Have you ever watched a game-winning goal and marveled at the athlete's peak physical condition? Or perhaps you've seen a player go down with an injury and wondered about the team of experts dedicated to getting them back on the field? Behind every resilient athlete, every successful comeback, and every optimized performance is a highly skilled sports medicine doctor. This career is a unique and compelling fusion of medical science and the dynamic world of athletics, offering a path that is both intellectually challenging and deeply rewarding.
But beyond the passion for sports and medicine lies a practical question for anyone considering this demanding journey: what is the real earning potential? A sports medicine doctor's salary is a reflection of years of intense training, specialized knowledge, and the critical role they play in the health and well-being of active individuals. While national averages provide a starting point, often hovering in the impressive $250,000 to $350,000 range, the full story is far more nuanced. I remember shadowing a team physician during a high school football game; watching them calmly and expertly diagnose a potential concussion on the sideline in the midst of chaos was a powerful lesson. It showed me that this role isn't just a job; it's a calling that demands immense expertise and commands a commensurate level of compensation.
This comprehensive guide is designed to be your definitive resource on the sports medicine doctor salary. We will dissect every factor that influences your potential earnings, from the educational path you choose to the city you practice in. Whether you're a high school student dreaming of working with a pro team or a medical resident contemplating your fellowship, this article will provide the authoritative, data-driven insights you need to map out your future.
### Table of Contents
- [What Does a Sports Medicine Doctor Do?](#what-does-a-sports-medicine-doctor-do)
- [Average Sports Medicine Doctor Salary: A Deep Dive](#average-sports-medicine-doctor-salary-a-deep-dive)
- [Key Factors That Influence a Sports Medicine Doctor's Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth for Sports Medicine Doctors](#job-outlook-and-career-growth)
- [How to Become a Sports Medicine Doctor: Your Step-by-Step Guide](#how-to-get-started-in-this-career)
- [Is a Career in Sports Medicine Right for You?](#conclusion)
---
What Does a Sports Medicine Doctor Do?

A common misconception is that sports medicine doctors exclusively treat elite professional athletes. While some do achieve these high-profile roles, the vast majority of their patients are everyday people: high school athletes, "weekend warriors," industrial workers with overuse injuries, and older adults striving to stay active and mobile.
At its core, a sports medicine doctor is a physician who specializes in the prevention, diagnosis, and non-surgical treatment of injuries related to exercise and sports. They are experts in the musculoskeletal system—the intricate network of bones, joints, muscles, ligaments, and tendons that allows for human movement.
Their role is distinct from that of an orthopedic surgeon. While orthopedic surgeons also treat musculoskeletal injuries, their primary focus is on operative solutions. A primary care sports medicine physician, by contrast, is the master of non-operative care. They are the first line of defense, aiming to resolve 90% of sports-related injuries without the need for surgery. Their toolkit includes advanced diagnostics, targeted physical therapy prescriptions, medication management, and a range of in-office procedures.
Core Responsibilities and Daily Tasks:
- Diagnosis: Conducting comprehensive physical exams, interpreting medical histories, and ordering and analyzing diagnostic imaging like X-rays, MRIs, and musculoskeletal ultrasounds.
- Non-Surgical Treatment: Developing and managing treatment plans that may include physical therapy, medication, therapeutic injections (such as corticosteroids, hyaluronic acid, or Platelet-Rich Plasma - PRP), and activity modification recommendations.
- Injury Prevention: Educating patients, teams, and communities on proper conditioning, nutrition, and techniques to minimize the risk of injury.
- Concussion Management: Diagnosing and managing sports-related concussions, overseeing return-to-play and return-to-learn protocols, a critical and rapidly evolving area of the field.
- Medical Coverage: Providing on-site medical care at sporting events, from local high school football games to collegiate championships or professional leagues. This can involve immediate, high-pressure decision-making on the sideline.
