Introduction

Imagine the deafening roar of a stadium, the focused intensity of an athlete pushing their limits, the quiet determination of a runner on a marathon course. Behind these moments of peak human performance is a network of support, and at its very core, you'll often find a sports medicine physician. This is a career that marries the intellectual rigor of medicine with the dynamic, high-stakes world of athletics. It’s a path for those who are not only fascinated by the intricate mechanics of the human body but are also deeply passionate about helping individuals—from professional athletes to "weekend warriors"—recover, excel, and stay in the game. If you're considering this demanding yet incredibly rewarding profession, one of your primary questions is likely about its financial viability. The good news is that the sports medicine physician salary reflects the extensive training, specialized expertise, and critical value these professionals bring to the healthcare landscape, with national averages often ranging from $250,000 to over $350,000 annually, and top earners exceeding $500,000.
As a career analyst, I've seen countless individuals seek professions that blend passion with practical, long-term stability. The field of sports medicine stands out as a prime example. I once had a conversation with a former collegiate soccer player whose career was threatened by a complex, recurring ankle injury. It wasn't a surgeon who solved her problem, but a non-operative sports medicine physician who, through meticulous diagnostic work and a novel rehabilitation plan, got her back on the field for her senior season. That story perfectly encapsulates the profound, life-changing impact these doctors have, an impact that is compensated accordingly.
This comprehensive guide is designed to be your definitive resource on the sports medicine physician salary. We will dissect every component of compensation, explore the factors that can significantly increase your earning potential, and provide a clear, actionable roadmap for embarking on this prestigious career path.
### Table of Contents
- [What Does a Sports Medicine Physician Do?](#what-does-a-sports-medicine-physician-do)
- [Average Sports Medicine Physician Salary: A Deep Dive](#average-sports-medicine-physician-salary-a-deep-dive)
- [Key Factors That Influence a Sports Medicine Physician's Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in a Sports Medicine Career](#how-to-get-started-in-this-career)
- [Conclusion: Is a Career in Sports Medicine Right for You?](#conclusion)
---
What Does a Sports Medicine Physician Do?

While the title may conjure images of a doctor rushing onto a football field, that sideline action is only a small, albeit visible, part of the job. A sports medicine physician is a medical doctor (MD or DO) who specializes in the prevention, diagnosis, and non-surgical treatment of injuries and illnesses related to physical activity and sports. They are the frontline experts for any musculoskeletal or medical issue that affects an active individual's ability to perform.
Their patient base is surprisingly diverse, extending far beyond elite athletes. They treat children with growth-plate injuries, high school athletes with concussions, middle-aged adults who injured themselves at the gym, and seniors hoping to maintain an active lifestyle. Their core philosophy is to restore function and minimize disability, using non-operative methods as the primary course of action.
Core Responsibilities and Daily Tasks:
A sports medicine physician's work is a blend of clinical practice, diagnostic investigation, and hands-on care. Here’s a breakdown of their typical duties:
- Patient Diagnosis and Consultation: Conducting thorough physical examinations, taking detailed patient histories, and diagnosing a wide array of musculoskeletal conditions, from acute sprains and fractures to chronic overuse injuries like tendonitis and stress fractures.
- Non-Surgical Treatment: This is their primary domain. They design and oversee comprehensive treatment plans that may include physical therapy, medication, therapeutic injections (such as corticosteroids, hyaluronic acid, or Platelet-Rich Plasma - PRP), bracing or casting, and lifestyle modifications.
- Medical Management of Athletes: They manage medical conditions that can affect performance, such as exercise-induced asthma, concussions, mononucleosis, and heat illness. They also provide guidance on nutrition and supplements.
- Diagnostic Imaging: Ordering and interpreting X-rays, MRIs, CT scans, and, increasingly, performing in-office musculoskeletal ultrasounds for real-time diagnosis and guided injections.
- Team and Event Coverage: Providing medical care "on the ground" for sports teams at the high school, collegiate, or professional level. This includes pre-participation physicals, sideline care during games, and managing injuries as they happen.
- Collaboration and Referral: Working closely with physical therapists, athletic trainers, and orthopedic surgeons. They are skilled at recognizing when a condition requires surgical intervention and will refer the patient to an orthopedic surgeon for further care.
