
- [What Does a PM&R Physician (Physiatrist) Do?](#what-does-a-pmr-physician-physiatrist-do)
- [Average PM&R Salary: A Deep Dive](#average-pmr-salary-a-deep-dive)
- [Key Factors That Influence a PM&R Salary](#key-factors-that-influence-a-pmr-salary)
- [Job Outlook and Career Growth in PM&R](#job-outlook-and-career-growth-in-pmr)
- [How to Become a PM&R Physician: Your Step-by-Step Guide](#how-to-become-a-pmr-physician-your-step-by-step-guide)
- [Conclusion: Is a Career in PM&R Right for You?](#conclusion-is-a-career-in-pmr-right-for-you)
What Does a PM&R Physician (Physiatrist) Do?

Before we delve into the numbers, it's essential to understand the unique and vital role of a PM&R physician, or physiatrist. Unlike surgeons who fix problems with a scalpel, physiatrists are experts in non-operative, patient-centered care. They are the medical doctors who lead a collaborative team—often including physical therapists, occupational therapists, and speech-language pathologists—to improve a patient's function, reduce pain, and enhance their overall quality of life.
The scope of PM&R is incredibly broad. Physiatrists treat a vast array of conditions affecting the brain, spinal cord, nerves, bones, joints, ligaments, muscles, and tendons. Their patient base is diverse, ranging from a professional athlete recovering from a concussion to an elderly person learning to navigate life after a stroke, or a worker managing chronic back pain.
Core Responsibilities and Daily Tasks:
A physiatrist's work is dynamic and multifaceted. Their responsibilities typically include:
- Diagnosing Conditions: Performing comprehensive physical examinations, ordering and interpreting imaging (X-rays, MRIs), and conducting specialized diagnostic tests like electromyography (EMG) and nerve conduction studies (NCS) to pinpoint the source of pain or functional impairment.
- Developing Treatment Plans: Creating individualized, holistic treatment plans that may include prescription medications (for pain, spasticity, etc.), therapeutic exercise regimens, and referrals to physical, occupational, or speech therapy.
- Performing Procedures: Many physiatrists perform minimally invasive procedures to manage pain and improve function. These can include ultrasound-guided injections into joints and soft tissues, nerve blocks, trigger point injections, and Botox injections for muscle spasticity. Subspecialists may perform more advanced procedures like spinal cord stimulator trials.
- Leading a Rehabilitation Team: Acting as the "quarterback" of the rehabilitation team, coordinating care among therapists, social workers, psychologists, and other medical professionals to ensure a unified and effective approach.
- Patient and Family Education: Educating patients and their families about their condition, setting realistic recovery goals, and providing strategies for long-term management and prevention.
### A Day in the Life of a Physiatrist
To make this more concrete, let's imagine a day for a physiatrist working in a mixed inpatient and outpatient setting:
- 7:30 AM - 9:00 AM: Arrives at the inpatient rehabilitation facility (IRF). Conducts morning rounds, visiting 8-10 patients who are recovering from major events like spinal cord injuries, traumatic brain injuries (TBIs), or strokes. Reviews their progress, adjusts medication, and addresses any new medical issues.
- 9:00 AM - 10:00 AM: Leads the weekly interdisciplinary team conference. Discusses each inpatient's progress with the physical therapist, occupational therapist, speech therapist, case manager, and social worker. Together, they refine the treatment plan and set goals for the coming week, including discharge planning.
- 10:00 AM - 12:00 PM: Performs procedures. This could involve an EMG/NCS study to diagnose carpal tunnel syndrome in one patient, followed by an ultrasound-guided corticosteroid injection for another patient with shoulder bursitis.
- 12:00 PM - 1:00 PM: Lunch, often accompanied by reviewing patient charts, returning calls, and preparing for the afternoon clinic.
- 1:00 PM - 5:00 PM: Sees patients in the outpatient clinic. The schedule is varied: a follow-up for a patient with chronic low back pain, a new consultation for a runner with a sports injury, a patient requiring Botox injections for post-stroke spasticity, and a long-term follow-up for a previous inpatient with a TBI.