- Collaboration: Working as part of a comprehensive care team alongside orthopedic surgeons, physical therapists, athletic trainers, nutritionists, and coaches to ensure a holistic approach to patient health and performance.
### A Day in the Life of a Sports Medicine Doctor
To make this tangible, let's follow Dr. Anya Sharma, a non-operative sports medicine physician working in a hospital-affiliated outpatient clinic.
- 7:30 AM - 8:30 AM: Dr. Sharma arrives at the clinic. She reviews her patient schedule for the day, checks imaging reports and lab results that came in overnight, and corresponds with physical therapists about their shared patients' progress. She has a quick huddle with her medical assistant and the clinic's athletic trainer to plan the day.
- 8:30 AM - 12:00 PM: Morning clinic begins. Her first patient is a 16-year-old soccer player with persistent knee pain. Dr. Sharma performs a detailed physical exam, using an in-office musculoskeletal ultrasound to get a real-time view of the patellar tendon, diagnosing tendonitis. She discusses a plan of activity modification and prescribes a specific physical therapy regimen. Her next few patients include a 45-year-old runner with shin splints, a 60-year-old golfer with elbow pain (epicondylitis), and a follow-up with a high school quarterback who is two weeks into the concussion protocol.
- 12:00 PM - 1:00 PM: Lunch is often a working one. Today, Dr. Sharma attends a virtual conference on new applications for biologic injections. This commitment to continuous medical education (CME) is essential.
- 1:00 PM - 4:30 PM: The afternoon clinic is dedicated to procedures. Dr. Sharma performs three ultrasound-guided corticosteroid injections for patients with shoulder bursitis and hip trochanteritis. She also sees a patient with osteoarthritis of the knee for a hyaluronic acid injection. These procedures require precision and skill, and the use of ultrasound dramatically improves accuracy and patient outcomes.
- 4:30 PM - 5:30 PM: Dr. Sharma finishes her patient charting for the day, returns calls, and signs off on prescription refills.
- 6:00 PM - 9:30 PM: It's a Friday night, so Dr. Sharma's day isn't over. As the team physician for a local university's football team, she heads to the stadium. She stands on the sideline, ready to evaluate and treat any injuries that occur during the game, working in tandem with the athletic trainers. It's a high-stakes environment, but seeing her patients compete safely is the ultimate reward.
This blend of clinical diagnosis, hands-on procedures, and high-energy event coverage makes a career in sports medicine uniquely dynamic and fulfilling.
---
Average Sports Medicine Doctor Salary: A Deep Dive
The financial compensation for a sports medicine doctor is substantial, reflecting the extensive education, specialized fellowship training, and high-stakes responsibility inherent in the role. While salaries can vary widely, we can establish a clear picture by analyzing data from reputable industry sources.
It's crucial to understand that most sports medicine doctors are first certified in a primary specialty like Family Medicine, Physical Medicine & Rehabilitation (PM&R), Pediatrics, or Emergency Medicine before completing a sports medicine fellowship. Therefore, their salaries are often benchmarked against these fields but with a premium for their additional qualification.
National Averages and Salary Ranges
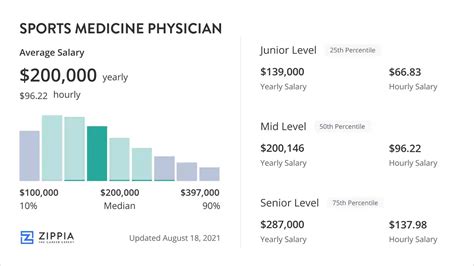
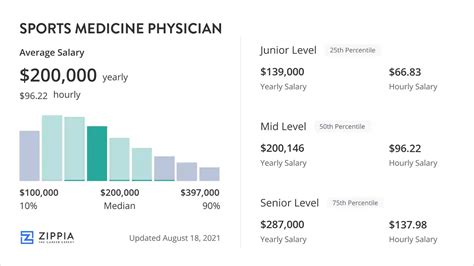
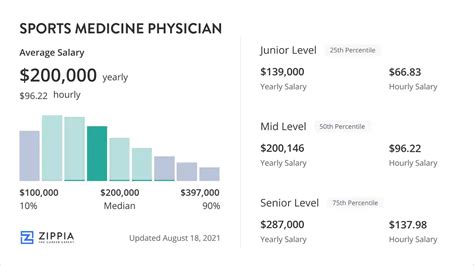
According to a composite of recent data from sources like Salary.com, Payscale, and Medscape's annual Physician Compensation Report, the national average base salary for a non-operative primary care sports medicine physician in the United States falls between $240,000 and $285,000 per year.
