Introduction

Have you ever looked at a physician—whether a family doctor or a life-saving surgeon—and wondered about the journey they took to acquire such profound expertise? The path to becoming a doctor is one of society's most demanding and respected, requiring a decade or more of rigorous education, grueling training, and an unwavering commitment to patient care. This dedication, while driven by a passion for healing, is also rewarded with significant financial compensation, making medicine one of the highest-paying professions in the world. But the term "doctor's salary" is not a monolith; it's a complex landscape shaped by specialty, location, experience, and a dozen other factors.
The financial potential in medicine is vast, with average physician salaries in the United States often ranging from $250,000 for primary care physicians to well over $600,000 for top-tier surgical specialists. This article will dissect that range, providing a definitive guide to understanding what doctors truly earn and why. I once had a conversation with an orthopedic surgeon who had just completed a complex spinal fusion. He spoke not of the procedure's technical difficulty, but of the immense privilege of giving someone back their mobility and life—a perspective that perfectly frames the immense value and responsibility that underpins a physician's compensation. This guide is for the aspiring medical student, the curious pre-med, the resident weighing their options, and anyone seeking to understand the financial realities of a career in medicine.
### Table of Contents
- [What Does a Physician Do?](#what-does-a-physician-do)
- [Average Physician Salary: A Deep Dive](#average-physician-salary-a-deep-dive)
- [Key Factors That Influence a Doctor's Salary](#key-factors-that-influence-a-doctors-salary)
- [Job Outlook and Career Growth in Medicine](#job-outlook-and-career-growth-in-medicine)
- [How to Become a Physician: A Step-by-Step Guide](#how-to-become-a-physician-a-step-by-step-guide)
- [Conclusion: Is the Demanding Path Worth the Reward?](#conclusion-is-the-demanding-path-worth-the-reward)
---
What Does a Physician Do?

At its core, a physician's role is to diagnose and treat human disease, injuries, and other physical and mental impairments. They are the cornerstones of the healthcare system, applying scientific knowledge and clinical expertise to preserve and restore health. However, the modern physician's responsibilities extend far beyond a simple examination room consultation. Their work is a multifaceted blend of science, investigation, communication, and administration.
According to the U.S. Bureau of Labor Statistics (BLS), the primary duties of physicians and surgeons involve taking patient histories, performing physical exams, ordering and interpreting diagnostic tests, and prescribing treatments or medications. Yet, the execution of these duties varies dramatically by specialty. A pediatrician focuses on the developmental health of children, an anesthesiologist manages patient pain and vital signs during surgery, and a psychiatrist addresses the complexities of mental health.
The daily tasks of a physician are demanding and often unpredictable:
- Direct Patient Care: This is the most visible part of the job. It includes seeing patients in a clinical setting (outpatient) or conducting rounds on admitted patients in a hospital (inpatient). This involves active listening, empathetic communication, and critical thinking to form a diagnosis.
- Performing Procedures: Depending on the specialty, this can range from a dermatologist removing a mole to a cardiothoracic surgeon performing open-heart surgery. These tasks require immense technical skill, precision, and the ability to remain calm under extreme pressure.
- Documentation and Administration: A significant portion of a doctor's day is spent on administrative tasks. This includes meticulously updating electronic health records (EHRs), writing prescriptions, communicating with insurance companies for pre-authorizations, and corresponding with other healthcare providers about patient care. This "charting" is crucial for continuity of care and legal documentation but is often cited as a major contributor to physician burnout.
- Continuous Learning and Collaboration: Medicine is a constantly evolving field. Physicians must engage in Continuing Medical Education (CME) to stay abreast of the latest research, treatments, and technologies. They regularly collaborate with nurses, physician assistants, pharmacists, and other specialists in a team-based approach to patient care.
- On-Call Responsibilities: Many physicians, especially those in hospital-based or surgical specialties, are required to be "on-call," meaning they must be available to respond to emergencies outside of regular working hours, often overnight or on weekends.
### A "Day in the Life" of a Hospital-Based General Internist
To make this tangible, let's follow Dr. Anya Sharma, a fictional hospitalist (an internist who cares exclusively for hospitalized patients).