- 5:00 PM - 6:00 PM: Completes charting, signs off on orders, and handles administrative tasks before heading home.
This "typical day" highlights the dynamic nature of physiatry—blending diagnostic detective work, hands-on procedures, and compassionate team leadership to make a tangible difference in patients' lives.
Average PM&R Salary: A Deep Dive
Now, let's get to the core of your query: the financial compensation for this critical work. A PM&R salary is consistently ranked in the upper tier of physician salaries, reflecting the high level of training required and the significant demand for their services. It's important to look at data from multiple reputable sources to get a well-rounded picture.
The most authoritative reports, such as the Medscape Physician Compensation Report, provide an excellent benchmark. They survey thousands of physicians across the United States annually.
National Averages and Salary Ranges
According to the Medscape Physician Compensation Report 2023, the average annual salary for a PM&R physician is $322,000. This figure represents the average base salary plus any bonuses and profit-sharing contributions.
However, an average can be misleading. The actual salary range is vast, influenced by a multitude of factors we will explore in the next section. Data from various salary aggregators helps to illustrate this range:
- Salary.com (as of late 2023) reports the median physiatrist salary in the U.S. is $288,623, with a typical range falling between $261,643 and $318,482.
- Doximity's 2023 Physician Compensation Report places the average compensation for Physical Medicine & Rehabilitation even higher at $347,236.
- Payscale (as of early 2024) shows a range from approximately $158,000 (likely representing academic or entry-level positions) to over $360,000 for experienced, high-earning physiatrists.
The takeaway is clear: while a starting salary might be in the low-to-mid $200,000s, the potential to earn well over $350,000 or even $400,000+ with experience and subspecialization is very real.
### Salary by Experience Level
Like any profession, experience is a primary driver of income growth in PM&R. The journey from a resident's stipend to a senior partner's salary is significant.
| Career Stage | Typical Years of Experience | Estimated Annual Salary Range | Data Source & Notes |
| :--- | :--- | :--- | :--- |
| PM&R Resident | 0-4 (Post-Med School) | $60,000 - $80,000 | AAMC, ACGME data. This is a training stipend, not a full physician salary. Varies by location and year of residency (PGY-1 to PGY-4). |
| Entry-Level Physiatrist | 0-2 (Post-Residency) | $220,000 - $280,000 | Based on industry reports and job postings. Often includes a signing bonus. The lower end is typical for academic positions. |
| Mid-Career Physiatrist | 3-10 years | $280,000 - $350,000 | Medscape, Doximity. At this stage, physicians have established a patient base and may have partnership opportunities. |
| Senior/Experienced Physiatrist | 10+ years | $350,000 - $450,000+ | Medscape, Doximity. Top earners are often practice owners, highly productive physicians in private practice, or subspecialists in high-demand areas. |
### Beyond the Base Salary: Understanding Total Compensation
A physiatrist's W-2 is often much more than just their base salary. Total compensation is a package that can significantly increase overall earnings. When evaluating a job offer, it's crucial to look at the complete picture.
- Production Bonuses: This is one of the most significant components of a PM&R salary, particularly in private practice and hospital-employed settings. Physicians are often compensated based on their productivity, which is measured in Relative Value Units (RVUs). An RVU is a measure of value used by Medicare and other payers to determine reimbursement. Each patient encounter, procedure, and service has an assigned RVU value. The more patients you see and the more procedures you perform (like EMGs or injections), the more RVUs you generate, leading to a higher bonus. A common model is a base salary plus a bonus for RVUs generated above a certain threshold.