### A Day in the Life: Dr. Anya Sharma, Primary Care Sports Medicine Physician
To make this tangible, let's follow a hypothetical day for a sports medicine physician working in a hospital-affiliated outpatient clinic.
- 8:00 AM - 9:00 AM: Dr. Sharma starts her day reviewing patient charts and imaging results from the previous day. She corresponds with a physical therapist via the electronic health record (EHR) system to adjust a rehabilitation protocol for a patient with patellofemoral pain syndrome.
- 9:00 AM - 12:30 PM: Morning clinic begins. Her patient list is varied: a 16-year-old basketball player for a follow-up on a concussion, a 45-year-old runner with Achilles tendonitis, a 65-year-old tennis player with shoulder pain, and a 22-year-old gymnast with a wrist sprain. For the tennis player, she uses an in-office ultrasound machine to visualize the rotator cuff tendons and performs an ultrasound-guided corticosteroid injection to reduce inflammation.
- 12:30 PM - 1:30 PM: Lunch, often combined with administrative tasks. She dictates her morning patient notes, returns calls to concerned parents, and has a quick call with the head athletic trainer at the local university she covers.
- 1:30 PM - 4:00 PM: Afternoon clinic. She sees more patients, including pre-participation physicals for the upcoming high school sports season. This involves screening for cardiac abnormalities and other conditions that could pose a risk during strenuous activity.
- 4:00 PM - 7:00 PM: Dr. Sharma drives to the local university to provide medical coverage for a collegiate soccer game. She assesses a player who twisted their knee on the field, performs sideline stability tests, and communicates her findings to the athletic training staff.
- 7:30 PM onwards: She returns home, where she might spend another 30-60 minutes finalizing charts and preparing for the next day.
This schedule highlights the dynamic nature of the role—blending the structured environment of a clinic with the unpredictable, fast-paced world of live sports.
---
Average Sports Medicine Physician Salary: A Deep Dive
The financial compensation for a sports medicine physician is substantial, reflecting the decade-plus of higher education and rigorous training required to earn the title. However, the salary is not a single, fixed number; it exists on a wide spectrum influenced by numerous factors we will explore in the next section.
It is crucial to distinguish between two main types of sports medicine physicians, as this is the single largest determinant of salary ranges:
1. Primary Care Sports Medicine Physicians: These doctors complete a residency in a primary care field (like Family Medicine, Pediatrics, or Internal Medicine) followed by a 1-2 year sports medicine fellowship. They are non-operative specialists.
2. Orthopedic Surgeon Sports Medicine Specialists: These are board-certified orthopedic surgeons who complete an additional fellowship in sports medicine. Because they perform surgery—often lucrative procedures like ACL reconstructions and rotator cuff repairs—their earning potential is significantly higher.
For the purpose of this guide, when we refer to a "sports medicine physician," we are primarily focusing on the non-operative, primary care-trained specialist, as this represents the most common pathway. We will, however, provide comparative data for their surgical counterparts.
### National Averages and Salary Ranges
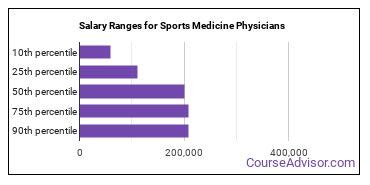
According to a variety of trusted sources, the national average salary for a non-operative sports medicine physician falls squarely in the six-figure range.
- Salary.com: Reports the median salary for a Sports Medicine Physician in the United States as $257,590 as of late 2023, with a typical range falling between $220,190 and $323,790.
- Payscale: Shows a slightly wider range, with an average base salary of approximately $225,000, but notes that total pay can reach up to $350,000+ when bonuses and profit-sharing are included.
- Medscape Physician Compensation Report: While not always having a separate category for non-operative sports medicine, it provides excellent proxy data. For example, the 2023 report lists Family Physicians (a common primary specialty) at an average of $255,000 and Pediatricians at $251,000. The additional fellowship and specialized procedures (like ultrasound-guided injections) in sports medicine typically add a significant premium to these base salaries. In contrast, the same report lists Orthopedic Surgeons at an average of $573,000, highlighting the surgical vs. non-surgical pay gap.
