For those with the ambition, intellect, and manual dexterity to master one of medicine's most intricate fields, a career as a vascular surgeon represents a pinnacle of professional achievement. It is a path defined by high-stakes procedures, life-altering patient outcomes, and, consequently, significant financial compensation. If you are exploring this demanding yet immensely rewarding specialty, you are likely asking a critical question: what does a vascular surgeon's salary truly look like? The answer is complex, with figures often reaching well into the high six figures, but influenced by a multitude of factors from geographic location to the specific nature of your practice.
I once had the privilege of interviewing a recently retired vascular surgeon for a feature on career longevity. He didn't dwell on the financial rewards, but on a single patient from early in his career—a young mother who nearly lost her leg after a car accident. He spoke of the painstaking, hours-long bypass surgery and the profound relief he felt weeks later when she walked into his clinic for a follow-up, her child holding her hand. That story crystallizes the essence of this profession: the salary is a reflection of the immense responsibility and the unique ability to restore life and function where it might otherwise be lost.
This comprehensive guide will dissect every component of a vascular surgeon's earnings, providing an authoritative look at not just the numbers, but the journey behind them. We will explore the national averages, the key drivers of salary, the future job outlook, and the rigorous steps required to enter this elite field.
### Table of Contents
- [What Does a Vascular Surgeon Do?](#what-is-a-vascular-surgeon)
- [Average Vascular Surgeon Salary: A Deep Dive](#deep-dive)
- [Key Factors That Influence a Vascular Surgeon's Salary](#key-factors)
- [Job Outlook and Career Growth for Vascular Surgeons](#job-outlook)
- [How to Become a Vascular Surgeon: A Step-by-Step Guide](#how-to-get-started)
- [Conclusion: Is a Career as a Vascular Surgeon Right for You?](#conclusion)
What Does a Vascular Surgeon Do?

A vascular surgeon is a highly specialized physician who diagnoses, treats, and manages conditions affecting the vascular system—the intricate network of arteries, veins, and lymphatic vessels that carry blood and fluid throughout the body. While the word "surgeon" implies a focus solely on the operating room, the reality of the role is far more multifaceted. They are the only specialists trained to treat vascular disease through every available modality: medical therapy, minimally invasive catheter-based procedures (endovascular surgery), and traditional open surgical reconstruction.
This comprehensive expertise is critical because vascular disease is often a chronic, systemic condition. A patient with peripheral artery disease (PAD), for example, may initially be managed with medication and lifestyle changes. As the disease progresses, the same vascular surgeon might perform an angioplasty or stenting procedure. If the condition becomes even more severe, that surgeon is also equipped to perform a complex surgical bypass. This continuity of care is a hallmark of the specialty.
Core Responsibilities and Conditions Treated:
- Diagnosis: Utilizing physical exams, patient history, and advanced imaging techniques like Doppler ultrasound, CT angiography (CTA), and MR angiography (MRA) to identify vascular problems.
- Medical Management: Prescribing medications such as blood thinners, cholesterol-lowering drugs, and blood pressure medications to manage disease and prevent progression.
- Endovascular Surgery: Performing minimally invasive procedures by navigating catheters and wires through blood vessels. Common procedures include angioplasty (inflating a balloon to open a vessel), stenting (placing a mesh tube to hold a vessel open), and endovascular aneurysm repair (EVAR).
- Open Surgery: Performing traditional surgical procedures that involve incisions to directly access and repair blood vessels. This includes carotid endarterectomy (removing plaque from the carotid artery), aortic aneurysm repair, and lower extremity bypass surgery for limb salvage.
- Patient Consultation: Educating patients and their families about their condition, treatment options, risks, and expected outcomes.
- Post-operative and Long-term Care: Managing patients after procedures and providing ongoing surveillance to monitor the vascular system for new or recurring issues.
### A Day in the Life of a Vascular Surgeon
To make this role more tangible, consider a typical (though often unpredictable) day for a hospital-employed vascular surgeon:
- 6:00 AM: Arrive at the hospital. Begin morning rounds on post-operative patients and new consults, checking on their recovery, reviewing vitals, and adjusting care plans.
- 7:30 AM: Morning conference with residents and fellows to discuss the day's surgical cases and review interesting consults from the previous night.
- 8:00 AM: First surgical case begins in the operating room. Today, it's a planned carotid endarterectomy to prevent a stroke in a 72-year-old patient. The procedure is intricate, requiring precise dissection around critical nerves.