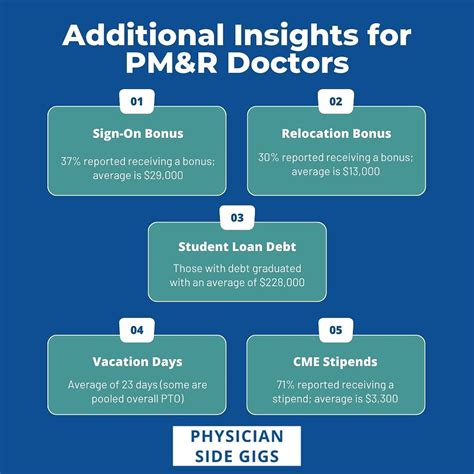
- Signing Bonuses: To attract top talent in a competitive market, many employers offer substantial signing bonuses. These can range from $15,000 to $50,000 or more, especially in underserved areas.
- Profit Sharing & Partnership Tracks: In private practice, physicians may be offered a partnership track after a few years. As a partner, you become a part-owner of the practice and share in its profits, which can dramatically increase your annual income beyond a salaried employee model.
- CME Allowance: Employers typically provide an annual allowance for Continuing Medical Education (CME), usually in the range of $3,000 - $5,000. This covers costs for conferences, workshops, and other educational activities required to maintain medical licensure.
- Retirement Benefits: Strong retirement plans, such as a 401(k) or 403(b) with a generous employer match, are standard. Some practices may offer more advanced options like cash balance plans for high-income earners.
- Relocation Assistance: For physicians moving to a new city for a job, relocation packages of $5,000 - $15,000 are common to cover moving expenses.
- Malpractice Insurance: The employer almost always covers the full cost of medical malpractice insurance, which is a significant expense.
Understanding these components is key. A job with a slightly lower base salary but a lucrative RVU bonus structure and a path to partnership could ultimately be far more financially rewarding than a flat-salaried position with no upside.
Key Factors That Influence a PM&R Salary
While we've established a strong baseline salary, the ~1500-word elephant in the room is the immense variability in compensation. Two physiatrists with the same years of experience can have a six-figure gap in their annual income. This difference is driven by a predictable set of factors. Mastering these variables is the key to strategically building a high-earning career.
###
Level of Education and Subspecialty Training
While all physiatrists must complete a four-year residency after medical school, the single most impactful educational choice for boosting salary is pursuing a fellowship. A one or two-year fellowship allows a physiatrist to become a board-certified subspecialist in a specific niche of PM&R. These subspecialties often involve more advanced, procedure-based skills, which directly translate to higher reimbursement and, therefore, higher earning potential.
Here's a breakdown of common PM&R fellowships and their general impact on salary:
- Interventional Pain Management: This is widely regarded as the most lucrative PM&R subspecialty. Pain management fellows receive advanced training in procedures like epidural steroid injections, facet joint injections, radiofrequency ablation, and spinal cord stimulator trials. Because these procedures are reimbursed at a high rate, physiatrists with a pain fellowship often earn significantly more than their generalist colleagues. It is not uncommon for interventional pain physiatrists in private practice to earn $500,000 to $700,000+ annually.
- Sports Medicine: A fellowship in sports medicine focuses on the non-operative treatment of athletic injuries. These physiatrists are experts in musculoskeletal ultrasound for both diagnosis and guiding injections (e.g., platelet-rich plasma - PRP). While not typically as high as interventional pain, sports medicine physiatrists still command a premium salary, often earning 10-20% more than a general physiatrist.
- Spinal Cord Injury (SCI) Medicine: This fellowship focuses on the complex, long-term care of patients with spinal cord injuries. While incredibly rewarding, it is generally less procedure-heavy than pain or sports medicine, so the salary bump is more modest. The value here is in specialized knowledge, leading to directorship roles in SCI units, which can come with administrative stipends.
- Traumatic Brain Injury (TBI) Medicine: Similar to SCI, this fellowship provides expertise in managing the cognitive, physical, and behavioral sequelae of brain injuries. Earning potential is comparable to general PM&R but opens doors to leadership positions in neuro-rehabilitation programs.
- Other Fellowships: Other subspecialties include Pediatric Rehabilitation, Neuromuscular Medicine, and Hospice/Palliative Care. These are driven more by passion for a specific patient population and, while respectable, do not typically lead to the top-tier salaries seen in interventional fields.
