Table of Contents

- [Introduction](#introduction)
- [What Does a Psychiatric Nurse Practitioner Do?](#what-does-a-pmhnp-do)
- [Average Psychiatric Nurse Practitioner Salary: A Deep Dive](#average-salary)
- [Key Factors That Influence Salary](#key-factors)
- [Job Outlook and Career Growth](#job-outlook)
- [How to Get Started in This Career](#how-to-get-started)
- [Conclusion](#conclusion)
---
Introduction

Are you driven by a deep desire to heal minds, mend spirits, and make a tangible difference in the lives of those struggling with mental health challenges? Do you also seek a career that offers exceptional financial stability, professional autonomy, and a staggering demand for your skills? If so, you may be standing at the gateway to one of modern healthcare's most vital and rewarding professions: the Psychiatric-Mental Health Nurse Practitioner (PMHNP). This career isn't just a job; it's a calling that places you at the epicenter of the mental health crisis, armed with the clinical expertise to provide life-changing care.
The financial rewards for this demanding work are significant. While compensation varies, the national median salary for a Psychiatric Nurse Practitioner consistently lands in the $130,000 to $145,000 range, with seasoned professionals in high-demand areas earning well over $200,000 annually. This robust earning potential reflects the immense value society places on these highly specialized advanced practice nurses.
I once had the privilege of observing a PMHNP work with a young veteran battling severe post-traumatic stress disorder. Witnessing the practitioner's blend of compassionate therapy and precise medication management transform this individual from a state of withdrawn despair to one of hopeful engagement was a profound lesson in the power of this role. It is this unique fusion of the art of therapy and the science of pharmacology that makes the PMHNP a cornerstone of modern mental healthcare.
This guide is designed to be your definitive resource, whether you are a nursing student exploring specializations, an experienced RN contemplating a career change, or a current PMHNP seeking to maximize your career trajectory. We will dissect every facet of the PMHNP salary, explore the factors that can elevate your earnings, and provide a clear, actionable roadmap to entering and excelling in this extraordinary field.
What Does a Psychiatric Nurse Practitioner Do?

A Psychiatric-Mental Health Nurse Practitioner (PMHNP) is an Advanced Practice Registered Nurse (APRN) with specialized training and board certification in psychiatry. They are qualified to provide a wide spectrum of mental health services to individuals, families, groups, and communities. In many states, PMHNPs have "full practice authority," meaning they can operate their own independent practices without the supervision of a physician, much like a psychiatrist.
Their core mission is to assess, diagnose, and treat the mental health needs of their patients. This multifaceted role blends the diagnostic and prescriptive authority of a medical provider with the patient-centered, holistic approach of nursing. Unlike a therapist or counselor who cannot prescribe medication, and unlike a psychiatrist who may focus more heavily on medication management, the PMHNP is uniquely positioned to provide both medication management *and* psychotherapy, offering a truly integrated model of care.
Core Responsibilities and Daily Tasks:
- Comprehensive Psychiatric Evaluations: Conducting in-depth interviews with patients to gather a full medical, psychiatric, and social history to understand the root and scope of their issues.
- Diagnosing Conditions: Using the Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR) to accurately diagnose a wide range of conditions, such as depression, anxiety disorders, bipolar disorder, schizophrenia, PTSD, and substance use disorders.
- Developing Treatment Plans: Creating individualized, holistic treatment plans that may include psychotherapy, medication, lifestyle recommendations, and other therapeutic interventions.
- Prescribing Psychotropic Medications: Prescribing and managing medications like antidepressants, anxiolytics, mood stabilizers, and antipsychotics. This includes educating patients about side effects, monitoring for efficacy, and making adjustments as needed.
- Providing Psychotherapy: Offering various forms of talk therapy, such as Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), supportive therapy, and motivational interviewing.
- Patient and Family Education: Educating patients and their families about mental health conditions, treatment options, and coping strategies to empower them in their recovery journey.
- Collaboration: Working as part of an interdisciplinary team with physicians, psychologists, social workers, and other healthcare professionals to ensure coordinated patient care.
- Crisis Intervention: Providing immediate care and support for patients experiencing acute psychiatric emergencies, such as suicidal ideation or psychosis.
### A Day in the Life of a PMHNP
To make this tangible, let's imagine a day for "Dr. Carter," a PMHNP working in an outpatient community mental health clinic.
