Introduction

Choosing a career in medicine in the United Kingdom is a decision driven by a profound desire to help others, a fascination with the complexities of the human body, and the pursuit of a profession that commands respect and offers lifelong learning. It is a calling, a commitment that demands immense dedication, resilience, and intellectual rigour. But alongside this calling, there's a practical and entirely valid question that every aspiring doctor, their family, and even current trainees ask: "What is a British doctor's salary?"
The answer is far from simple. A doctor's earnings in the UK are not a single figure but a complex tapestry woven from years of experience, specialisation, location, and the significant distinction between working for the National Health Service (NHS) and practising privately. The journey begins with a modest salary as a junior doctor, laden with student debt, and can culminate in a six-figure income as a senior consultant or a successful General Practitioner (GP). For the 2023-24 period, the basic salary for a newly qualified doctor starts at £32,398, while experienced consultants can earn a basic salary of up to £126,281 within the NHS, with significant potential for additional earnings.
I remember sitting in a hospital waiting room, my family anxiously awaiting news about a loved one. The calm, compassionate authority of the consultant who finally came to speak with us was a beacon of hope in a moment of fear. It wasn't just her medical knowledge that was impactful; it was the trust she inspired. This career is about being that beacon, and understanding the financial framework that supports such a vital role is crucial for anyone considering this demanding yet incredibly rewarding path.
This comprehensive guide will demystify the financial landscape of a medical career in the UK. We will dissect the NHS pay scales, explore the factors that dictate earning potential, and provide a clear, step-by-step roadmap for those standing at the start of their journey.
### Table of Contents
- [What Does a British Doctor Do?](#what-does-a-british-doctor-do)
- [Average British Doctor Salary: A Deep Dive](#average-british-doctor-salary-a-deep-dive)
- [Key Factors That Influence a Doctor's Salary](#key-factors-that-influence-a-doctors-salary)
- [Job Outlook and Career Growth for UK Doctors](#job-outlook-and-career-growth-for-uk-doctors)
- [How to Become a Doctor in the UK: A Step-by-Step Guide](#how-to-become-a-doctor-in-the-uk-a-step-by-step-guide)
- [Conclusion: Is a Career in Medicine Worth It?](#conclusion-is-a-career-in-medicine-worth-it)
---
What Does a British Doctor Do?
The title "doctor" in the UK encompasses a vast range of roles and responsibilities, but they are broadly categorised into two main pathways: General Practitioners (GPs) and hospital doctors (who work in various specialities). While both are dedicated to patient care, their daily work environments, tasks, and long-term career structures are distinctly different.
General Practitioners (GPs) are the cornerstone of community-based healthcare and the first point of contact for most patients within the NHS. They are expert generalists, trained to diagnose, treat, and manage a wide spectrum of illnesses and health concerns for patients of all ages. Their work is incredibly varied, ranging from treating acute infections and minor injuries to managing chronic conditions like diabetes and heart disease, providing vaccinations, and offering mental health support. A GP's role extends beyond clinical duties; most GPs work as independent contractors to the NHS, meaning they are often partners or salaried employees in a GP practice, which involves business management, staff supervision, and financial planning.
Hospital Doctors work within specific medical or surgical specialities in a hospital setting. Their career path is more structured, progressing through a rigorous training programme to eventually become a senior 'Consultant'. Their work is focused on a particular area of medicine, such as cardiology, oncology, paediatrics, or general surgery. A hospital doctor's responsibilities include attending ward rounds to review admitted patients, running outpatient clinics for specialist consultations, performing surgical procedures or medical interventions, interpreting complex diagnostic tests, and collaborating with a large multidisciplinary team of nurses, therapists, and other specialists. They also play a vital role in teaching junior doctors and medical students and are often involved in clinical research.
### A Day in the Life of a British Doctor
To make these roles more tangible, let's consider two typical days:
A Day in the Life of a GP (Dr. Evans):
- 8:00 AM: Arrives at the surgery. Reviews urgent blood test results and hospital letters that have come in overnight, actioning anything critical.
- 8:30 AM - 11:30 AM: Morning surgery. Sees a new patient every 10-15 minutes. Today's list includes a child with an ear infection, an elderly man for his annual diabetes review, a woman concerned about a skin lesion, and a young professional struggling with anxiety.
- 11:30 AM - 1:00 PM: "Admin time." Signs repeat prescriptions, dictates referral letters to specialists, and makes phone calls to patients to discuss test results. Has a quick meeting with the practice manager about finances.
- 1:00 PM - 2:00 PM: Lunch, often eaten at the desk. Makes a couple of home visits to housebound elderly patients.