The Takeaway: Completing an ACGME-accredited fellowship, particularly in a procedure-heavy field like Interventional Pain, is the most direct educational path to a top-percentile PM&R salary.
###
Years of Experience and Career Trajectory
As illustrated in the table above, experience is a powerful salary driver. The income growth curve is steepest in the first decade of practice.
- Years 1-3 (Early Career): A physiatrist is fresh out of residency/fellowship. They are building their clinical speed, efficiency, and reputation. Salaries are often guaranteed for the first 1-2 years as they ramp up their practice. The focus is on learning the business of medicine and becoming proficient. Annual income is typically in the $220k - $280k range.
- Years 4-10 (Mid-Career): This is the prime growth phase. The physiatrist is now highly efficient, has a full patient panel, and may be generating significant RVUs. This is often when partnership offers are extended in private groups. Income climbs steadily into the $280k - $350k range for generalists, and higher for subspecialists.
- Years 11+ (Senior/Mature Practice): At this stage, income plateaus for many, but top earners continue to grow. These physiatrists may be practice owners, medical directors, or highly sought-after proceduralists. Their reputation drives referrals. For those in private practice or with a high-production model, salaries can comfortably exceed $400k or $500k. The Medscape report shows that physicians with 25+ years of experience often have the highest earnings.
###
Geographic Location
"Location, location, location" isn't just for real estate. In medicine, it's a huge determinant of salary. Compensation varies dramatically by state and even between urban and rural areas within the same state. This is often driven by supply and demand, cost of living, and local insurance reimbursement rates.
Interestingly, the highest-paying states are often *not* the ones with the highest cost of living, like New York or California. Instead, they are frequently in the Midwest and Southeast, where there is a greater need to offer competitive salaries to attract physicians.
Highest-Paying Regions/States (General Physician Trends that apply to PM&R):
According to various compensation reports (including Medscape and Doximity), states consistently ranking high for physician compensation include:
- Wisconsin
- Indiana
- Georgia
- Oklahoma
- Alabama
- Kentucky
Physiatrists in these states may earn 15-25% above the national average. A job in Indianapolis might pay significantly more than an equivalent one in Boston or Los Angeles.
Lower-Paying Regions/States:
Conversely, states in the Northeast and some on the West Coast tend to have more physicians per capita and lower reimbursement rates, leading to lower average salaries.
- Maryland
- Massachusetts
- Colorado
- District of Columbia
Urban vs. Rural: Rural and smaller metropolitan areas often have to offer higher salaries and better incentives (like student loan repayment) to recruit physiatrists compared to desirable, saturated major cities.
###
Company Type & Practice Setting
Where you choose to work has a colossal impact on your PM&R salary and overall work-life balance. Each setting has a different business model and compensation structure.
- Private Practice (Physician-Owned): This setting traditionally offers the highest income potential.
- Solo Practice: You are the boss and keep all the profits, but you also bear all the overhead, administrative burdens, and financial risk. Earning potential is theoretically unlimited but requires immense business acumen.
- Single-Specialty Group (SSG): A group of only physiatrists. This is a common and often lucrative model. You share overhead costs and call coverage. After a 2-3 year partnership track, you become a part-owner, sharing in the group's profits. This is a common path to earning $400k+.
- Multi-Specialty Group (MSG): A large group with physicians from many specialties (e.g., orthopedics, neurosurgery, primary care). This model provides a built-in referral base, which is a major advantage. Compensation is often very competitive and can rival SSGs.
- Hospital or Health System-Employed: This is an increasingly common model. The hospital employs you directly.
- Pros: Stable salary, predictable hours, no administrative hassle (billing, staffing, etc.), excellent benefits, and often no personal financial risk.
- Cons: Less autonomy and lower top-end earning potential compared to private practice ownership. Your salary is often a base plus a production bonus, but the "ceiling" is generally lower. This is a great option for those who prioritize stability and work-life balance. Average salaries are often right around the Medscape national average of $322,000.
