Table of Contents

- [Introduction](#introduction)
- [What Does a Nurse in Canada Do?](#what-does-a-nurse-in-canada-do)
- [Average Nurse Salary in Canada: A Deep Dive](#average-nurse-salary-in-canada-a-deep-dive)
- [Key Factors That Influence a Nurse's Salary](#key-factors-that-influence-a-nurses-salary)
- [Job Outlook and Career Growth for Nurses in Canada](#job-outlook-and-career-growth-for-nurses-in-canada)
- [How to Become a Nurse in Canada](#how-to-become-a-nurse-in-canada)
- [Conclusion: Is a Nursing Career in Canada Right for You?](#conclusion-is-a-nursing-career-in-canada-right-for-you)
Introduction

Have you ever felt a profound calling to make a tangible difference in people's lives? To be the calm, competent presence in a moment of crisis, the advocate for a patient's well-being, and a cornerstone of a community's health? If this resonates with you, a career in nursing in Canada might be your future. It's a profession that demands intellect, empathy, and resilience in equal measure, but in return, it offers immense personal fulfillment and a stable, rewarding career path. For those of you typing "canada salary nurse" into your search bars, you're not just looking for a number; you're seeking to understand the value placed on this vital role and what a life in this profession could look like. The answer is promising: nursing in Canada is not only a respected vocation but also a financially secure one, with average salaries for Registered Nurses (RNs) often ranging from $75,000 to over $100,000 annually, depending on a host of factors we will explore in detail.
I'll never forget the quiet competence of the cardiac nurse who cared for my father after his surgery. She was more than just a medical professional; she was a communicator, an educator, and a source of profound comfort during a stressful time. Her ability to explain complex information with simple clarity and to provide care with such confident compassion solidified my understanding that nursing is truly where science and humanity intersect.
This guide is designed to be your definitive resource, moving beyond simple salary figures to give you a complete 360-degree view of the nursing profession in Canada. We will dissect the roles and responsibilities, delve into the financial data from authoritative sources, and break down every factor that influences your earning potential—from your level of education and location to your area of specialization. We'll also map out the career trajectory, explore the robust job outlook, and provide a clear, step-by-step roadmap on how to begin your journey. Whether you are a high school student considering your options, an internationally educated nurse looking to practice in Canada, or a professional considering a career change, this guide will provide the expert insights and data-driven answers you need.
What Does a Nurse in Canada Do?

To understand the value and salary of a nurse, one must first appreciate the sheer breadth and depth of their responsibilities. The role is far more dynamic and complex than the outdated stereotype of a simple caregiver. In Canada, the nursing profession is primarily composed of three regulated roles, each with a distinct scope of practice, educational requirements, and responsibilities: Licensed Practical Nurses (LPNs), Registered Nurses (RNs), and Nurse Practitioners (NPs).
Registered Nurses (RNs) form the backbone of the Canadian healthcare system. They are highly skilled professionals who have typically completed a four-year Bachelor of Science in Nursing (BScN) degree. Their scope of practice is extensive and autonomous. RNs are responsible for coordinating the comprehensive care of patients, which involves a sophisticated blend of critical thinking, clinical skills, and leadership.
Core responsibilities of an RN include:
- Comprehensive Health Assessment: Conducting detailed physical and psychosocial assessments of patients to identify health issues and plan care.
- Care Planning and Implementation: Developing, implementing, and evaluating individualized nursing care plans for patients with complex health needs.
- Administering Medications and Treatments: Safely administering a wide range of medications (including intravenous medications), managing complex wound care, and performing other advanced treatments as prescribed.
- Operating and Monitoring Medical Equipment: Using sophisticated medical technology, such as cardiac monitors, ventilators, and infusion pumps.
- Patient and Family Education: Educating patients and their families about health conditions, treatment plans, and preventative health strategies.
- Leadership and Collaboration: Leading and supervising other healthcare staff, including LPNs and personal support workers, and collaborating with physicians, therapists, and other members of the interdisciplinary health team.
- Advocacy: Acting as a powerful advocate for patients' rights, safety, and health needs within the healthcare system.
