Table of Contents

- [Introduction: Decoding the Value of a Urologist](#introduction)
- [What Does a Urologist Do? A Fusion of Medicine and Surgery](#what-does-a-urologist-do)
- [Average Urologist Salary: A Deep Dive into Compensation](#average-urologist-salary)
- [Key Factors That Influence Urologist Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth for Urologists](#job-outlook-and-career-growth)
- [How to Become a Urologist: Your Step-by-Step Roadmap](#how-to-become-a-urologist)
- [Conclusion: Is a Career in Urology the Right Fit for You?](#conclusion)
Introduction: Decoding the Value of a Urologist
For those drawn to the intricate and demanding world of medicine, the field of urology presents a unique and compelling path. It is a specialty that requires the diagnostic acumen of an internist, the steady hand of a surgeon, and a profound degree of empathy to navigate some of life's most sensitive health issues. If you are considering this challenging yet immensely rewarding career, one of the primary questions on your mind is likely: "What is the average urologist salary?" The answer is that urology is not only one of the most vital and innovative medical specialties but also one of the most financially rewarding. Urologists consistently rank among the highest-paid physicians, with an average annual salary often soaring well above $450,000, and top earners pushing into the high six or even seven figures.
This financial potential, however, is merely a reflection of the immense value urologists provide. I was reminded of this profoundly when a close family member faced a terrifying kidney cancer diagnosis. The urologic surgeon we met was a paragon of professionalism, blending technical brilliance with a calm, reassuring demeanor that turned our fear into a structured plan for hope. Watching them explain a complex robotic-assisted partial nephrectomy with such clarity and confidence was a masterclass in medical communication and expertise. It's this unique combination of high-stakes skill and deep human connection that defines the profession and justifies its significant compensation.
This guide is designed to be your definitive resource on the journey to and through a career in urology. We will move far beyond a simple salary number to provide a comprehensive analysis of the financial, professional, and personal landscape of this elite medical specialty. We will dissect compensation data from the most reliable sources, explore the crucial factors that dictate earning potential, and map out the rigorous path required to join its ranks. Whether you are a student contemplating medical school, a resident weighing specialties, or simply curious about this high-stakes profession, this article will provide the in-depth, authoritative answers you seek.
What Does a Urologist Do? A Fusion of Medicine and Surgery
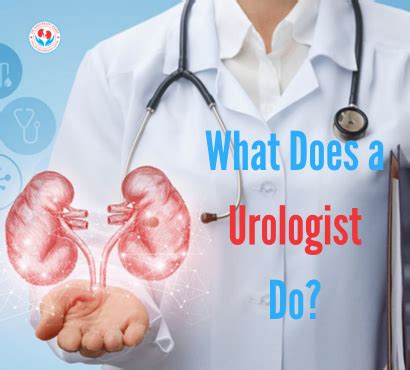
At its core, urology is the surgical specialty that focuses on the diseases of the male and female urinary tract systems and the male reproductive organs. Urologists are experts in the health of the kidneys, adrenal glands, ureters, urinary bladder, urethra, and the male reproductive organs (testes, epididymis, vas deferens, seminal vesicles, prostate, and penis). This broad scope makes the field incredibly diverse, offering a mix of clinical practice and complex surgical procedures that is rare among medical specialties.
Unlike a cardiologist who might primarily manage conditions with medication and refer to a cardiothoracic surgeon for operations, a urologist is often both the diagnostician *and* the surgeon. They manage chronic conditions like an overactive bladder with medication and behavioral therapy, while also being the one in the operating room performing a prostatectomy for cancer or removing a kidney stone with a laser.
Daily Tasks and Core Responsibilities:
A urologist's work can be broadly categorized into two main areas: office-based clinical practice and hospital-based surgical procedures.
- Clinical Diagnosis and Management:
- Conducting patient consultations to diagnose conditions like urinary tract infections (UTIs), benign prostatic hyperplasia (BPH), kidney stones, urinary incontinence, and erectile dysfunction.
- Performing in-office procedures such as cystoscopy (inserting a small camera into the bladder), vasectomies, prostate biopsies, and urodynamic studies (to assess bladder function).
- Prescribing medications and developing long-term treatment plans for chronic urologic conditions.
- Providing cancer screenings, particularly for prostate, bladder, and kidney cancer.
- Surgical Intervention:
- Performing a wide array of surgeries, ranging from minimally invasive to major open operations.
- Endourology: Using small scopes and instruments inserted through the urinary tract to treat conditions like kidney stones.