However, a national average only tells part of the story. The total compensation range is much broader:
- Entry-Level (10th Percentile): Physicians just completing their fellowship can expect to start in the $190,000 to $225,000 range.
- Median (50th Percentile): This represents the national average, typically around $265,000.
- Senior/Experienced (90th Percentile): Highly experienced physicians, especially those in private practice or high-demand locations, can earn $350,000 or more.
For instance, Salary.com's 2024 data reports the median salary for a Sports Medicine Physician at $261,399, with a typical range falling between $223,281 and $325,189. Similarly, Payscale lists a range of $154k - $298k for base salary, highlighting the variability in the field.
Salary Progression by Experience Level
A doctor's earning potential grows significantly with experience, reputation, and patient volume. Here is a typical trajectory:
| Experience Level | Years in Practice | Typical Annual Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level / Early Career | 0-4 Years | $190,000 - $240,000 | Fresh out of fellowship, focused on building a patient base, often in a hospital-employed or group practice setting. |
| Mid-Career | 5-15 Years | $240,000 - $300,000 | Established reputation, efficient patient workflow, may take on leadership roles or become a partner in a private practice. |
| Senior / Late Career | 15+ Years | $280,000 - $350,000+ | Peak earning years. May have multiple revenue streams (e.g., clinic, team coverage, medical directorships, teaching). |
*(Salary data is a synthesized estimate based on 2023-2024 reports from Salary.com, Medscape, and industry analysis.)*
Beyond the Base Salary: Understanding Total Compensation
A physician's W-2 is rarely just a base salary. Total compensation is a package that includes several other lucrative components.
- Productivity Bonuses: This is the most common form of additional income. Many employed physicians work under a model that includes a base salary plus a bonus based on productivity, often measured in Work Relative Value Units (wRVUs). The wRVU is a standardized measure of the value of a physician's service, factoring in the time, skill, and intensity required. A doctor who sees more patients or performs more procedures generates more wRVUs and thus earns a larger bonus. Medscape's 2023 report noted that the average incentive bonus for specialist physicians was around $85,000.
- Profit Sharing & Partnership: For doctors in private practice, this is a major pathway to higher earnings. After a few years as an employee, a physician may be offered a "partnership track." Once a partner, they share in the practice's profits, which can significantly exceed a salaried employee's income. This, however, also comes with the risks and responsibilities of business ownership.
- Ancillary Services Revenue: Private practices can generate additional revenue from in-house services like physical therapy, diagnostic imaging (MRI, X-ray), and durable medical equipment (braces, splints). Sports medicine physicians who own or are partners in such practices share in the profits from these valuable services.
- Stipends and Directorships: Many sports medicine physicians earn additional income through stipends for serving as a team physician for a university or high school district. Others may be paid a directorship fee for serving as the Medical Director of an athletic training program or a rehabilitation facility. These roles can add anywhere from $10,000 to $50,000+ annually.