- Academic Medicine: Working for a university medical center.
- Pros: Opportunities for teaching residents and medical students, conducting research, and treating complex cases.
- Cons: Significantly lower salaries compared to private practice. A physiatrist in academia might earn $200k - $250k. The compensation is traded for the prestige, intellectual stimulation, and other benefits of an academic career.
- Government/VA (Veterans Affairs): Working for the VA healthcare system or other government entities.
- Pros: Incredible job security, excellent federal benefits (including a pension), and a focus on patient care without the pressures of billing or RVUs.
- Cons: Salaries are generally lower than in the private sector and are often set by government pay scales. However, the work-life balance and benefits package can be very appealing.
###
In-Demand Skills and Procedural Competence
In the world of PM&R, "skills" directly translate to procedures you can perform and bill for. The more value you can provide through hands-on interventions, the higher your earning potential.
High-Value Procedural Skills:
- Electrodiagnostic Medicine (EMG/NCS): Proficiency in performing and interpreting these nerve and muscle studies is a core PM&R skill. It's a significant source of revenue for an outpatient practice.
- Musculoskeletal (MSK) Ultrasound: This has become the standard of care for diagnosing soft tissue injuries and for accurately guiding injections. Expertise in MSK ultrasound is highly sought after and increases your value.
- Fluoroscopy-Guided Spinal Injections: For pain specialists, being skilled in using X-ray guidance (fluoroscopy) to perform epidurals, facet blocks, and other spinal procedures is the cornerstone of a high-earning practice.
- Regenerative Medicine Procedures: Offering treatments like Platelet-Rich Plasma (PRP) and stem cell injections (where appropriate and regulated) can be a cash-based or high-reimbursement service that significantly boosts income.
- Spasticity Management: Advanced skills in using botulinum toxin (Botox) injections and managing intrathecal baclofen pumps for patients with stroke, MS, or cerebral palsy is a valuable niche.
A physiatrist who is a "generalist" and primarily manages patients through therapy referrals and oral medications will earn substantially less than a physiatrist who spends a significant portion of their time in a procedure suite.
Job Outlook and Career Growth in PM&R

A high salary today is wonderful, but career longevity and future demand are just as important. The great news for aspiring physiatrists is that the job outlook for this specialty is exceptionally bright.
BLS Projections and Market Demand
The U.S. Bureau of Labor Statistics (BLS) projects employment for all physicians and surgeons to grow by 3 percent from 2022 to 2032, which is about the average for all occupations. However, this general number doesn't tell the whole story for PM&R. The demand for physiatrists is expected to outpace many other specialties due to several powerful demographic and healthcare trends.
The Association of American Medical Colleges (AAMC) has consistently projected a significant physician shortage in the coming years, with specialty care being particularly affected. PM&R is right at the center of several major growth drivers:
1. The Aging Population: The baby boomer generation is entering its senior years, leading to a massive increase in age-related conditions that physiatrists specialize in treating. This includes strokes, arthritis, spinal stenosis, joint replacements, and general deconditioning. The focus on maintaining function and independence in this large population segment puts PM&R in a pivotal role.
2. Focus on Value-Based Care: The healthcare system is slowly shifting from a fee-for-service model to a value-based care model. This new model rewards providers for patient outcomes and cost-effective care. Physiatrists excel in this environment. By providing comprehensive, non-operative solutions, they can often help patients avoid costly surgeries and reduce hospital readmission rates, demonstrating immense value to health systems.
3. Advancements in Rehabilitation: New technologies, from advanced prosthetics and robotics to innovative regenerative medicine techniques, are expanding the scope of what is possible in rehabilitation. Physiatrists are at the forefront of implementing these technologies to improve patient outcomes.
4. Increased Survival from Trauma and Critical Illness: Modern medicine is better than ever at saving lives after catastrophic events like severe car accidents, battlefield injuries, and complex surgeries.