- 8:30 AM: Dr. Carter arrives, grabs a coffee, and reviews her schedule. She quickly checks patient charts, reviewing lab results for a patient on lithium and reading a consultation note from a primary care provider about a new referral.
- 9:00 AM: Her first patient is a 45-minute follow-up with a 28-year-old software developer being treated for Panic Disorder. They spend the first 20 minutes discussing his progress with CBT exercises to manage panic attacks and the last 25 minutes reviewing his SSRI medication, which they decide to continue at the current dose.
- 10:00 AM: The next appointment is a 60-minute new patient evaluation. Dr. Carter meets with a 65-year-old retired teacher experiencing symptoms of major depression following the death of her spouse. The session is a deep dive into her history, symptoms, and support system. By the end, Dr. Carter has made a provisional diagnosis and discussed the pros and cons of starting an antidepressant alongside weekly supportive therapy.
- 11:00 AM - 12:30 PM: Two more follow-up appointments, one for a teenager with ADHD and another for a patient with Bipolar II Disorder, focusing on medication adherence and mood stability.
- 12:30 PM - 1:30 PM: Lunch and charting. Dr. Carter diligently documents her morning sessions, sends prescription refills to pharmacies, and answers messages in the electronic health record (EHR) portal. She also has a quick "curbside consult" with a social worker at the clinic about housing resources for a patient.
- 1:30 PM: Dr. Carter leads a 90-minute group therapy session for adults with social anxiety, facilitating a discussion on exposure therapy techniques.
- 3:00 PM: She handles a crisis call from an established patient who is feeling overwhelmed and having passive suicidal thoughts. Dr. Carter spends 30 minutes on the phone, de-escalating the situation, reinforcing the patient's safety plan, and scheduling an urgent follow-up for the next day.
- 3:30 PM - 5:00 PM: Two final follow-up appointments.
- 5:00 PM - 5:30 PM: She finishes her final notes, signs off on charts, and responds to any remaining emails before heading home, having directly impacted the well-being of more than a dozen individuals.
This example illustrates the dynamic, challenging, and deeply impactful nature of the PMHNP role.
Average Psychiatric Nurse Practitioner Salary: A Deep Dive
The compensation for a Psychiatric Nurse Practitioner is one of the highest among all nurse practitioner specialties, a direct reflection of the high demand, advanced skill set, and significant responsibility the role entails. Salary data consistently shows a robust six-figure income, making it a financially lucrative career path within healthcare.
According to a 2023 report from the American Association of Nurse Practitioners (AANP), PMHNPs are the highest-paid of all NP specialties. The report states that full-time PMHNPs have a median total income of $145,000, which includes base salary, bonuses, and other incentives.
Let's break this down further using data from several authoritative sources, updated for 2024:
- Salary.com: Reports the median PMHNP salary in the United States as $132,610 as of early 2024. The typical salary range falls between $118,540 (25th percentile) and $145,468 (75th percentile), with the top 10% of earners exceeding $157,000.
- Payscale: Shows an average base salary of approximately $120,470 per year. However, when total compensation (including bonuses) is factored in, the range extends significantly, from $91,000 on the low end to $161,000 on the high end.
- Glassdoor: Cites an average total pay of $142,669 per year, with a likely range between $119,000 and $173,000. This figure incorporates base salary as well as additional compensation like bonuses and profit sharing.
- U.S. Bureau of Labor Statistics (BLS): The BLS provides data for all Nurse Practitioners under a single category. As of May 2023, the median annual wage for all Nurse Practitioners was $128,490. The top 10% of NPs earned more than $174,930. Given that PMHNPs are consistently reported as the highest-earning specialty, it's safe to assume their median is on the higher end of this spectrum.
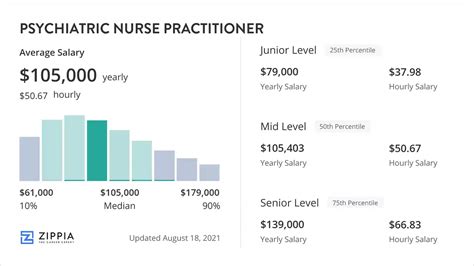
### Salary by Experience Level
Like any profession, experience is a primary driver of income growth. A newly certified PMHNP will earn less than a practitioner with a decade of experience who may also have administrative or leadership responsibilities.