- Standard Benefits Package: Like other high-level professionals, sports medicine doctors receive a robust benefits package, which is a significant part of their total compensation. This almost always includes:
- Health, dental, and vision insurance
- Generous retirement plans (e.g., 401(k) or 403(b) with employer match)
- Malpractice insurance coverage (a very expensive and critical benefit)
- Annual stipend for Continuing Medical Education (CME), typically $3,000 - $5,000
- Paid time off (vacation and sick leave)
- Disability and life insurance
When considering a job offer, it is imperative to look beyond the base salary and evaluate the entire compensation structure to understand the true long-term earning potential.
---
Key Factors That Influence a Sports Medicine Doctor's Salary
The difference between earning $220,000 and $380,000 is not random; it is driven by a predictable set of factors. Understanding these variables is the key to maximizing your earning potential throughout your career. This section provides a granular analysis of the elements that have the most significant impact on a sports medicine doctor's salary.
### ### Level of Education & Specialization Pathway
This is arguably the most significant differentiator in lifetime earnings. The path to becoming a "sports medicine doctor" can fork in two primary directions, with vastly different financial outcomes.
1. Primary Care Sports Medicine (Non-Operative)
This is the path we have focused on thus far. The journey involves:
- Medical School (MD or DO)
- Residency in a primary care field (e.g., Family Medicine, PM&R, Pediatrics).
- Sports Medicine Fellowship (1-2 years).
- Certificate of Added Qualifications (CAQ) in Sports Medicine.
Physicians on this track are the non-surgical experts. Their salaries, as detailed above, typically fall in the $240k - $350k range.
2. Orthopedic Surgery with Sports Medicine Fellowship (Operative)
This is a surgical pathway with a much longer and more competitive training process. The journey involves:
- Medical School (MD or DO)
- Orthopedic Surgery Residency (a highly competitive 5-year program).
- Sports Medicine Surgery Fellowship (1 year).
These doctors are orthopedic surgeons who specialize in surgically repairing sports injuries, such as ACL reconstructions, rotator cuff repairs, and labral repairs. Due to the high value and reimbursement rates for surgical procedures, their earning potential is substantially higher.
According to the Medscape Physician Compensation Report 2023, the average salary for an orthopedic surgeon is $573,000, making it one of the highest-paid medical specialties. Those with a sports medicine fellowship often find themselves on the higher end of this scale, particularly if they are the designated surgeons for professional or major collegiate teams.
The takeaway is clear: While both are "sports medicine doctors," the distinction between a non-operative primary care physician and an operative orthopedic surgeon is the single largest factor influencing salary, with surgeons earning, on average, nearly double their non-operative counterparts.
### ### Years of Experience and Reputation
As in any profession, experience pays. However, in medicine, "experience" is synonymous with reputation, efficiency, and trust.
- 0-4 Years (Building Phase): Early-career physicians focus on building a patient roster. Their schedules might not be completely full initially, and they are still honing their clinical efficiency. Salaries are often guaranteed for the first 1-2 years before transitioning to a productivity-based model.
- 5-15 Years (Peak Growth): A mid-career physician has a well-established referral network of primary care doctors, physical therapists, and coaches. Their clinical workflows are highly efficient, allowing them to see more patients and perform more procedures per day, directly boosting their wRVU generation and, consequently, their income. This is often the period where they are offered partnership in a private practice, leading to a significant jump in earnings.
- 15+ Years (Mature Practice): Senior physicians are at their peak earning potential. They are sought-after experts. Many diversify their careers at this stage, which can further increase income. They might take on lucrative administrative roles like a hospital department chair, a chief medical officer, or expand their team physician duties. They may also dedicate more time to teaching, research, or consulting, which provides both income and professional satisfaction.
### ### Geographic Location
Where you choose to practice has a profound impact on your salary, driven by local market demand, cost of living, and, most importantly, insurance reimbursement rates.
A 2023 physician salary report by Doximity noted that average physician pay could vary by over $100,000 between the highest and lowest-paying metro areas. While specific data for sports medicine is granular, we can extrapolate from data for primary care and orthopedic surgery.