- 2:00 PM - 5:00 PM: Afternoon surgery. Another series of varied patient consultations.
- 5:00 PM - 6:30 PM (or later): Finishes patient-related paperwork, reviews the day's tasks, and prepares for the next day. The work often extends well beyond the official closing time.
A Day in the Life of a Hospital Surgical Registrar (Dr. Khan):
- 7:30 AM: Arrives at the hospital for the pre-operative ward round. Sees all patients scheduled for surgery today, answers their last-minute questions, and ensures they have signed consent forms.
- 8:30 AM: Team briefing in the operating theatre with the consultant surgeon, anaesthetist, and nursing team to run through the day's operating list.
- 9:00 AM - 1:00 PM: In theatre. Assists the consultant in a complex bowel cancer resection. The registrar performs parts of the operation under direct supervision, honing their surgical skills.
- 1:00 PM - 1:30 PM: A quick lunch break in the hospital canteen.
- 1:30 PM - 5:00 PM: Post-operative ward round. Checks on patients from the morning's list and other post-op patients on the ward, adjusting pain relief and fluid plans. Responds to any urgent calls ("bleeps") from the ward nurses about unwell patients.
- 5:00 PM - 6:00 PM: Handover. Meets with the on-call team to provide a detailed summary of all the patients on the ward, highlighting anyone who is unstable or needs close monitoring overnight.
- 6:00 PM onwards: Catches up on administrative tasks like updating patient notes and dictating discharge summaries. If on-call, the shift could continue through the night, dealing with emergency admissions and critical patient issues.
---
Average British Doctor Salary: A Deep Dive

A doctor's salary in the UK is highly structured, especially within the NHS, which employs the vast majority of doctors. The pay system is transparent and based on a series of national contracts negotiated between the government and doctors' unions, primarily the British Medical Association (BMA).
The progression is linear and tied directly to one's training stage and years of experience. It's crucial to understand that the "average salary" is a misleading figure because it blends the earnings of a newly qualified doctor with those of a highly experienced consultant. Instead, it's more accurate to break it down by career stage.
*All figures below are based on the latest pay scales for doctors in England for 2023/24, as published by NHS Employers and the BMA. Pay scales may differ slightly in Scotland, Wales, and Northern Ireland, but generally follow a similar structure.*
### The NHS Pay Scale: A Career-Long Journey
The journey begins immediately after graduating from medical school.
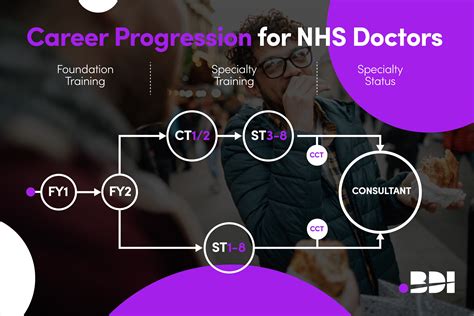
1. Foundation Training (Junior Doctors)
This is a two-year training programme for newly qualified doctors.
- Foundation Year 1 (FY1): Basic salary: £32,398. This is the first salaried role after medical school.
- Foundation Year 2 (FY2): Basic salary: £37,303. With a year of experience, the basic pay increases.
2. Specialty Training (Junior Doctors, sometimes called "Registrars")
After the Foundation Programme, doctors enter specialty training (CT/ST) which can last from three to eight years depending on the chosen field (e.g., three years for General Practice, eight years for some surgical specialities). Pay is determined by a nodal pay point system based on the years of training completed.
| Nodal Pay Point (Years of Training) | 2023/24 Basic Salary |
| :--- | :--- |
| CT1/ST1 | £43,923 |
| CT2/ST2 | £43,923 |
| ST3 | £55,329 |
| ST4 | £55,329 |
| ST5 | £55,329 |
| ST6 | £63,152 |
| ST7 | £63,152 |
| ST8 | £63,152 |
3. Specialty Doctors and Specialists (Non-Training Roles)
These are senior doctors who have completed their training but are not consultants. The specialist grade is a newer role for doctors with at least 12 years of post-graduate experience.
- Specialty Doctor (2021 contract): The pay scale ranges from £52,530 to £82,400, based on years of experience in the grade.
- Specialist Grade (2021 contract): The pay scale ranges from £83,945 to £92,275.