Here is a typical salary progression, synthesized from data provided by Payscale and Salary.com:
| Experience Level | Typical Years of Experience | Average Annual Salary Range | Key Responsibilities & Skills |
| :--- | :--- | :--- | :--- |
| Entry-Level PMHNP | 0-2 years | $105,000 - $125,000 | Basic diagnostic assessments, medication management under some supervision (depending on state), developing foundational therapy skills. Focus is on building confidence and caseload. |
| Mid-Career PMHNP | 3-9 years | $125,000 - $145,000 | Full autonomy in patient care, managing more complex cases (e.g., treatment-resistant depression), mentoring new NPs, potential participation in clinical committees. |
| Senior/Experienced PMHNP | 10-19 years | $145,000 - $165,000+ | Expertise in a sub-specialty (e.g., addiction, forensics), leadership roles (e.g., Clinical Director), precepting students, potential for opening a private practice. |
| Late-Career/Expert PMHNP | 20+ years | $160,000 - $200,000+ | Often in high-level administrative, academic, or private practice owner roles. Seen as a thought leader, consultant, or policy advocate. Highest earning potential. |
### Understanding Your Total Compensation Package
It's crucial to look beyond the base salary. A comprehensive compensation package can add tens of thousands of dollars in value to your annual earnings. When evaluating a job offer, consider the following components:
- Base Salary: The fixed, predictable amount you earn. This forms the bulk of your compensation.
- Sign-On Bonus: Increasingly common, especially in high-need areas or for competitive positions. These can range from $5,000 to $25,000 or more, often tied to a commitment to stay for a certain period (e.g., two years).
- Performance Bonuses: Annual or quarterly bonuses tied to metrics like patient volume, quality of care outcomes, or clinic revenue.
- Profit Sharing: Common in private practice settings, where a portion of the practice's profits is distributed to employees.
- Health Insurance: A comprehensive health, dental, and vision insurance plan is a significant financial benefit. Look at the quality of the plan, deductibles, and the percentage of the premium covered by the employer.
- Retirement Savings Plan: Access to a 401(k) or 403(b) plan, especially one with a generous employer match, is critical for long-term financial health. An employer matching 4-6% of your salary is a substantial benefit.
- Paid Time Off (PTO): This includes vacation days, sick leave, and holidays. A generous PTO package (e.g., 4-6 weeks) improves work-life balance and is a valuable part of compensation.
- Continuing Medical Education (CME) Stipend: Most employers offer an annual allowance (e.g., $1,500 - $3,000) and paid time off to attend conferences, workshops, and courses required to maintain your license and certification.
- Malpractice Insurance: Employer-provided malpractice or liability insurance is standard and essential. Be sure to understand the type of coverage (occurrence vs. claims-made).
- Loan Repayment Programs: Some employers, particularly non-profits and government agencies (like the VA or HRSA-approved sites), offer loan repayment assistance, which can be worth tens of thousands of dollars.
When comparing offers, calculate the total value of each package, not just the base salary, to make a truly informed decision.
Key Factors That Influence a Psychiatric Nurse Practitioner's Salary
While the national averages provide a solid baseline, your individual earning potential as a PMHNP can vary dramatically based on a confluence of factors. Understanding these variables is the key to strategically navigating your career and maximizing your income. This is the most critical section for anyone looking to understand the nuances of PMHNP compensation.
### 1. Level of Education: MSN vs. DNP
The foundational requirement to become a PMHNP is a graduate degree. The two primary pathways are the Master of Science in Nursing (MSN) and the Doctor of Nursing Practice (DNP).
- Master of Science in Nursing (MSN): This has traditionally been the standard educational path for PMHNPs. It provides the core clinical knowledge and training required for assessment, diagnosis, and treatment in psychiatric care. An MSN-prepared PMHNP is fully qualified for certification and licensure.
- Doctor of Nursing Practice (DNP): The DNP is a terminal degree focused on clinical practice leadership. The curriculum builds upon the MSN foundation with additional coursework in evidence-based practice, quality improvement, systems leadership, health policy, and data analytics. It is designed to prepare nurses for the highest level of clinical practice.
Salary Impact: While an MSN is sufficient to earn a high salary, holding a DNP can provide a competitive edge and a moderate salary bump. Data suggests DNP-prepared PMHNPs earn, on average, $7,000 to $10,000 more per year than their MSN-prepared colleagues. This premium exists for several reasons:
- Advanced Expertise: The DNP signifies a higher level of education and expertise, which employers may reward.
- Access to Leadership Roles: DNP graduates are often prime candidates for leadership, administrative, and academic positions, which naturally come with higher salaries.