- 6:30 AM: Dr. Sharma arrives at the hospital. She gets a "sign-out" from the overnight physician, reviewing any critical events or new admissions for the patients on her service.
- 7:00 AM - 9:00 AM: She pre-rounds on her patients, quickly checking vital signs, talking to nurses, and reviewing new lab results and imaging studies that came in overnight. She formulates a plan for each patient for the day.
- 9:00 AM - 1:00 PM: This is the bulk of her rounding time. She goes room to room, accompanied by a resident and medical students. For each patient, she performs a focused exam, discusses the diagnosis and treatment plan in clear terms, answers questions from the patient and their family, and places new orders in the EHR. This could involve anything from adjusting IV fluids for a dehydrated patient to consulting a cardiologist for someone with chest pain.
- 1:00 PM - 2:00 PM: A quick lunch while catching up on non-urgent pages and reviewing notes from consultants.
- 2:00 PM - 5:00 PM: Dr. Sharma's afternoon is dedicated to "putting out fires" and documentation. She follows up on tests she ordered in the morning, admits new patients from the Emergency Department, and fields calls from specialists and family members. The bulk of this time is spent at a computer, meticulously documenting her findings and care plans for every patient she saw—a critical but time-consuming task.
- 5:00 PM - 6:30 PM: She prepares her "sign-out" list for the incoming evening physician, ensuring a safe handoff of care. She flags the sickest patients and any pending critical tasks.
- 6:30 PM: Dr. Sharma heads home, but her work isn't truly over. She might receive a non-urgent page about a patient later in the evening, and her mind is often still running through complex cases, a testament to the all-encompassing nature of the profession.
---
Average Physician Salary: A Deep Dive
The compensation for physicians is among the highest of any profession, a reflection of the extensive education, high-stakes responsibility, and specialized skills required. However, the salary figures can vary dramatically, creating a wide spectrum of earning potential.
According to the 2023 Medscape Physician Compensation Report, one of the most comprehensive annual surveys in the industry, the average overall physician salary in the United States is $352,000. This figure breaks down into an average of $265,000 for primary care physicians (PCPs) and a significantly higher $382,000 for specialists.
Similarly, the 2023 Doximity Physician Compensation Report, which analyzes data from over 190,000 U.S. doctors, reports an even higher average of $375,000 for PCPs and $475,000 for specialists. The discrepancy between sources often comes down to methodology and the specific demographics of the physicians surveyed, but both reports clearly illustrate a six-figure income as the standard.
It's crucial to understand that these are averages. The actual salary range is vast, stretching from just under $200,000 for some pediatricians in low-paying areas to over $1,000,000 for top-earning neurosurgeons in private practice.
### Physician Salary by Experience Level
A physician's salary follows a distinct upward trajectory throughout their career. The initial years of residency are marked by modest pay, which then skyrockets upon completion of training.
| Career Stage | Typical Years of Experience | Average Annual Salary Range | Notes |
| :--- | :--- | :--- | :--- |
| Medical Resident/Fellow| 0 (Post-Medical School) | $60,000 - $80,000 | This is a training salary, not a professional one. It is set by the institution and increases slightly each year of residency. |
| Early Career Physician| 1-7 Years (Post-Residency) | $220,000 - $350,000 | The largest salary jump occurs here. Initial salary is often guaranteed for 1-2 years before moving to a production-based model. |
| Mid-Career Physician| 8-20 Years | $300,000 - $550,000+ | Earnings increase as physicians become more efficient, build a patient base, and potentially become partners in a practice. |
| Senior/Late Career| 21+ Years | $320,000 - $600,000+ | Salary may plateau or even slightly decrease as some physicians choose to reduce hours or take on more administrative/teaching roles. |
*Source: Data compiled and synthesized from Medscape, Doximity, and MGMA (Medical Group Management Association) industry reports.*
### A Look at Total Compensation: Beyond the Base Salary
A physician's income is rarely just a flat salary. The total compensation package is a complex structure designed to incentivize productivity and attract top talent.
- Base Salary: This is the guaranteed portion of pay, common in hospital-employed models or for the first few years in a private practice.