Licensed Practical Nurses (LPNs), known as Registered Practical Nurses (RPNs) in Ontario, are also vital members of the healthcare team. They typically complete a two-year diploma program. While their scope is more focused than an RN's, it is no less important. LPNs provide care to patients with less complex needs and work under the direction or in collaboration with RNs and physicians. Their work often involves performing health assessments, administering medications (with some restrictions compared to RNs), providing wound care, and monitoring patient health status.
Nurse Practitioners (NPs) are RNs who have pursued advanced education at the Master's or Doctoral level. They possess an expanded scope of practice that includes duties traditionally performed by physicians. NPs can autonomously diagnose and treat illnesses, order and interpret diagnostic tests, prescribe medications, and manage chronic diseases. They are leaders in the healthcare system, often running their own clinics and providing comprehensive primary care.
### A Day in the Life of a Hospital-Based RN
To make this tangible, let's walk through a hypothetical day for an RN on a busy medical-surgical floor:
- 7:00 AM: Arrive and receive a detailed handover report from the night shift nurse on a caseload of 4-5 patients. This involves understanding recent changes in condition, new orders, and outstanding tasks.
- 7:30 AM: Begin the first round of patient assessments. This isn't just taking vital signs; it's a head-to-toe check, assessing pain levels, checking IV sites, evaluating surgical wounds, and, most importantly, talking to the patients to gauge their status.
- 9:00 AM: Medication administration time. This requires meticulous attention to detail—checking dosages, patient allergies, and potential drug interactions for multiple patients simultaneously.
- 10:30 AM: A patient's blood pressure suddenly drops. The RN immediately assesses the patient, initiates protocols, pages the physician with a concise SBAR (Situation, Background, Assessment, Recommendation) report, and administers ordered fluids.
- 12:00 PM: Charting. Documentation is a critical and time-consuming legal responsibility. Every assessment, intervention, and patient response must be accurately recorded.
- 1:00 PM: Coordinate with the interdisciplinary team. The RN speaks with a physiotherapist about a patient's mobility goals, discusses a new diet order with a dietitian, and works with a social worker to plan a patient's discharge.
- 2:30 PM: Patient and family education. The RN spends time with a newly diagnosed diabetic patient, teaching them how to administer insulin and check their blood sugar levels before they are discharged.
- 4:00 PM: Prepare for the next shift. Another round of assessments and medication administration.
- 6:30 PM: Prepare a detailed handover report for the incoming evening shift nurse, ensuring a safe and seamless transition of care.
- 7:00 PM: Final documentation check before heading home, already thinking about the patients and their progress.
This snapshot reveals that a nurse's day is a high-stakes balancing act of clinical expertise, critical thinking, time management, and profound human connection. This demanding and multifaceted nature is precisely why the profession commands respect and a competitive salary.
Average Nurse Salary in Canada: A Deep Dive
When analyzing nurse salaries in Canada, it's essential to look beyond a single national average. Compensation is highly structured, often dictated by public-sector union contracts, and varies significantly based on the nurse's designation (LPN, RN, NP), years of experience, and province of employment. Here, we'll provide a detailed breakdown using data from authoritative Canadian sources like Job Bank Canada, Statistics Canada, and reputable salary aggregators.
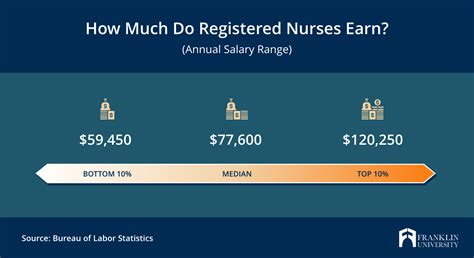
According to the Government of Canada's Job Bank, the median hourly wage for a Registered Nurse (NOC 31301) in Canada is approximately $40.00 per hour. This translates to a median annual salary of roughly $83,200 for a standard full-time work year (40 hours/week). However, this is just the midpoint. The wage spectrum is wide, with the low end for new graduates starting around $30.00 per hour and the high end for experienced, specialized, or senior nurses reaching well over $52.00 per hour. [Source: Job Bank Canada, 2023-2024 data].
It's crucial to understand that many full-time hospital nurses work 37.5-hour weeks, and their base salary is often just one part of their total compensation.