4. Consultants
A consultant is a senior doctor who has completed all their specialist training and been placed on the GMC's specialist register. They have ultimate clinical responsibility for their patients. The consultant contract has thresholds, with pay increasing significantly after a certain number of years of service.
| Years as Consultant | 2023/24 Basic Salary Threshold |
| :--- | :--- |
| 0-4 | £93,666 |
| 5-9 | £96,555 |
| 10-14 | £102,684 |
| 15-18 | £114,003 |
| 19+ | £126,281 |
5. General Practitioners (GPs)
GPs operate under a different model. Most are not directly salaried by the NHS. Instead, their practice receives funding from the NHS based on its patient list size and other factors. From this funding, the practice pays its expenses (staff, building, utilities), and the remaining profit is distributed among the partners.
- Salaried GPs: These are GPs employed by the practice. According to the BMA, the recommended salary range for a salaried GP is £68,975 to £104,085, depending on experience and responsibilities.
- GP Partners: These GPs are co-owners of the practice and their income is a share of the profits. This can be highly variable. Data from NHS Digital's "GP Earnings and Expenses" report for 2021/22 showed the average income before tax for a GP partner was £148,000. However, this comes with the significant responsibilities and financial risks of running a business.
### Beyond the Basic Salary: Other Compensation Components
A doctor's total pay packet is more than just their basic salary. Several other components contribute significantly to their final earnings:
- Pay for Additional Hours: Doctors are contracted for a standard 40-hour week. Any work beyond this is paid at an enhanced rate.
- Weekend and On-Call Allowances: Working weekends, evenings, and being on-call attracts an additional allowance, which can be a substantial portion of a junior doctor's income. For example, a junior doctor working 1 in 4 weekends with a full shift on both Saturday and Sunday could see their take-home pay increase significantly.
- London Weighting: To compensate for the significantly higher cost of living, doctors working in London and fringe areas receive a pay supplement. This is currently around £2,162 per year, but the exact amount varies by Trust.
- Locum Work: Many doctors supplement their income by working "locum" shifts. These are temporary shifts to cover gaps in the rota. Locum rates are typically much higher than salaried pay, often ranging from £50-£120 per hour depending on the specialty and urgency.
- National Clinical Impact Awards (NCIAs): Formerly known as Clinical Excellence Awards, these are prestigious and financially rewarding awards for consultants whose work is deemed to be of national significance, over and above the standard expectation. These can add between £20,000 and £40,000 per year to a consultant's salary.
- Private Practice: This is the most significant source of additional income for many consultants. By working in private hospitals outside of their NHS hours, they can earn substantial fees for consultations and procedures.
---
Key Factors That Influence a Doctor's Salary

While the NHS pay scales provide a clear and rigid framework, several key factors create significant variation in what a doctor in the UK actually earns. Understanding these nuances is essential for grasping the full financial picture of a medical career.
### 1. Years of Experience and Training Stage
This is the single most dominant factor within the NHS system. As demonstrated in the tables above, a doctor's salary is explicitly tied to their progression through a long and arduous training pathway.
- The Early Years (Foundation & Core Training): The first 4-5 years post-graduation are characterised by relatively modest salaries when considering the level of responsibility and debt accrued. A doctor in their first year (FY1) earns a basic of £32,398. After four years, upon entering ST3, this jumps to £55,329. While these salaries are supplemented by on-call and weekend work, they reflect a trainee status. The focus during this period is on acquiring a broad base of skills, not maximising income.
- The Registrar Years (Higher Specialty Training): From ST3 onwards, doctors are "registrars" with increasing autonomy. Their basic salary rises in increments, reaching £63,152 in the final years of training (ST6+). At this stage, many doctors are in their early to mid-thirties, and this salary level, while respectable, can feel constrained, especially when compared to peers in finance or law who have been earning at a high level for years. This is a key reason many registrars undertake locum work to supplement their income.
- The Consultant Leap: The most significant financial jump in an NHS hospital career occurs upon achieving the Certificate of Completion of Training (CCT) and securing a consultant post. The starting basic salary for a new consultant (£93,666) is a near 50% increase from a senior registrar's salary. The salary then continues to increase with experience, crossing the £100k threshold after 10 years and reaching a peak of £126,281 after 19 years of service as a consultant. This long-term, predictable growth is a hallmark of the NHS consultant contract.
### 2. Area of Specialization
The choice of specialty has a profound impact on earning potential, primarily through the opportunities for private practice and the nature of the work itself.
- General Practice (GP): As outlined, becoming a GP Partner offers one of the highest earning potentials within the NHS system. The average earnings of £148,000 (before tax) for a partner surpasses the peak basic NHS consultant salary. However, this comes with the immense pressure and financial risk of running a small business, managing staff, and being responsible for the practice's budget.
- High-Earning Hospital Specialities (via Private Practice): Certain specialties have a much more lucrative private sector market. These are typically procedure-based fields where patients are willing and able to pay for faster access or specific surgeons. Examples include:
- Plastic Surgery: Particularly cosmetic procedures.