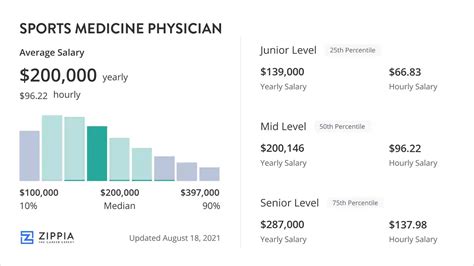
### Salary by Experience Level
Like any profession, experience is a powerful driver of salary growth. A physician's value increases as they build their reputation, hone their skills, and become more efficient.
Here is a typical salary progression for a non-operative sports medicine physician:
| Experience Level | Years in Practice | Typical Annual Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-3 Years | $190,000 - $240,000 | Just completed fellowship. Often in a hospital-employed or academic setting with a structured salary and productivity-based incentives. Focus is on building a patient panel. |
| Mid-Career | 4-10 Years | $240,000 - $320,000 | Established patient base and reputation. More efficient in the clinic. May take on leadership roles (e.g., team physician for a college) or become a partner in a private practice. |
| Senior/Experienced| 11-20+ Years | $300,000 - $450,000+ | At the peak of their earning potential. Often in private practice with ownership stakes, or hold prestigious roles like Medical Director for a health system's sports medicine division or a professional sports team. |
*(Salary ranges are estimates compiled from industry reports and salary aggregators like Salary.com and Doximity.)*
### Beyond the Base Salary: Understanding Total Compensation
A physician's base salary is only one piece of the puzzle. Total compensation is a far more accurate measure of their financial picture. Here are the other components that make up a sports medicine physician’s earnings:
- Production Bonuses: This is the most common form of additional income. Physicians are often compensated based on Relative Value Units (RVUs), a measure of the volume and complexity of the services they provide. The more patients they see and procedures they perform, the higher their bonus.
- Signing Bonus: To attract top talent, particularly in underserved areas, hospitals and large practices may offer a one-time signing bonus that can range from $10,000 to $50,000 or more.
- Profit Sharing/Partnership Track: In private practice, physicians may have the opportunity to become a partner after a few years. This means they share in the profits of the practice, which can significantly boost their annual income but also comes with the responsibilities of a business owner.
- Ancillary Services Revenue: A major income driver for private practices is offering in-house ancillary services like physical therapy, X-ray/MRI, and durable medical equipment (braces, crutches). Physicians often receive a share of the revenue generated from these services.
- Stipends and Directorships: Serving as the official team physician for a university or a Medical Director for a sports medicine program often comes with an annual stipend. This can range from a modest $10,000-$20,000 for a local high school to over $100,000 for a major NCAA Division I university or professional team.
- Benefits Package: While not direct cash, a strong benefits package has significant monetary value. This almost always includes comprehensive health, dental, and vision insurance; a generous retirement plan (e.g., 401(k) with employer match); and, critically, malpractice insurance coverage. Continuing Medical Education (CME) allowance (typically $3,000-$5,000 per year) is also standard.
When evaluating a job offer, it's essential to look at this complete picture. A lower base salary with a strong RVU bonus structure and a partnership track could be far more lucrative in the long run than a higher, flat salary at a different institution.
---
Key Factors That Influence a Sports Medicine Physician's Salary
The wide salary ranges discussed above are a direct result of several key variables. A prospective or practicing physician has significant control over many of these factors, allowing them to strategically shape their career path for maximum earning potential. This section provides an exhaustive breakdown of what moves the needle on a sports medicine physician salary.
###
Level of Education and Specialization Pathway
This is arguably the most fundamental factor. As mentioned previously, the path taken to become a sports medicine specialist creates a significant salary divergence.
- Primary Care Pathway (Non-Operative): This involves an undergraduate degree (4 years), medical school (4 years), a residency in a field like Family Medicine, PM&R, or Pediatrics (3-4 years), and finally, a Sports Medicine Fellowship (1-2 years). This 12-14 year journey leads to the salary ranges discussed primarily in this article ($220k - $350k+).
- Orthopedic Surgery Pathway (Operative): This involves the same undergrad and medical school path but is followed by a much longer and more competitive Orthopedic Surgery Residency (5 years) and a Sports Medicine Surgical Fellowship (1 year). This 14-year path leads to a significantly higher average salary, often in the $450,000 to $700,000+ range, because their practice is built around high-reimbursement surgical procedures.