- Laparoscopy and Robotics: Utilizing minimally invasive techniques, most notably with the da Vinci® Surgical System, for procedures like prostatectomies, nephrectomies (kidney removal), and pyeloplasties (kidney reconstruction).
- Urologic Oncology: Surgically removing cancerous tumors from the prostate, bladder, kidneys, and testes.
- Reconstructive Urology: Repairing structures of the urinary tract following trauma, cancer surgery, or congenital defects.
### A Day in the Life of a Urologist
To make this tangible, consider a typical day for a urologist in a private practice group:
- 7:00 AM - 8:00 AM: Hospital Rounds. The day begins at the hospital, checking on post-operative patients. This involves reviewing their charts, assessing their recovery, managing any complications, and communicating with the nursing staff before discharging them.
- 8:30 AM - 12:00 PM: Morning Clinic. The urologist heads to their private office for a packed schedule of patient appointments. This might include a new patient with blood in their urine, a follow-up with a prostate cancer survivor, a consultation for a vasectomy, and an annual check-up for a patient with a history of kidney stones.
- 12:00 PM - 1:00 PM: Lunch & Administrative Tasks. A brief window to grab lunch, return urgent phone calls, review lab results and imaging reports (like CT scans and MRIs), and sign off on patient charts.
- 1:30 PM - 4:30 PM: Operating Room. The afternoon is dedicated to surgery at the hospital or an affiliated surgery center. Today's schedule might include a robotic-assisted prostatectomy for cancer and a ureteroscopy with laser lithotripsy to break up a large kidney stone.
- 5:00 PM - 6:30 PM: Evening Clinic & Final Admin. A few more patient appointments may be scheduled after surgery. The day concludes by finishing charting, dictating operation notes, and responding to non-urgent messages before heading home. This doesn't include the "on-call" responsibilities, where a urologist must be available overnight or on weekends for emergencies like a severe kidney stone attack or urinary retention.
This demanding schedule highlights the need for exceptional time management, intellectual stamina, and technical skill, all of which are factored into the specialty's high compensation.
Average Urologist Salary: A Deep Dive into Compensation
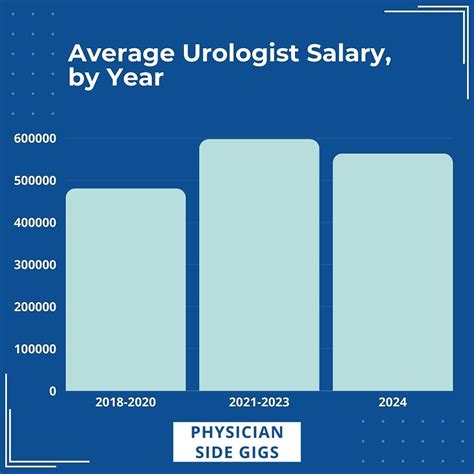
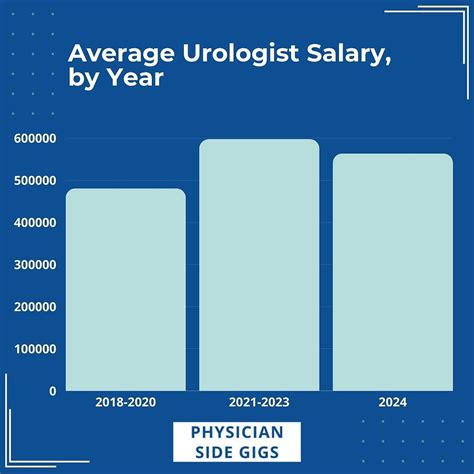
Urology is consistently positioned in the top tier of physician salaries, a direct reflection of the extensive training required, the procedural nature of the work, and the high demand for its services. While the exact "average urologist salary" can vary based on the data source, a clear picture of substantial earning potential emerges from all reputable reports.
According to the 2023 Medscape Physician Compensation Report, one of the most comprehensive surveys in the industry, the average annual salary for a urologist in the United States is $506,000. This places urology among the top 5 highest-paying specialties, alongside plastic surgery, orthopedics, cardiology, and otolaryngology.
Other authoritative sources provide a similar financial outlook, though the numbers can differ slightly based on their methodology (e.g., self-reported data vs. employer-posted data).
- Doximity's 2023 Physician Compensation Report places the average urologist salary at $514,931. Doximity's data is highly regarded as it's drawn from a massive survey of over 190,000 U.S. physicians.