- Orthopaedic Surgery: Especially joint replacements (hip, knee).
- Cardiology: Particularly interventional procedures like stenting.
- Ophthalmology: Cataract surgery is a high-volume private procedure.
- Dermatology: Private consultations for skin conditions and cosmetic dermatology.
A consultant in one of these fields might work their 40 hours (10 Programmed Activities) in the NHS and then run private clinics and operating lists one or two days a week. Private consultation fees can range from £200-£400, and surgical procedures can cost patients thousands of pounds, from which the surgeon takes a significant fee. This can easily double a consultant's total income, pushing their earnings well into the £200,000 - £300,000+ range.
- Lower-Earning Hospital Specialities (Less Private Work): Conversely, some crucial specialities have a much smaller private market. These are often fields that deal with acute, non-elective emergencies or are intrinsically tied to the NHS infrastructure.
- Emergency Medicine: Almost exclusively NHS-based.
- Palliative Care: Largely provided through the NHS or charitable hospices.
- Geriatric Medicine: While some private geriatricians exist, the majority of complex elderly care happens within the NHS.
- Most areas of Pathology and Histopathology.
Consultants in these fields are highly respected and essential, but their total earnings are more likely to be confined to their NHS salary plus any awards or management roles, as significant private practice income is less common.
### 3. Geographic Location
Where a doctor chooses to work in the UK can have a direct, albeit relatively minor, impact on their contracted salary, but a major impact on their disposable income.
- London Weighting: The only formal geographic pay supplement is the "London Weighting". As per the BMA, this is a payment to compensate for the high cost of living in the capital. All NHS doctors working in inner, outer, or fringe areas of London receive an additional payment. For example, a doctor working in an Inner London trust might receive an extra £2,162 per year.
- The Cost-of-Living Equation: While the London weighting provides a small uplift, it barely touches the sides of the vastly higher costs of housing, transport, and general living in London compared to other parts of the UK. A consultant earning £100,000 in London may have significantly less disposable income than a consultant on the same salary in Manchester, Cardiff, or Glasgow. This is a critical consideration for doctors planning their careers and lives.
- Devolved Nations: While the pay scales in Scotland, Wales, and Northern Ireland are very similar to England's, there can be minor differences arising from separate negotiations with their respective governments. For example, in recent years, Scotland has sometimes offered slightly better pay awards than England, although the core structure remains the same.
### 4. Employment Type: NHS vs. Private Practice vs. Locum
This is arguably the second most important factor after experience. The traditional model is a permanent contract with an NHS Trust, but alternatives offer greater flexibility and earning potential.
- NHS Salaried (The Standard Path): The vast majority of doctors work on a permanent, salaried NHS contract. This offers immense job security, a generous pension scheme (one of the best available in the UK), sick pay, and maternity/paternity leave. The trade-off is a contractually defined salary and a rigid work structure.
- Private Practice (The Income Multiplier): Working in the private sector is not typically a full-time alternative but an addition to an NHS role. Most consultants with a successful private practice hold a part-time NHS contract (e.g., 6-8 Programmed Activities instead of 10) to free up time. The income is limited only by patient demand, the doctor's reputation, and the rates they can charge. It requires business acumen, marketing, and managing relationships with private hospitals and insurers.
- Locum Doctor (The Flexibility & High Rate Option): A locum doctor is essentially a freelance professional. They work temporary shifts to fill rota gaps, cover leave, or help with periods of high demand. Locum agencies connect doctors with hospitals. The primary benefits are flexibility (choosing when and where to work) and significantly higher hourly pay rates. A senior registrar might earn £30/hour in their NHS job but command £70-£90/hour for a locum shift. A consultant could earn £100-£150/hour. The downsides are a lack of job security, no sick pay or pension contributions (unless managed privately), and the administrative burden of managing one's own taxes and finances. For many doctors, a period of locum work is a way to save money quickly, travel, or gain experience in different hospitals before settling into a permanent post.
### 5. Additional Roles and Responsibilities
Within the NHS, there are structured ways for senior doctors to increase their earnings by taking on non-clinical responsibilities.
- Management Positions: Consultants can take on leadership roles that come with additional pay. A Clinical Lead might oversee a department, while a Clinical Director might manage a whole directorate (e.g., all of surgery). A Medical Director sits on the hospital's executive board and is one of the most senior medical roles in a Trust. These roles carry additional "Programmed Activities" (PAs) in their contract, directly increasing their salary.