- 11:00 AM: Head to the hybrid OR or catheterization lab for an endovascular case: an angioplasty and stenting of a blocked artery in the leg of a diabetic patient to treat pain and prevent amputation.
- 1:30 PM: A quick lunch while reviewing patient charts and responding to urgent pages.
- 2:00 PM: Afternoon clinic. See a mix of new patients referred for varicose veins, patients for pre-operative evaluation, and long-term follow-ups for aortic aneurysm surveillance.
- 5:00 PM: An emergency page arrives. A patient in the ER has a ruptured abdominal aortic aneurysm (AAA)—a life-threatening emergency. The surgeon immediately cancels remaining administrative tasks and heads to the OR for emergent surgery that will last several hours.
- 9:00 PM: The emergency surgery is successful. The surgeon speaks with the anxious family, dictates the operative note, and checks on their other patients before finally heading home, knowing they are still on call for any other emergencies that may arise overnight.
This example illustrates the intense blend of planned procedures, clinic management, and unpredictable emergencies that define the profession. It requires stamina, deep medical knowledge, and exceptional technical skill.
Average Vascular Surgeon Salary: A Deep Dive
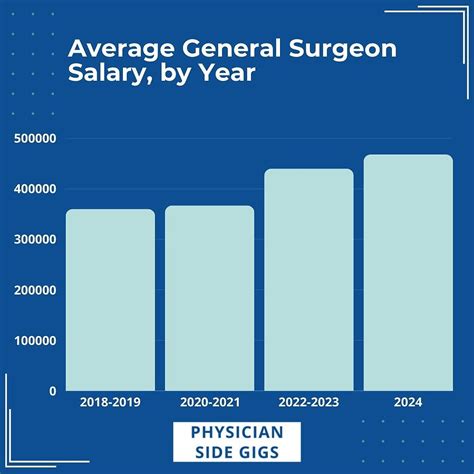
The significant demands, extensive training, and critical nature of vascular surgery place it among the highest-paid medical specialties. While exact figures fluctuate, the earning potential is substantial, consistently placing vascular surgeons in the top tier of physician earners.
It is crucial to understand that compensation is rarely just a flat salary. It is a package that often includes a base salary supplemented by productivity bonuses, benefits, and other incentives.
National Average Salary and Typical Range
According to several authoritative sources, the national median salary for a vascular surgeon in the United States falls in a robust range.
- Doximity's 2023 Physician Compensation Report, a comprehensive analysis based on data from over 190,000 U.S. physicians, lists the average compensation for Vascular Surgery at $557,632.
- Salary.com, which aggregates employer-reported data, states the median vascular surgeon salary in the U.S. is $488,724 as of late 2023, with a typical range falling between $415,808 and $571,118. The top 10% of earners can exceed $667,237.
- The 2023 Medscape Physician Compensation Report provides another valuable data point, showing an average salary for surgeons (a general category) at $412,000. While not specific to vascular, it's important to note that vascular surgery typically trends higher than the general surgery average due to its sub-specialization.
These figures highlight a consistent theme: an average salary hovering around $500,000, with a wide band that can stretch from roughly $400,000 for early-career surgeons to well over $700,000 for experienced, high-producing surgeons in private practice.
### Salary Brackets by Experience Level
Salary progression in surgery is steep and directly correlated with experience, reputation, and efficiency. As a surgeon becomes faster, takes on more complex cases, and builds a strong referral network, their productivity and, consequently, their income rises dramatically.
| Experience Level | Typical Annual Compensation Range | Key Characteristics |
| :--- | :--- | :--- |
| Entry-Level (0-3 Years Post-Fellowship) | $350,000 - $450,000 | Often starts with a guaranteed salary for the first 1-2 years. Focus is on building a practice, establishing referral patterns, and gaining efficiency in the OR. May receive a significant signing bonus. |
| Mid-Career (4-10 Years) | $450,000 - $650,000+ | Transitioned to a productivity-based model (e.g., wRVU). Has a mature practice, a strong reputation, and handles a high volume of complex cases. May be on a partnership track in a private group. |
| Senior / Late Career (11+ Years) | $550,000 - $800,000+ | Peak earning years. Highly efficient with a robust referral base. Often in a leadership position (e.g., Partner, Department Chair, Medical Director). May supplement income with consulting or medical device development. |
*Note: These ranges are illustrative and can be heavily influenced by the other factors discussed in the next section.*
### Deconstructing the Compensation Package
A vascular surgeon's total earnings are a composite of several components. Understanding these is key to evaluating any job offer.