- Competitive Advantage: In a competitive job market, a DNP can be a deciding factor for hiring managers, particularly at prestigious academic medical centers.
### 2. Years of Experience and Career Trajectory
As detailed in the previous section, experience is arguably the single most significant determinant of salary after initial qualification. The salary growth trajectory for a PMHNP is steep in the first decade of practice.
- 0-2 Years (Entry-Level): The focus is on consolidating skills. Salaries are strong but reflect a learning curve. Employers invest in your development.
- 3-9 Years (Mid-Career): You have become a proficient, autonomous provider. Your efficiency, ability to handle complex comorbidity, and confidence command a higher salary. This is where many PMHNPs see the most significant percentage-based salary growth. You can confidently negotiate for higher pay based on a proven track record of positive patient outcomes.
- 10+ Years (Senior/Expert): At this stage, salary increases are driven less by clinical proficiency (which is assumed) and more by the additional value you bring. This can include:
- Opening a Private Practice: The single biggest leap in earning potential, with owners often earning $200,000 to $300,000+, though this comes with the risks and responsibilities of business ownership.
- Taking on Leadership Roles: Becoming a Director of Behavioral Health Services, a Chief Nursing Officer, or a lead PMHNP for a large clinic system carries significant salary premiums.
- Specializing: Developing a reputation as the go-to expert in a niche area like forensic psychiatry or perinatal mental health can allow you to command higher consultation fees or salaries.
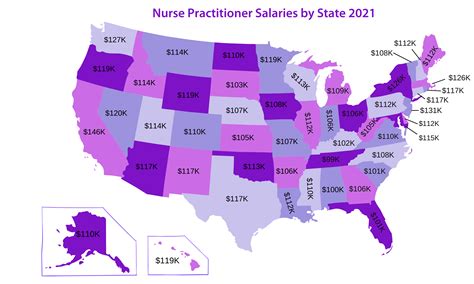
### 3. Geographic Location: Where You Practice Matters
Your physical location is a massive driver of salary, influenced by supply and demand, cost of living, and state-level scope of practice laws.
State-Level Variation: Salaries can vary by $30,000-$50,000 or more from the highest-paying states to the lowest-paying ones. According to the May 2023 BLS data for all Nurse Practitioners, the top-paying states are:
1. California: Annual Mean Wage: $161,540
2. New Jersey: Annual Mean Wage: $152,060
3. Massachusetts: Annual Mean Wage: $148,010
4. Oregon: Annual Mean Wage: $147,150
5. Nevada: Annual Mean Wage: $145,980
Conversely, states in the Southeast and parts of the Midwest tend to have lower average salaries, though the cost of living in these areas is also significantly lower. For example, states like Alabama, Tennessee, and Arkansas report median NP salaries closer to the $105,000 - $115,000 range. A $120,000 salary in Little Rock, Arkansas, may provide a higher quality of life than a $150,000 salary in San Jose, California.
Urban vs. Rural:
- Major Metropolitan Areas: Cities like San Francisco, New York, Los Angeles, and Boston offer the highest nominal salaries due to high demand and extremely high cost of living.
- Rural and Underserved Areas: These areas face critical shortages of mental health providers. To attract talent, they often offer very competitive salaries, excellent benefits, and access to significant loan repayment programs (like the National Health Service Corps Loan Repayment Program, which can provide up to $50,000 tax-free). A PMHNP position in rural Oregon might pay as much as one in Portland, but with a much lower cost of living and potentially a better work-life balance.
Scope of Practice Laws: There is a strong correlation between states with Full Practice Authority (FPA) and higher NP salaries. In FPA states, PMHNPs can practice independently, establish their own clinics, and bill directly for their services. This autonomy increases their market value. States like Arizona, Oregon, Washington, and Maryland are all FPA states with high NP salaries. In contrast, states with more restrictive practice laws (requiring physician supervision) can sometimes suppress wages.
### 4. Work Setting (Company Type & Size)
Where you choose to work has a profound impact on your daily life, patient population, and compensation structure.
- Private Psychiatric Practice: This setting offers the highest earning potential, particularly for practice owners. Salaried PMHNPs in established group practices can earn $140,000 - $180,000+. Owners who manage their billing, overhead, and patient load effectively can clear well over $250,000 annually.
- Hospitals (State, Local, and Private): Hospital systems are the largest employers of PMHNPs. They offer competitive salaries, typically in the $125,000 - $150,000 range, and excellent benefits packages (robust retirement plans, quality health insurance). Work may be in inpatient psychiatric units, consultation-liaison services (consulting on medical floors), or emergency departments.