Highest Paying States/Regions:
States in the Midwest and Southeast often offer higher compensation for physicians. This is driven by a combination of factors, including a greater need to attract talent away from major coastal cities and favorable reimbursement environments. States like Alabama, Kentucky, Oklahoma, Indiana, and Missouri consistently rank high for physician pay. For instance, a sports medicine practice in a mid-sized Midwestern city might offer a starting salary of $275,000 to attract a new fellow, compared to $230,000 in a more saturated coastal market.
Lower Paying States/Regions:
Conversely, states in the Northeast and some parts of the West Coast tend to have lower average physician salaries, despite a much higher cost of living. This is due to a high density of physicians, a greater number of academic institutions (which traditionally pay less than private practice), and often less favorable state-level insurance reimbursement policies. States like Maryland, Massachusetts, and Colorado often fall in this category.
Rural vs. Urban Divide:
There is a significant financial incentive to practice in rural or underserved areas. To combat physician shortages, rural hospitals and clinics often offer substantial compensation packages, including higher base salaries, significant sign-on bonuses (often $20,000-$50,000), and student loan repayment assistance programs (which can be worth tens or even hundreds of thousands of dollars). A physician might earn $300,000+ in a rural setting for a job that would pay $250,000 in a major metropolitan area.
### ### Practice Setting & Employment Model
The type of organization you work for is a critical determinant of your salary and work-life balance.
| Practice Setting | Typical Salary Range (Non-Operative) | Pros | Cons |
| :--- | :--- | :--- | :--- |
| Hospital / Health System Employed | $230,000 - $290,000 | Stable salary, strong benefits, less administrative burden, built-in referral base. | Less autonomy, potential for bureaucracy, salary ceiling may be lower than private practice. |
| Private Practice (Physician-Owned) | $250,000 - $400,000+ | High earning potential (especially as a partner), autonomy in clinical and business decisions. | Must manage business aspects (billing, HR, marketing), financial risk, requires buying into the practice. |
| Academic Medical Center | $210,000 - $260,000 | Opportunities for teaching and research, treating complex cases, prestige. | Generally lower salaries, pressure to publish research, clinical work may be secondary to academic duties. |
| Multi-Specialty Group | $240,000 - $310,000 | Combines stability of employment with the collaborative feel of a private group, strong internal referral network. | Can be large and bureaucratic, partnership tracks may be longer or more complex. |
| Direct Team Physician (Pro/D1) | Highly Variable | Working with elite athletes, high-profile role. | Very few full-time positions exist; often a supplemental role. Can be all-consuming with high travel demands. |
### ### In-Demand Skills and Procedural Competency
In an evolving medical landscape, certain skills can make you a more valuable asset and, therefore, a higher earner.
- Musculoskeletal (MSK) Ultrasound: This is arguably the most important procedural skill for a modern non-operative sports medicine doctor. Proficiency in using ultrasound for both diagnosis (e.g., identifying tendon tears) and for guiding injections (e.g., into a shoulder joint or nerve) is no longer a bonus; it is an expectation. Physicians who are highly skilled with ultrasound are more efficient, can offer more in-office procedures, and generate more revenue for their practice.
- Regenerative Medicine Expertise: A growing number of patients are seeking cutting-edge treatments like Platelet-Rich Plasma (PRP) and other orthobiologics. These are often cash-based procedures (not covered by insurance), providing a significant revenue stream for the practice and the physician. Doctors who build a reputation as experts in this niche can command higher service fees and attract a wider patient base.
- Concussion Management: With heightened awareness of the long-term effects of head injuries, clinics and teams are seeking true experts in concussion diagnosis and management. A physician known for their evidence-based, protocol-driven approach can become the go-to specialist in their region.
- Tenotomy Procedures: Advanced, minimally-invasive procedures like Tenex (percutaneous tenotomy) to treat chronic tendinopathy are another high-value skill. This allows a non-operative doctor to treat conditions that previously may have required open surgery, making them an invaluable part of a care team.