1. Base Salary: This is the guaranteed portion of your pay. In hospital-employed models or academic medicine, this makes up a larger percentage of total compensation. In private practice, the "base" might be a smaller draw against future earnings.
2. Productivity Bonuses (wRVU Model): This is the most significant variable in modern physician compensation. The wRVU (work Relative Value Unit) is a measure assigned by Medicare to every medical service and procedure, reflecting its intensity, time, and required skill. Surgeons are often paid a certain dollar amount per wRVU they generate above a set threshold. A surgeon who performs many high-wRVU procedures (like complex aortic repairs) will have a much higher income than one who does not, even with the same base salary.
3. Signing Bonus: To attract top talent, especially in underserved areas, hospitals and groups offer substantial signing bonuses. These can range from $25,000 to $100,000 or more.
4. Call Pay: Surgeons are often paid a stipend for being on call for the hospital, which can be a daily rate (e.g., $1,000-$2,500 per day) or an hourly rate if they are called in for an emergency.
5. Performance & Quality Bonuses: Increasingly, a portion of compensation is tied to quality metrics, such as patient satisfaction scores, low complication rates, and adherence to best practices.
6. Benefits Package: This is a crucial, non-salary part of compensation. A strong package includes:
- Malpractice Insurance: Typically "occurrence-based" or "claims-made" with tail coverage, a value of tens of thousands of dollars per year.
- Health, Dental, and Vision Insurance.
- Retirement Plans: Such as a 401(k) or 403(b) with a generous employer match.
- Continuing Medical Education (CME) Allowance: An annual stipend ($5,000 - $15,000) for attending conferences and maintaining licensure.
- Relocation Allowance: Financial assistance for moving to a new city for a job.
7. Partnership/Equity (Private Practice): For those in private groups, the ultimate financial goal is partnership. This means buying into the practice and sharing in its profits, which can lead to the highest levels of income but also involves taking on business risk and administrative responsibilities.
Key Factors That Influence a Vascular Surgeon's Salary

While the national averages provide a useful benchmark, a vascular surgeon's actual salary is a dynamic figure shaped by a powerful interplay of professional choices and market forces. Two surgeons with identical skills can have vastly different incomes based on where and how they practice. This section provides an exhaustive breakdown of the most critical salary determinants.
###
1. Education and Advanced Training
The foundation of a surgeon's salary is their extensive and costly education. The journey is one of the longest in any profession, and the compensation reflects the delayed gratification and significant debt often incurred.
- The Foundational Path: The baseline for becoming a vascular surgeon is a Doctor of Medicine (M.D.) or Doctor of Osteopathic Medicine (D.O.) degree, followed by a demanding residency and fellowship. This entire post-college training process takes a minimum of seven years.
- The Two Training Paradigms:
- Independent "5+2" Fellowship: The traditional path involves completing a five-year General Surgery residency, followed by a highly competitive two-year Vascular Surgery fellowship.
- Integrated "0+5" Residency: A more modern, streamlined path where medical school graduates match directly into a five- or six-year residency dedicated solely to vascular surgery.
- Board Certification: Achieving board certification from the American Board of Surgery (ABS) in vascular surgery is the gold standard. It is a rigorous process that validates a surgeon's expertise and is a prerequisite for hospital credentialing and optimal compensation. Lack of board certification would be a significant barrier to high earnings.
- Advanced Fellowships: While not common, some vascular surgeons pursue an additional year of "super-fellowship" training in a niche area like complex aortic endovascular techniques or thoracic outlet syndrome. This specialized expertise can lead to a position as a regional expert, commanding a higher salary and attracting complex, high-reimbursement cases.
###
2. Years of Experience: The Path to Peak Earnings
As highlighted in the salary table, experience is arguably the most potent driver of salary growth for a surgeon. This isn't just about age; it's about the tangible development of skill, efficiency, and reputation.
- Early Career (Years 1-3): A new surgeon is often on a guaranteed salary as they build their practice. They are learning the hospital system, establishing relationships with referring physicians (primary care, cardiologists, nephrologists), and honing their operative speed. Their wRVU production is typically lower as they ramp up.
- Mid-Career (Years 4-10): This is where income often accelerates. The surgeon has transitioned to a productivity-based model. Their reputation is established, leading to a steady stream of referrals. They are highly efficient in the OR, able to perform more cases in the same amount of time. They are also comfortable with more complex, high-wRVU procedures. If in private practice, this is the typical window for becoming a partner.