- Outpatient Community Mental Health Centers (CMHCs): These clinics, often non-profits, serve a diverse and often underserved population. Salaries might be slightly lower than in the private sector, perhaps $115,000 - $135,000, but the non-salary benefits can be immense. Many CMHCs are qualifying sites for Public Service Loan Forgiveness (PSLF) and other federal loan repayment programs.
- Government (Federal): Working for the Department of Veterans Affairs (VA) or the military is a popular choice. The VA is the largest single employer of PMHNPs in the U.S. Federal salaries are transparent and based on a grade-and-step system. Pay is competitive, often $120,000 - $160,000+, and the benefits package is arguably the best available, with a generous pension plan (FERS), excellent health insurance, and ample time off.
- Telepsychiatry Platforms: The rise of telehealth has created a new employment model. PMHNPs can work from home, offering care to patients across the state (or in multiple states, if licensed). Compensation models vary. Some platforms offer a straight salary, while others pay per-consult or an hourly rate (typically $80 - $120 per hour). This offers unparalleled flexibility but may come with fewer traditional benefits.
- Academic Institutions: Working for a university involves a mix of clinical practice, teaching, and research. Salaries may be slightly lower than in a purely clinical role, but the position offers variety, prestige, and the reward of shaping the next generation of nurses.
### 5. Area of Sub-Specialization
While PMHNP is itself a specialization, developing expertise in a specific niche can increase your demand and salary.
- Child and Adolescent Psychiatry: There is a severe national shortage of providers who treat children and adolescents. PMHNPs with this sub-specialty are in extremely high demand and can command premium salaries.
- Addiction Medicine / Substance Use Disorders: With the ongoing opioid crisis, expertise in addiction is highly valued. PMHNPs with a DATA 2000 waiver (X-waiver, now updated) to prescribe buprenorphine and other medications for substance use disorders (SUDs) are critical assets.
- Geriatric Psychiatry: As the population ages, the need for mental health providers who understand the complexities of dementia, late-life depression, and the interaction of psychiatric and medical conditions in older adults is growing.
- Forensic Psychiatry: This niche involves working at the intersection of mental health and the legal system, conducting evaluations for court, working in correctional facilities, or consulting on legal cases. These roles are often high-stress but can be very high-paying.
- Perinatal Psychiatry: Focusing on the mental health of pregnant and postpartum individuals is a growing and vital field.
### 6. In-Demand Skills That Boost Your Value
Beyond your degree and certification, cultivating specific skills can directly translate to a higher paycheck.
- Psychotherapy Expertise: Being highly proficient in specific therapeutic modalities like DBT, EMDR (Eye Movement Desensitization and Reprocessing), or psychodynamic psychotherapy makes you more valuable than a practitioner who only manages medications.
- Telehealth Proficiency: Being comfortable and effective with virtual care platforms is no longer optional; it's a core competency that expands your employment options.
- Bilingualism: In a diverse country, being fluent in a second language, particularly Spanish, can significantly increase your salary (often a 5-10% premium) and make you a top candidate in many regions.
- Leadership and Management: Skills in budgeting, staff supervision, quality improvement, and program development can qualify you for higher-paying administrative roles.
- Complex Medication Management: Having expertise in managing complex regimens for conditions like treatment-resistant schizophrenia or bipolar disorder, including the use of long-acting injectables or Clozapine, sets you apart.
By strategically considering these six factors, you can move from being a passive job-taker to an active architect of your career and financial future.
Job Outlook and Career Growth

The career outlook for Psychiatric Nurse Practitioners is not just bright; it is explosive. The demand for qualified mental health professionals far outstrips the current supply, creating a job market that is exceptionally favorable for PMHNPs. This trend is projected to continue and even accelerate over the next decade.
The U.S. Bureau of Labor Statistics (BLS) projects that employment for all Nurse Practitioners will grow by 45% from 2022 to 2032. This is one of the fastest growth rates of any occupation in the entire U.S. economy, translating to about 118,600 openings for NPs each year, on average, over the decade. Within this group, the demand for PMHNPs is among the most acute.
Key Drivers of Unprecedented Demand:
1. The National Mental Health Crisis: Rates of depression, anxiety, trauma, and substance use have been climbing for years, a trend exacerbated by the COVID-19 pandemic. This has created an overwhelming need for accessible and effective mental