- Teaching and Academia: Doctors who are heavily involved in teaching medical students or formal university research often have joint contracts between the NHS and a university. This can come with the title of Senior Lecturer, Reader, or Professor, and an associated academic salary uplift.
- National Clinical Impact Awards (NCIAs): As mentioned, these awards are a significant source of extra income for the UK's top consultants. They are competitive and awarded to those who can demonstrate a major impact on clinical services, research, or medical education at a national level.
---
Job Outlook and Career Growth for UK Doctors
The career outlook for doctors in the United Kingdom is a complex picture of high demand, significant challenges, and evolving practice. While the profession offers exceptional job security, it is also operating under considerable strain, a factor that aspiring doctors must consider.
### High Demand and Job Security
The demand for doctors in the UK consistently outstrips supply. An ageing population with increasingly complex health needs, coupled with ongoing recruitment and retention challenges within the NHS, means that qualified doctors have near-guaranteed employment. The NHS Long Term Workforce Plan, published in June 2023, is the government's strategy to address these shortfalls. It highlights the scale of the challenge, projecting a potential workforce shortfall of between 260,000 and 360,000 staff by 2036/37 if no action is taken.
This fundamental imbalance ensures that from the moment of graduation, a doctor's skills are in high demand. The structured training pathway means there is a clear, mapped-out career progression from Foundation Doctor to Consultant or GP. Unlike many other professions, there is virtually no risk of redundancy or unemployment for a competent doctor willing to work in the UK.
### Current Challenges Facing the Profession
Despite high demand, the profession faces significant headwinds that impact morale and working conditions:
1. Workforce Strain and Burnout: Years of underfunding, exacerbated by the COVID-19 pandemic, have placed immense pressure on the medical workforce. Doctors frequently report working in understaffed environments, covering rota gaps, and dealing with unsustainable workloads. This has led to high rates of burnout, a key driver behind doctors leaving the profession or reducing their hours.
2. Pay Erosion and Industrial Action: A major point of contention has been the erosion of pay in real terms over the last decade. The BMA calculates that since 2008, pay for junior doctors has been cut by over 26% and for consultants by over 35% when accounting for inflation. This has been the primary driver behind the recent waves of industrial action (strikes) by both junior doctors and consultants, as they seek to restore the value of their pay. This ongoing dispute creates uncertainty and has impacted morale across the NHS.
3. Retention Issues: The combination of burnout, pay erosion, and difficult working conditions has led to a "leaky bucket" problem. Data from the General Medical Council (GMC) shows a concerning trend of doctors choosing to leave the UK register to practise abroad (in countries like Australia and Canada, which often offer better pay and work-life balance), take career breaks, or leave medicine altogether. Retaining experienced doctors is as big a challenge as recruiting new ones.
### Future Trends and Staying Relevant
The future of medicine in the UK will be shaped by technology, changing patient expectations, and new models of care. To thrive, doctors must be adaptable.
- The Rise of Technology: Artificial Intelligence (AI) is set to revolutionise diagnostics, particularly in fields like radiology and pathology, by helping to analyse images and data more quickly and accurately. Telemedicine and remote consultations, which surged during the pandemic, are here to stay, changing how GPs and specialists interact with patients. Doctors of the future will need to be digitally literate and able to integrate these tools into their practice.
- Focus on Integrated and Community Care: There is a major policy push to move more healthcare out of hospitals and into the community. This will increase the importance of GPs, community geriatricians, and other specialists who can manage complex conditions outside of an acute setting. This creates new career opportunities in community-based roles and leadership.
- Portfolio Careers: Increasingly, doctors are opting for "portfolio careers" rather than a single, linear path. This might involve combining a part-time NHS role with locum work, a medical education position, private practice, or even work in the life sciences or health-tech industry. This approach offers greater flexibility, variety, and control over one's work-life balance and is a way to mitigate some of the pressures of a full-time NHS role.
Advancement in the field requires more than just clinical excellence. Engaging in teaching, participating in clinical audits and research, taking on management responsibilities, and developing a sub-specialty interest are all key ways to progress towards a consultant post and distinguish oneself for senior roles and awards.
---
How to Become a Doctor in the UK: A Step-by-Step Guide

The path to becoming a fully qualified doctor in the UK is a long, highly competitive, and meticulously structured marathon. It requires academic excellence, resilience, and a deep-seated commitment from a young age. Here is the standard step-by-step journey.
Step 1: Excel at School (Age 14-18)
The journey begins with your GCSEs and A-Levels (or equivalent qualifications).
- GCSEs: You will need a strong set of results, typically with top grades (7-9 or A-A*) in Mathematics, English, and Sciences.
- A-Levels: This is the critical academic hurdle. Almost all UK