Within the non-operative path, the choice of primary residency can have a minor impact. Physicians trained in Physical Medicine & Rehabilitation (PM&R), known as physiatrists, often have deep expertise in musculoskeletal and neurological rehab and may command slightly higher salaries due to their proficiency in advanced procedures like electromyography (EMG) and nerve conduction studies.
Key Takeaway: The decision to pursue a surgical vs. non-surgical career is the single biggest financial fork in the road.
###
Years of Experience and Reputation
As detailed in the salary progression table, experience is directly correlated with income. This isn't just about time served; it's about the value built over that time.
- Early Career (0-3 years): Physicians are focused on speed and efficiency. They are still building a referral network with primary care doctors, physical therapists, and local coaches. Their initial contract is often a guaranteed salary with productivity bonuses kicking in after a certain threshold.
- Mid-Career (4-10 years): By this point, the physician has an established reputation in the community. They receive direct referrals from former patients and have a streamlined clinical process. They are likely a partner in their practice or have renegotiated their hospital contract for a more favorable compensation model, often based entirely on productivity, which gives them higher earning potential. Salary growth is steepest during this phase.
- Late Career (11+ years): Senior physicians leverage their reputation to secure the most lucrative positions. They might be the go-to specialist for complex second opinions, serve as a medical director, or run a highly profitable private practice. Their income is a reflection of a career spent building clinical excellence and business acumen.
###
Geographic Location
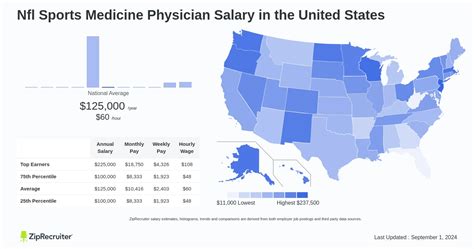
Where you practice medicine has a profound impact on your salary, driven by supply and demand, cost of living, and the local healthcare market.
- Highest Paying States/Regions: Physician salaries are often highest in regions that are less saturated with specialists and may be considered less traditionally "desirable" to live in, creating higher demand. According to Medscape and Doximity data, states in the Southeast (e.g., Alabama, Georgia, Florida) and the Midwest (e.g., Indiana, Wisconsin, Ohio) frequently offer higher compensation to attract physicians than an oversaturated coastal market. For instance, a sports medicine physician in Milwaukee might earn significantly more than one in Boston or Los Angeles, even after adjusting for cost of living.
- Lowest Paying States/Regions: Conversely, areas with a high density of academic medical centers and a perceived high quality of life, such as the Northeast (e.g., Massachusetts, Maryland) and parts of the West Coast (e.g., California), tend to have more competition and thus lower average salaries.
- Rural vs. Urban: Rural areas often pay a premium to attract physicians. A doctor in a rural hospital system could be the only sports medicine specialist for miles, giving them a captive patient population and a higher salary offer from the hospital trying to fill that need. However, urban centers offer more opportunities for high-volume private practice and lucrative cash-pay services.
Example Salary Variation by City (Illustrative):
- Charlotte, NC: ~$285,000
- Indianapolis, IN: ~$275,000
- Boston, MA: ~$240,000
- San Francisco, CA: ~$260,000 (Higher salary but dwarfed by extreme cost of living)
*(Data compiled and estimated based on Salary.com and Doximity regional reports.)*
###
Practice Setting (Company Type & Size)
The type of organization you work for is another massive determinant of your income structure and potential.
- Private Practice (Physician-Owned): This setting offers the highest income potential. This can be a solo practice or a multi-specialty group (e.g., a large orthopedic group that employs non-operative sports physicians). After an initial period on a guaranteed salary, physicians typically become partners. Their income is a direct reflection of the practice's profitability, including ancillary services. The trade-off is significant: partners are business owners, responsible for overhead, staffing, billing, and marketing. The risk is higher, but so is the reward. Typical Earning Potential: $300,000 - $500,000+.
- Hospital or Health System Employment: This is the most common model for early-career physicians. It offers stability and predictability. The hospital handles all administrative and business aspects. The physician receives a base salary plus production (RVU) bonuses. Benefits are usually excellent, and there's no business risk. However, the income ceiling is generally lower than in private practice. Typical Earning Potential: $220,000 - $350,000.