- Production Bonuses (RVU-Based Compensation): This is the most common model after the initial guarantee period. Physicians earn bonuses based on their work output, measured in Relative Value Units (RVUs). Each patient encounter, procedure, and service is assigned an RVU value by Medicare. The more patients a doctor sees or the more complex procedures they perform, the more RVUs they generate, and the higher their bonus. This directly ties compensation to productivity.
- Signing Bonus: To attract physicians to a new role, especially in high-need areas or specialties, institutions often offer a one-time signing bonus, which can range from $10,000 to over $100,000.
- Performance & Quality Bonuses: With the shift towards value-based care, some compensation is tied to quality metrics, such as patient satisfaction scores, adherence to clinical guidelines, and positive patient outcomes.
- Partnership/Ownership Track: In private practice, physicians may be offered a path to partnership after a few years. As a partner, they buy into the practice and share in its profits, which can significantly increase their long-term earning potential beyond what a salaried employee could make.
- Ancillary Benefits: The benefits package is extremely valuable and a key part of total compensation. This almost always includes:
- Malpractice Insurance: Often a "claims-made" or "occurrence" policy fully paid for by the employer, which can be worth $10,000 to over $100,000 per year depending on the specialty.
- Continuing Medical Education (CME) Allowance: An annual stipend (e.g., $3,000 - $5,000) to cover costs for conferences and educational materials.
- Health, Dental, and Vision Insurance.
- Generous Retirement Plans: Such as 401(k) or 403(b) with significant employer matching contributions.
- Relocation Assistance: A stipend to cover the costs of moving for a new job.
- Licensing and Board Fee Reimbursement.
When considering a physician's salary, it's essential to look at this entire picture. A role with a slightly lower base salary but a lucrative production model and a path to partnership could be far more profitable in the long run than a high-salaried but stagnant hospital position.
---
Key Factors That Influence a Doctor's Salary

While the national averages provide a useful benchmark, a doctor's actual take-home pay is determined by a confluence of powerful factors. Understanding these variables is critical for any aspiring physician planning their career trajectory.
### ### 1. Area of Specialization (The Single Biggest Factor)
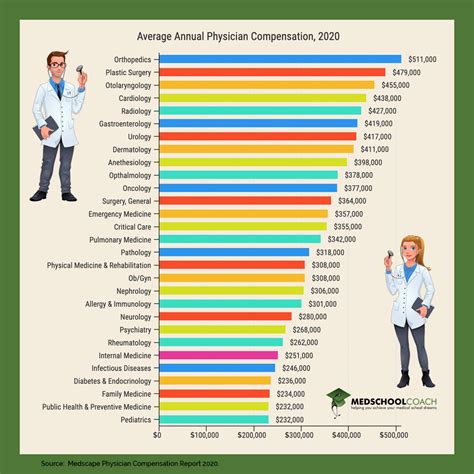
Without question, the choice of medical specialty is the most significant determinant of a physician's earning potential. The gap between the highest- and lowest-paying specialties can be more than $500,000 per year. This disparity is driven by several forces:
- Procedural vs. Cognitive Specialties: Specialists who perform procedures (surgeons, interventional cardiologists, gastroenterologists) are compensated at a much higher rate than those in primarily cognitive specialties (pediatricians, internists, endocrinologists). The healthcare reimbursement system, particularly Medicare, assigns higher values (RVUs) to procedures than to time spent on consultation and management.
- Length and Rigor of Training: Specialties requiring longer and more competitive residencies and fellowships (e.g., neurosurgery, plastic surgery) command higher salaries, partly as a return on that extended investment of time and lost earning years.
- Market Demand and Supply: Specialties facing a shortage of physicians relative to patient demand will see higher salaries.
- Call Schedules and Lifestyle: Specialties with more demanding on-call schedules and higher-risk procedures often have higher compensation to account for the lifestyle impact.
Here is a detailed breakdown of average annual salaries by specialty, illustrating the vast differences.