- Salary.com, which aggregates real-time employer-reported data, shows a median urologist salary of $433,634 as of late 2023, with a typical range falling between $380,483 and $504,010. It's important to note that this range often excludes bonuses and other incentives, which can be substantial.
- Merritt Hawkins, a leading physician search firm, reports in their 2023 review that the *starting* salary range offered to urologists is between $350,000 and $700,000, showcasing the high demand right out of residency.
### Salary Brackets by Experience Level
A physician's salary is not static; it evolves significantly throughout their career. A urologist's income trajectory is steep, with earnings growing rapidly after the initial years of practice as they build their reputation, patient base, and surgical efficiency.
Here is a representative breakdown of potential earnings by career stage, synthesized from industry data:
| Career Stage | Years of Experience | Typical Salary Range (Base + Bonus) | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level/Early Career | 0-5 years | $350,000 - $450,000 | Post-residency/fellowship. Often includes a guaranteed salary for the first 1-2 years before transitioning to a productivity-based model. Focus is on building a practice and gaining speed/efficiency. |
| Mid-Career | 6-20 years | $450,000 - $650,000+ | Peak earning years. The urologist has a well-established practice, a strong referral network, and high surgical volume. Many achieve partnership in a private practice during this time, leading to higher income potential. |
| Senior/Late Career | 21+ years | $400,000 - $600,000+ | Earnings may plateau or slightly decline as some urologists choose to reduce their surgical caseload or on-call responsibilities. However, many highly experienced surgeons remain top earners well into their 60s. |
### Dissecting the Compensation Package: More Than Just a Salary
A urologist's total compensation is a package that extends far beyond their base salary. For many, especially those in private practice or hospital-employed positions, a significant portion of their income is variable and tied to productivity.
- Base Salary: This is the guaranteed annual income. In many hospital-employed models or academic positions, this forms the bulk of the compensation. In private practice, it might be a lower figure, with the majority of earnings coming from productivity bonuses.
- Productivity Bonuses (RVUs): This is the most common form of incentive compensation. The system is based on Relative Value Units (RVUs), a measure set by Medicare to value the work involved in a physician's service. Every patient encounter, procedure, and surgery has an RVU value. Urologists are often paid a certain dollar amount per RVU generated above a set threshold. Because urology is a procedure-heavy specialty, the potential for high RVU generation is immense, directly driving up income. A complex robotic surgery can generate many times more RVUs than a simple office visit.
- Performance & Quality Bonuses: An increasing number of health systems are tying a portion of compensation to quality metrics, such as patient satisfaction scores, adherence to clinical guidelines, and positive patient outcomes. While typically a smaller part of the package (e.g., 5-10%), this is a growing trend.
- Ancillary Service Revenue (Private Practice): Partners in a private urology group may share in the profits from in-house services like pathology (from prostate biopsies), advanced imaging, or an in-office ambulatory surgery center. This can be a significant source of additional income.
- Standard Benefits Package: Like other highly skilled professionals, urologists receive a robust benefits package, which must be factored into the total compensation picture.
- Medical Malpractice Insurance: Crucial for a surgical specialty, this is almost always fully covered by the employer and can be worth tens of thousands of dollars per year.
- Health, Dental, and Vision Insurance: Comprehensive family plans are standard.
- Retirement Plans: Generous 401(k) or 403(b) plans, often with a significant employer match or profit-sharing component.
- Continuing Medical Education (CME) Allowance: A stipend of $5,000 - $15,000 per year to cover costs for conferences, journals, and courses needed to maintain medical licensure.
- Paid Time Off (PTO): Typically 4-6 weeks of vacation time, plus additional time for CME.
- Relocation Allowance / Signing Bonus: Often offered to new hires, signing bonuses can range from $20,000 to $100,000+ to attract talent to a specific location or practice.
Key Factors That Influence Urologist Salary

While the national averages provide a strong benchmark, a urologist's individual earning potential is influenced by a complex interplay of several key factors. Understanding these variables is critical for any aspiring urologist looking to maximize their career and financial trajectory. Two urologists with identical training can have vastly different incomes based on where and how they choose to practice.
### 1. Geographic Location
Geography is one of the most powerful drivers of physician compensation. The salary for a urologist can vary by more than $100,000 per year simply based on the state or metropolitan area in which they practice. This variation is driven by supply and demand, cost of living, and the local healthcare market dynamics.
Generally, salaries tend to be higher in the Southeast, Midwest, and less-populated regions where there is a greater need to attract and retain specialized physicians. Conversely, salaries may be lower in major metropolitan areas on the East and West Coasts (e.g., Boston, New York City, San Francisco, Los Angeles), where there is a higher concentration of physicians and academic medical centers.