Mastering these skills not only improves patient care but also directly impacts the bottom line of a practice, making a physician with this toolkit a more attractive hire and a higher earner.
---
Job Outlook and Career Growth

For those willing to undertake the rigorous training, the future is exceptionally bright. The demand for sports medicine physicians is robust and projected to grow, driven by powerful demographic and societal trends.
Official Job Growth Projections
The U.S. Bureau of Labor Statistics (BLS) groups sports medicine physicians under the broader category of "Physicians and Surgeons." According to the BLS's 2022-2032 projections, employment in this category is expected to grow by 3%, which is about as fast as the average for all occupations. This will result in approximately 24,000 openings for physicians and surgeons each year, on average, over the decade.
While 3% might not seem explosive, it's important to contextualize this for a high-level profession. The demand is stable and consistent, driven by the need to replace retiring physicians and to meet the needs of a growing and aging population.
Key Trends Fueling Demand:
1. The "Active Aging" Population: Baby boomers and Generation X are remaining physically active later in life than any previous generation. This demographic is committed to activities like running, cycling, tennis, and golf, but is also more susceptible to overuse injuries, arthritis, and tendinopathies. They represent a large and growing patient base for sports medicine specialists who can help them stay in the game.
2. Increased Awareness of Sports Injuries: From youth leagues to professional sports, there is a greater understanding of the importance of proper injury management, especially concerning concussions. Schools, leagues, and parents are more likely than ever to seek out specialist care, moving away from the old "just walk it off" mentality. This cultural shift directly increases patient volume.
3. The Rise of the "Weekend Warrior": More sedentary professionals are engaging in high-intensity fitness activities. While beneficial for health, this often leads to injuries when individuals do "too much, too soon." This group frequently seeks sports medicine care to treat acute injuries and learn how to train more safely.
4. Emphasis on Non-Operative and Value-Based Care: The healthcare system is increasingly focused on finding effective, lower-cost alternatives to surgery. Sports medicine physicians are perfectly positioned to lead this charge. Their expertise in resolving injuries through physical therapy, injections, and rehabilitation aligns with the goals of value-based care, making them highly valuable to hospitals and insurance providers.
Future Challenges and Staying Relevant
Despite the positive outlook, the profession is not without its challenges.
- Insurance Reimbursement Battles: Physicians constantly face pressure from insurance companies to justify treatments and navigate complex pre-authorization processes. Reimbursement rates for some services may not always keep pace with inflation.
- Physician Burnout: The demands of clinical practice, administrative tasks (like electronic health records), and work-life balance can be significant. This is a challenge across all of medicine.
- Scope of Practice Creep: Other healthcare providers, such as physician assistants, nurse practitioners, and physical therapists, are expanding their scope of practice, creating more competition in the musculoskeletal care market.
How to Future-Proof Your Career and Advance:
- Embrace Lifelong Learning: Medicine is constantly changing. The physician who stays current on the latest research, diagnostic techniques (like advanced ultrasound applications), and treatment modalities (like orthobiologics) will always be in high demand.
- Develop a Niche: Instead of being a generalist, consider developing a deeper expertise in a specific area. This could be as a concussion specialist, a performing arts medicine expert, a specialist in female athlete health, or an expert in regenerative medicine. A niche makes you a referral magnet.
- Build Your Network: Cultivate strong relationships with primary care doctors, orthopedic surgeons, physical therapists, and athletic trainers in your community. A strong referral network is the lifeblood of a successful practice.
- Consider Leadership and Administrative Roles: As your career progresses, look for opportunities to take on leadership positions. This could involve becoming a medical director for a therapy clinic, a department head at a hospital, or serving on the board of a professional society like the American Medical Society for Sports Medicine (AMSSM). These roles not only increase your influence but also your income.
The path of a sports medicine doctor is not just a job, but a career with multiple avenues