Top-Tier Earning Specialties (>$500,000)
| Specialty | Average Annual Salary | Brief Description |
| :--- | :--- | :--- |
| Neurosurgery | $788,313 | Surgeons who operate on the brain, spine, and nervous system. |
| Thoracic Surgery | $706,775 | Surgeons who operate on organs within the chest, primarily the heart and lungs. |
| Orthopedic Surgery | $624,043 | Surgeons who treat musculoskeletal trauma, spine diseases, and sports injuries. |
| Plastic Surgery | $571,373 | Surgeons who perform reconstructive and cosmetic procedures. |
| Vascular Surgery | $557,632 | Surgeons who treat diseases of the arteries and veins outside of the heart. |
| Cardiology (Invasive)| $544,293 | Physicians who perform procedures like stenting and angioplasty. |
| Radiation Oncology | $547,535 | Physicians who treat cancer using radiation therapy. |
| Gastroenterology | $512,583 | Specialists in the digestive system who perform procedures like colonoscopies. |
| Urology | $505,745 | Surgeons who treat conditions of the male and female urinary tract and male reproductive organs. |
High-Earning Specialties ($400,000 - $500,000)
| Specialty | Average Annual Salary | Brief Description |
| :--- | :--- | :--- |
| Radiology | $483,161 | Physicians who interpret medical images (X-rays, CTs, MRIs) to diagnose disease. |
| Dermatology | $471,000 | Specialists in skin, hair, and nail conditions. |
| Anesthesiology | $462,500 | Physicians who administer anesthesia and monitor patients during surgery. |
| Oncology | $447,214 | Physicians who diagnose and treat cancer, primarily with chemotherapy. |
| Ophthalmology | $417,000 | Physicians and surgeons who treat diseases of the eye. |
| General Surgery | $412,000 | Surgeons who perform a wide range of common surgeries, often related to the abdomen. |
| Pulmonology | $408,000 | Specialists in diseases of the lungs and respiratory system, often in critical care. |
Mid-Range and Primary Care Specialties (<$400,000)
| Specialty | Average Annual Salary | Brief Description |
| :--- | :--- | :--- |
| Emergency Medicine | $373,000 | Physicians who work in emergency departments, treating acute illnesses and injuries. |
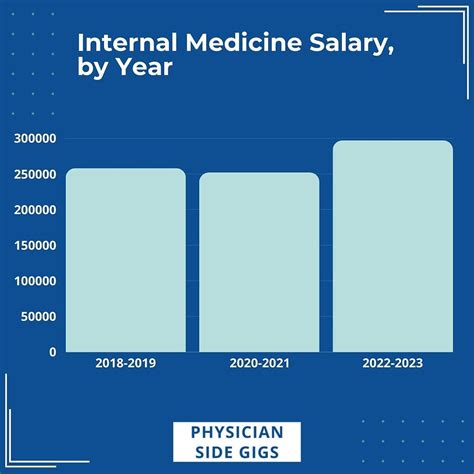
| Internal Medicine | $273,000 | Primary care physicians for adults, focused on disease prevention and management. |
| Family Medicine | $255,000 | Primary care physicians for the entire family, from infants to the elderly. |
| Psychiatry | $250,000 | Physicians specializing in the diagnosis and treatment of mental illness. |
| Neurology | $290,000 | Specialists in non-surgical treatment of the brain and nervous system (e.g., stroke, epilepsy). |
| Pediatrics | $244,000 | Primary care physicians for infants, children, and adolescents. |
| Public Health & Prev. Med. | $243,000 | Lowest-paying specialty, focused on population health rather than individual patient care. |
*Sources: Data compiled from 2023 reports by Doximity, Medscape, and Salary.com. Figures are averages and can vary significantly.*
### ### 2. Geographic Location
Where a physician chooses to practice has a profound impact on their salary, often in counter-intuitive ways. The highest salaries are not always found in major coastal cities with high costs of living. Instead, they are often in regions with a higher demand for physicians and a lower saturation of specialists.
According to the Doximity report, there's a principle of "geographic arbitrage" at play. States in the Southeast and Midwest often offer higher compensation to attract physicians away from the more traditionally desirable (and doctor-saturated) coastal markets.
Top 5 Highest-Paying States for Physicians (Average Annual Salary)
1. Oklahoma: $426,242
2. Alabama: $423,043
3. Missouri: $422,931
4. Indiana: $420,109
5. Kentucky: $416,519
Top 5 Lowest-Paying States for Physicians (Average Annual Salary)
1. District of Columbia: $342,139
2. Maryland: $350,904
3. Massachusetts: $358,639
4. Hawaii: $362,354
5. Delaware: $367,314
The difference between practicing in Oklahoma and Maryland could be over $80,000 per year, on average. Furthermore, the cost of living in Oklahoma is substantially lower, meaning the effective take-home pay and quality of life for the same salary are much higher.