Examples of High-Paying vs. Lower-Paying Regions (based on aggregated data from Medscape, Doximity, and Merritt Hawkins):
- Top-Paying States/Regions:
- The Southeast: States like Alabama, Georgia, and Florida often report some of the highest urology salaries, driven by high patient demand (including an aging population) and favorable practice environments.
- The Midwest: States such as Wisconsin, Indiana, and North Dakota consistently offer lucrative compensation packages to attract specialists away from the coasts. A 2023 Doximity report highlighted Wisconsin as a top state for physician compensation growth.
- Rural & Underserved Areas: Practices in non-metropolitan areas across the country almost always offer higher salaries and signing bonuses as a direct incentive to fill a critical community need.
- Lower-Paying (but still high) States/Regions:
- The Northeast: States like Maryland, Massachusetts, and Virginia tend to be on the lower end of the urology salary spectrum. This is often due to a higher density of urologists, a greater prevalence of academic positions (which traditionally pay less than private practice), and dominant insurance payers with less favorable reimbursement rates.
- The West Coast: While the cost of living is high, salaries in states like California may not always keep pace, especially in saturated markets like Los Angeles and the Bay Area.
It's crucial to analyze salary data in the context of cost of living. A $550,000 salary in rural Wisconsin may provide a much higher quality of life and greater wealth-building potential than a $500,000 salary in San Diego.
### 2. Practice Setting and Ownership Model
The type of environment where a urologist works has a profound impact on their compensation structure and overall earning potential.
- Private Practice (Physician-Owned): This model traditionally offers the highest income potential.
- Single-Specialty Group: A group of only urologists. This is the most common private practice model in urology. After an initial 1-2 year "partnership track" on a guaranteed salary, a urologist becomes a partner. As a partner, they share in the practice's overhead but also its profits, including revenue from ancillary services. Business acumen is key to success.
- Multi-Specialty Group: A large practice with physicians from various specialties (e.g., primary care, oncology, radiology). This model can provide a strong, built-in referral base, but may offer slightly less autonomy than a single-specialty group.
- Hospital or Health System Employment: This is the fastest-growing employment model for physicians. The urologist is a direct employee of the hospital.
- Pros: Offers stability, predictable hours (relative to private practice), a guaranteed salary, and excellent benefits. The hospital handles all administrative burdens like billing, staffing, and marketing.
- Cons: Lower top-end earning potential compared to a successful private practice partner. There is less autonomy over practice decisions and scheduling. Compensation is heavily reliant on the productivity (RVU) model set by the hospital.
- Academic Medical Centers: Urologists at universities and teaching hospitals are involved in a "tripartite mission": clinical care, research, and teaching medical students and residents.
- Pros: Prestige, opportunities to engage in cutting-edge research, teaching the next generation, and managing the most complex cases referred from the region.
- Cons: Salaries are almost always lower than in private practice or even general hospital employment. A significant portion of time is dedicated to non-revenue-generating activities like research and education, which is reflected in the lower clinical pay.
- Locum Tenens: This involves working as a temporary, independent contractor to fill in for other urologists who are on vacation, leave, or to cover staffing shortages.
- Pros: Extremely high daily or weekly pay rates. Offers flexibility in scheduling and location.
- Cons: No benefits, no job security, and constant travel. It's not a long-term career path for most but can be a lucrative option for urologists between permanent jobs or nearing retirement.
### 3. Subspecialization and Fellowship Training
After completing a 5-6 year urology residency, physicians can choose to pursue further subspecialty training through a 1-3 year fellowship. This advanced expertise can significantly enhance earning potential by enabling them to perform more complex, higher-reimbursed procedures.
- Urologic Oncology: 2-3 year fellowship focusing on the surgical and medical management of urologic cancers. These surgeons tackle the most complex cases (e.g., robotic cystectomy with neobladder reconstruction) and are among the highest earners in the field.
- Pediatric Urology: 2-year fellowship to treat urologic issues in children, from birth defects to tumors. This is a highly specialized and in-demand field.
- Female Pelvic Medicine and Reconstructive Surgery (FPMRS): Also known as Urogynecology, this 2-3 year fellowship focuses on issues like severe incontinence and pelvic organ prolapse. It involves complex reconstructive surgeries.
- Andrology / Male Infertility: 1-2 year fellowship focusing on male reproductive health, including erectile dysfunction and surgical procedures for infertility (e.g., microscopic vasectomy reversal).