- Academic Medical Center: Working for a university hospital involves a "three-legged stool" of responsibilities: clinical work, teaching (medical students and residents), and research. The clinical load is often lighter, and the focus is on complex cases and advancing the field. As a result, direct compensation is typically lower than in private or hospital practice. The benefits come from intellectual stimulation, prestige, and strong institutional benefits. Typical Earning Potential: $190,000 - $280,000.
- Professional/Collegiate Team Employment: Being a full-time physician for a pro sports team or a major university is a niche and highly competitive role. The compensation structure can be complex, often a mix of a base salary from an affiliated hospital and a separate, substantial stipend from the team itself. While prestigious, these jobs are few and far between. Most team physicians maintain a primary clinical practice and cover the team as a portion of their job.
###
Niche Specializations and In-Demand Skills
Even within non-operative sports medicine, developing a niche can significantly boost your value and, therefore, your salary. Physicians who cultivate high-value, in-demand skills can command higher pay and open up new revenue streams.
- Musculoskeletal Ultrasound: Proficiency in using ultrasound for both diagnosis (visualizing tendons, ligaments, and muscles in real-time) and guiding procedures (injections) is arguably the most valuable clinical skill. It improves accuracy, patient outcomes, and is reimbursed by insurance. Physicians who are experts in this are highly sought after.
- Regenerative Medicine: This is a rapidly growing and often cash-pay field. Offering procedures like Platelet-Rich Plasma (PRP) therapy, prolotherapy, and stem cell injections for conditions like osteoarthritis and chronic tendon injuries can add a significant revenue stream to a practice. Since many of these are not covered by insurance, physicians can set their own prices.
- Concussion Management: With heightened awareness around sports-related concussions, having a dedicated concussion clinic and being recognized as a local expert can be a major practice builder and referral source.
- Female Athlete Triad/Relative Energy Deficiency in Sport (RED-S): Specializing in the complex interplay of nutrition, menstrual function, and bone health in female athletes is a growing niche that addresses a critical need.
- Business Acumen: For those in private practice, skills in management, marketing, and finance are just as important as clinical skills for maximizing income. Understanding how to run an efficient clinic and negotiate with insurance companies is paramount.
- Medical-Legal Consulting: Experienced physicians can serve as expert witnesses in legal cases involving sports-related injuries, which can be a lucrative side-income.
By strategically choosing a location, practice type, and developing in-demand skills, a sports medicine physician can navigate their career toward the highest echelons of the salary spectrum.
---
Job Outlook and Career Growth

For anyone investing over a decade in education, the long-term viability of their chosen profession is a critical concern. Fortunately, the job outlook for sports medicine physicians is exceptionally strong, driven by powerful demographic and societal trends.
### Job Growth Projections
The U.S. Bureau of Labor Statistics (BLS) projects the employment of physicians and surgeons, as a whole, to grow by 3 percent from 2022 to 2032. While this may seem modest, it translates to approximately 24,000 job openings each year, on average, over the decade, primarily due to the need to replace workers who retire or transfer to different occupations.
However, the outlook for sports medicine specifically is likely much stronger than this general figure suggests. Several factors contribute to a robust and growing demand:
1. An Aging but Active Population: The massive Baby Boomer generation is moving into its senior years but is more active than any preceding generation. They are participating in recreational sports, running, and fitness activities later in life, leading to a higher incidence of musculoskeletal injuries, osteoarthritis, and a desire for non-operative treatments to maintain their active lifestyles. These "weekend warriors" are a core patient base.
2. Increased Youth Sports Participation: Youth sports have become more intense and competitive at younger ages, unfortunately leading to a rise in overuse injuries, stress fractures, and other conditions that require specialized pediatric and adolescent sports medicine care.
3. Greater Awareness of Sports Injuries: High-profile media coverage of topics like concussions in the NFL and ACL tears in soccer has made athletes, parents, and coaches more proactive about seeking specialized medical care. The old "walk it off" mentality is fading, replaced by an understanding of the importance of proper diagnosis and treatment.
4. Emphasis on Value-Based Care and Prevention: Health systems are increasingly focused on preventing costly surgeries and hospitalizations. Non-operative sports medicine physicians are perfectly positioned in this model, as their primary goal is to resolve issues through more conservative and cost-effective means like physical therapy and rehabilitation.
### Emerging Trends and Future Challenges
The field is not static. Staying ahead of emerging trends is key to long-term success, while being aware of challenges is crucial for career longevity.
Key Trends:
*