Rural vs. Urban: Physicians in rural areas often earn more than their urban counterparts. Rural communities face chronic physician shortages and must offer higher salaries, loan forgiveness programs, and generous signing bonuses to recruit talent. A family physician might earn $240,000 in a major metropolitan area but be offered $300,000 plus student loan repayment to work in a rural clinic two hours away.
### ### 3. Practice Setting and Employment Model
The type of organization a physician works for is another critical salary driver. The traditional image of a doctor running their own small practice is becoming less common, with most physicians now being salaried employees.
- Private Practice (Physician-Owned): This model offers the highest earning potential. Physician-owners not only earn a clinical salary but also share in the profits of the practice, which can include revenue from ancillary services like in-house labs or imaging centers. However, this comes with the added responsibility and risk of running a business, including managing staff, billing, and overhead.
- Private Practice (Employee): A physician employed by a private group will earn a competitive salary and bonus but will not share in the practice's overall profits. They have less administrative burden but a lower long-term ceiling on income compared to partners.
- Hospital or Health System Employee: This is now the most common employment model. Hospitals offer a stable, predictable salary, excellent benefits, and handle all administrative and billing aspects. Compensation is often very competitive, especially for in-demand specialties, but may have less upside than a successful private practice. The average salary for hospital-employed physicians is often slightly lower than for those in private practice.
- Academic Medical Center: Physicians at universities and teaching hospitals typically earn less than their counterparts in private practice or community hospitals. A portion of their time is dedicated to research, teaching medical students and residents, and administrative duties, which are compensated at a lower rate than clinical work. The trade-off is the prestige, intellectual stimulation, and opportunities for groundbreaking research.
- Government (e.g., VA, Military, Public Health): Government-employed physicians (e.g., working for the Department of Veterans Affairs) generally have the lowest salaries. However, these roles offer unparalleled job security, excellent benefits, predictable hours, and often qualify for generous loan forgiveness programs.
### ### 4. Level of Education and Sub-specialization
While all physicians must complete medical school and residency, pursuing further training in a fellowship can significantly boost earning potential. A fellowship is 1-3+ years of additional training in a sub-specialty after residency is complete.
For example:
- An Internal Medicine resident (3 years of training) becomes a general internist earning an average of $273,000.
- If that internist completes a 3-year Cardiology fellowship, their average salary jumps to over $490,000.
- If they further sub-specialize with a 1-year Interventional Cardiology fellowship, their average salary can exceed $540,000.
This demonstrates that the investment in additional years of training directly translates into higher lifelong earning power.
### ### 5. In-Demand Skills and Procedural Competencies
Within any given specialty, physicians who have mastered specific, high-demand skills can command higher compensation.
- Advanced Procedural Skills: An orthopedic surgeon who is an expert in robotic-assisted knee replacement or complex spinal reconstruction will be more valuable and productive than one who only performs basic procedures.
- Leadership and Administrative Roles: Physicians who take on leadership roles, such as Chief of a department, Medical Director, or Chief Medical Officer (CMO), receive an administrative stipend on top of their clinical salary. These roles require management and business skills in addition to clinical expertise.
- Telehealth Proficiency: In the post-pandemic era, proficiency with telemedicine platforms and a willingness to conduct virtual visits can increase a physician's patient panel and efficiency, leading to higher productivity-based pay.
- Bilingualism: In diverse communities, the ability to speak a second language (such as Spanish) can be a significant asset, making a physician more attractive to employers and potentially leading to a larger patient base.
---
Job Outlook and Career Growth in Medicine
The long-term career outlook for physicians and surgeons in the United States is exceptionally strong. Despite the long training path and significant challenges, the demand for medical services continues to outpace the supply of doctors, ensuring robust job security and sustained salary growth for the foreseeable future.
According to the U.S. Bureau of Labor Statistics (BLS) Occupational Outlook Handbook, employment of physicians and surgeons is projected