- Endourology and Robotic Surgery: 1-2 year fellowship to master advanced, minimally invasive techniques for treating kidney stones, BPH, and cancers. Expertise in robotics is particularly valuable.
While a general urologist can have a very successful career, those with fellowship training are often sought after by academic centers and large specialty groups to serve as the local or regional expert, commanding higher salaries and referral volumes.
### 4. High-Value Skills and Procedural Expertise
In a surgical field, "you eat what you kill." A urologist's income is directly tied to the procedures they perform. Developing expertise in high-RVU (and thus, high-reimbursement) procedures is the most direct way to increase earnings.
- Robotic Surgery Proficiency: Expertise with the da Vinci® Surgical System is no longer a niche skill; it is the standard of care for many procedures, especially prostatectomies. Surgeons who are highly efficient and have excellent outcomes with robotic surgery are invaluable assets and top earners.
- Complex Cancer Surgery: The ability to perform radical cystectomies, partial nephrectomies for complex tumors, and retroperitoneal lymph node dissections places a urologist in the top tier of the specialty.
- Advanced Reconstructive Surgery: Skills in creating neobladders, repairing urethral strictures, or performing complex ureteral reconstruction are highly specialized and well-compensated.
- Business Acumen (for Private Practice): For those on a partnership track, understanding the business side of medicine—billing codes, overhead management, marketing, and contract negotiation—is a skill that directly translates to higher personal income.
Job Outlook and Career Growth for Urologists

The long-term career outlook for urologists is exceptionally strong. While the U.S. Bureau of Labor Statistics (BLS) projects a 3% job growth for all physicians and surgeons between 2022 and 2032—about as fast as the average for all occupations—this general figure does not capture the specific, powerful tailwinds driving demand for urology.
The primary driver is demographics. The aging of the U.S. population, particularly the massive Baby Boomer generation moving into their 60s, 70s, and 80s, is creating a "perfect storm" of demand for urologic care. The incidence of key urologic conditions rises dramatically with age:
- Benign Prostatic Hyperplasia (BPH): Affects about 50% of men in their 50s and up to 90% of men in their 80s.
- Prostate Cancer: The most common non-skin cancer in men, with risk increasing significantly after age 50.
- Bladder Cancer: Primarily a disease of older adults, with the average age of diagnosis being 73.
- Urinary Incontinence: Becomes more prevalent with age, especially in women.
- Kidney Stones: While they can affect all ages, prevalence increases with age.
Simultaneously, the supply of urologists is not keeping pace with this rising demand. A 2021 report from the American Urological Association (AUA) highlighted a looming workforce shortage, noting that a significant portion of the current urology workforce is approaching retirement age. This growing gap between supply and demand places newly trained urologists in a very strong negotiating position and ensures robust job security for the foreseeable future.
### Emerging Trends and Future Challenges
The field of urology is not static. It is constantly evolving with technological and medical advancements. To stay relevant and successful, urologists must adapt to these trends.
Key Trends:
- Expansion of Minimally Invasive Techniques: The shift from open surgery to robotic and laparoscopic procedures will continue. Expertise in these areas will be paramount.
- Advances in Urologic Oncology: The integration of immunotherapy, targeted therapies, and genomic testing is changing cancer care. Urologists will need to work closely with medical oncologists and stay abreast of these developments.
- Telehealth Integration: While not suitable for surgery, telehealth has found a firm place in urology for follow-up appointments, initial consultations, and management of chronic conditions, improving practice efficiency and patient access.
- Focus on Men's Health: There is a growing movement to treat men's health holistically, with urology at the center. This includes not just prostate health and ED, but also a focus on testosterone deficiency, cardiovascular risk, and preventative care.
Future Challenges:
- Physician Burnout: The high demands of the job, long hours, and administrative burdens (such as electronic health records and prior authorizations from insurance companies) are leading to high rates of burnout across all of medicine, and urology is no exception.
- Reimbursement Pressures: Declining reimbursement rates from Medicare and private insurers are a constant challenge, forcing practices to see more patients and become more efficient to maintain revenue.
- Consolidation of Healthcare: The trend of private practices being acquired by large hospital systems or private equity firms continues. This can lead to a loss of autonomy for physicians.
Advice for Career Advancement and Longevity:
- Embrace Lifelong Learning: The field changes rapidly. Consistently attend conferences, participate in workshops (especially for new surgical techniques), and read journals to stay at the cutting edge.
- Develop a Niche: While a general urology practice is viable, developing a reputation