- Peak Earning Years (Years 11-20): A senior surgeon is a master of their craft. They have a vast referral network and are often the "go-to" surgeon for the most challenging cases in the region. Their wRVU production is at its highest. They may hold leadership roles (Chief of Surgery, Medical Director) that come with additional stipends. Their value to a hospital or practice is immense, granting them significant leverage in contract negotiations.
###
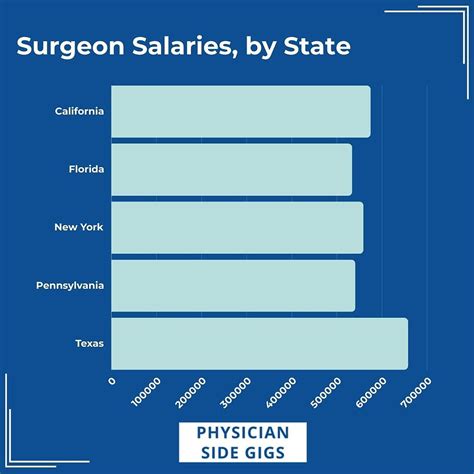
3. Geographic Location: The Stark Reality of Regional Markets
Where you choose to practice can impact your salary by hundreds of thousands of dollars. This variation is driven by supply and demand, cost of living, and the local insurance reimbursement landscape. Doximity's 2023 report provides clear evidence of this geographic disparity.
Highest-Paying States/Regions:
Often, less-populated states in the Midwest and Southeast offer higher salaries to attract scarce surgical talent. These areas may have fewer surgeons per capita, creating intense demand.
- Top-Paying States (Example Data from Physician Surveys):
1. Wisconsin
2. Indiana
3. Georgia
4. Connecticut
5. Texas
Lowest-Paying States/Regions:
Conversely, areas with a high density of physicians and academic medical centers, such as those on the East and West Coasts, tend to have more competition and thus lower average salaries, though the cost of living is often much higher.
- Lower-Paying States (Example Data from Physician Surveys):
1. Maryland
2. Massachusetts
3. Colorado
4. Virginia
5. Arizona
> Expert Insight: The "rural premium" is a significant factor. A surgeon willing to practice in a smaller, regional medical center that is the sole vascular provider for a large geographic area can often command a salary that surpasses those in major metropolitan hubs like New York or Los Angeles. They are more valuable to that specific hospital.
###
4. Practice Setting & Employment Model: The Autonomy vs. Security Trade-off
The type of organization you work for is a critical determinant of your compensation structure and overall earning potential.
- Private Practice (Physician-Owned Group):
- Salary Potential: Highest. After a 1-3 year partnership track, surgeons become owners and share in the group's profits. Top earners in this model can reach $800,000 to $1,000,000+.
- Structure: Income is directly tied to the productivity of the surgeon and the group, minus overhead costs (staff, rent, billing, malpractice).
- Pros: Maximum autonomy, direct financial reward for hard work.
- Cons: Involves running a business, managing staff, dealing with insurance companies, and personal financial risk.
- Hospital or Health System Employment:
- Salary Potential: Strong and stable, but generally capped lower than top-tier private practice. A typical range might be $450,000 to $650,000.
- Structure: Typically a base salary plus a wRVU-based production bonus. The hospital handles all administrative and business aspects.
- Pros: High degree of security, predictable income, excellent benefits, no business-related headaches.
- Cons: Less autonomy, may be subject to hospital-wide policies and bureaucracy, potential for less control over scheduling and case selection.
- Academic Medical Center:
- Salary Potential: Generally the lowest of the three models. A typical range might be $350,000 to $500,000.
- Structure: Salaried position with potential for modest bonuses.
- Pros: Prestige, opportunities for teaching residents and fellows, dedicated research time, access to cutting-edge technology.
- Cons: Lower direct cash compensation, pressure to publish research and secure grants ("publish or perish"), often more administrative duties. The "payment" is partially in the form of academic prestige and impact.
###
5. Procedural Focus and Sub-specialization
While "Vascular Surgery" is itself a specialization, a surgeon's income within the field can be influenced by the types of procedures they perform most frequently. Reimbursement rates, and thus wRVUs, vary significantly between different interventions.
- High-Reimbursement Procedures: Surgeons who build a practice focused on complex, high-acuity work tend to earn more. This includes:
- Complex Aortic Work: Open and endovascular repair of thoracic and abdominal aortic aneurysms (e.g., FEVAR - Fenestrated Endovascular Aortic Repair).
- Complex Limb Salvage: Multi-level bypasses and interventions for critical limb ischemia.
- Carotid Interventions: Carotid endarterectomy and TCAR (TransCarotid Artery Revascularization).
- Lower-Reimbursement Procedures: While still essential, some areas of vascular care have lower reimbursement rates. A practice that is heavily focused on venous disease (e.g., varicose vein ablations) or dialysis access may have a lower average revenue per case compared to an arterially-focused practice. The key to success in these areas is high volume and efficiency.
###
6. In-Demand Skills and Ancillary Services
Beyond the scalpel, certain skills and practice enhancements can significantly boost income.
- Advanced Endovascular Skills: Expertise in the latest minimally invasive technologies (e.g., new stent-grafts, atherectomy devices, advanced imaging) makes a surgeon highly valuable and able to perform procedures that were previously not possible.
- Office-Based Lab (OBL) Ownership: For private practice surgeons, establishing an accredited OBL to perform outpatient procedures (like angioplasties or varicose vein treatments) can be a major revenue generator. By owning the facility, the practice captures the "facility fee" in addition to the professional fee, substantially increasing the reimbursement for each case.
- Vascular Lab Interpretation: Surgeons who are credentialed as Registered Physicians in Vascular Interpretation (RPVI) can bill for the professional interpretation of the vascular ultrasounds performed in their practice's lab. This creates a consistent, non-operative revenue stream.
- Business Acumen: In private practice, understanding contract negotiation, billing and coding optimization, and efficient practice management are skills that directly translate to a higher take-home income.
Job Outlook and Career Growth for Vascular Surgeons
For those considering the long training path, the future stability and demand for the profession are paramount. The outlook for vascular surgeons is exceptionally strong, driven by powerful demographic and public health trends.
Job Growth Projections
The U.S. Bureau of Labor Statistics (BLS) projects that employment for all physicians and surgeons will grow by 3% from 2022 to 2032, which is about as fast as the average for all occupations. However, this general number masks the acute demand within specific specialties. For vascular surgery, the demand is expected to significantly outpace the overall average.
A 2020 study in the *Journal of Vascular Surgery* projected a substantial and growing workforce shortage. It estimated that by 2025, the demand for vascular surgeons would outstrip the supply by nearly 30%, a deficit of over 1,800 surgeons.
Key Drivers of Future Demand:
1. The Aging Population: The primary driver is the aging of the Baby Boomer generation. Vascular diseases, such as aortic aneurysms, peripheral artery disease, and carotid stenosis, are predominantly diseases of aging. As millions more Americans enter their 60s, 70s, and 80s, the incidence of these conditions will surge.
2. Rising Rates of Chronic Disease: The epidemics of obesity, diabetes, and hypertension are direct contributors to vascular pathology. A patient with poorly controlled diabetes is at extremely high risk for peripheral artery disease and subsequent limb loss, requiring the expertise of a vascular surgeon.
3. The Endovascular Revolution: The shift toward less invasive endovascular procedures has expanded the pool of patients who are eligible for treatment. Elderly or frail patients who were once considered too high-risk for major open surgery can now be treated safely with minimally invasive techniques, further increasing the volume of work for vascular surgeons.
4. Retiring Workforce: A significant portion of the current vascular surgeon workforce is approaching retirement age, which will create vacancies that need to be filled by new graduates.
Future Challenges and Staying Relevant
Despite the strong outlook, the profession faces challenges that aspiring surgeons must be prepared for:
- Physician Burnout: The long hours, high-stakes decisions, on-call burden, and administrative tasks can lead to significant stress and burnout. Maintaining a work-life balance is a critical, ongoing challenge.
- Reimbursement Pressures: Navigating the complexities of Medicare, Medicaid, and private insurance reimbursement is a constant battle. Downward pressure on reimbursement rates requires surgeons and practices to be more efficient and demonstrate value through quality outcomes.
- Turf Battles: Other specialties, such as interventional cardiology and interventional radiology, also perform peripheral vascular interventions. Vascular surgeons differentiate themselves through their comprehensive training in both open and endovascular techniques and their ability to manage the entire spectrum of a patient's vascular disease long-term.
Advancing in Your Career:
Career growth doesn't end after fellowship.