### Salary by Nursing Designation
The most significant initial factor in salary is the nursing role itself. The educational investment directly correlates with earning potential.
| Nursing Designation | Typical Education | Median Hourly Wage (Approx.) | Median Annual Salary (Approx.) | Sources |
| ------------------------------ | --------------------------- | ------------------------------ | -------------------------------- | ------------------------------------------------------------------------------ |
| Licensed Practical Nurse (LPN/RPN) | 2-year Diploma | $28.00 - $32.00 | $58,240 - $66,560 | Job Bank Canada, Payscale Canada |
| Registered Nurse (RN) | 4-year Bachelor's (BScN) | $40.00 - $44.00 | $83,200 - $91,520 | Job Bank Canada, Statistics Canada |
| Nurse Practitioner (NP) | Master's Degree (MN-NP) | $55.00 - $65.00 | $114,400 - $135,200 | Job Bank Canada, Glassdoor Canada |
*Note: Annual salaries are calculated based on a 40-hour work week for comparison purposes. Actual take-home pay will vary based on hours worked, overtime, and other factors.*
### Salary Growth by Experience Level (Registered Nurse)
Unlike many professions where salary is negotiated individually, RN salaries in unionized environments (which includes the vast majority of hospitals) increase in predictable, contractually obligated "steps" based on years of service. A nurse with eight years of experience will automatically earn more than a nurse with two years of experience in the same position.
Here is a representative salary progression for an RN in a unionized hospital setting:
- Entry-Level / New Graduate (Year 1):
- Hourly Wage: $34.00 - $39.00
- Annual Salary: ~$70,720 - $81,120
- New graduates start at the first step of the pay grid.
- Mid-Career (5-8 Years of Experience):
- Hourly Wage: $42.00 - $48.00
- Annual Salary: ~$87,360 - $99,840
- By this stage, an RN has progressed through several steps of the pay grid and has developed significant clinical competence.
- Senior / Experienced (10+ Years of Experience):
- Hourly Wage: $49.00 - $55.00+
- Annual Salary: ~$101,920 - $114,400+
- At this level, RNs are at or near the top of the standard pay scale. Further increases may come from taking on specialized roles (e.g., Clinical Nurse Educator), leadership positions (e.g., Charge Nurse, Manager), or from general cost-of-living adjustments negotiated by the union.
[Source: Analysis based on publicly available nursing union collective agreements in provinces like Ontario (ONA), British Columbia (BCNU), and Alberta (UNA)].
### Deconstructing the Compensation Package: Beyond the Base Salary
A nurse's base salary is only part of the story. The total compensation package in Canada is often significantly higher due to a variety of premiums and benefits, particularly in 24/7 hospital environments.
- Shift Premiums: Nurses receive extra pay for working undesirable hours. This is a standard feature of collective agreements.
- Evening Shift Premium: Typically an extra $2.00 - $3.00 per hour.
- Night Shift Premium: Can range from $3.50 - $5.50 per hour.
- Weekend Premium: An additional premium, often around $2.50 - $4.00 per hour, for all hours worked on a Saturday or Sunday.
- Overtime Pay: Work performed beyond the standard full-time hours is paid at a premium rate, typically 1.5x the regular hourly rate ("time and a half") and sometimes 2.0x ("double time") for excessive hours or work on a statutory holiday. Given the current nursing shortages, overtime is unfortunately common and can substantially increase annual earnings.
- Charge Nurse / In-Charge Pay: An RN who is designated as the "Charge Nurse" for a shift, taking on leadership and coordination responsibilities for the unit, receives an additional hourly premium (e.g., an extra $2.00 - $3.00 per hour).
- Specialty Certification Pay: Some collective agreements provide an annual or hourly bonus for nurses who hold and maintain advanced certifications in specialty areas like critical care (CCN), emergency (CEN), or perioperative nursing (CPN).
- Comprehensive Benefits Package: This is a major component of compensation in the public sector. It almost always includes:
- Pension Plan: Excellent defined-benefit pension plans (e.g., HOOPP in Ontario) are a significant long-term financial benefit.
- Health and Dental Insurance: Robust coverage for prescription drugs, dental care, vision care, physiotherapy, and more.
- Disability and Life Insurance: Short-term and long-term disability coverage provides income security in case of illness or injury.
- Paid Time Off: Generous vacation allowances that increase with years of service, plus paid sick days and statutory holidays.
When these additional components are factored in, a senior, full-time RN working a mix of shifts in a hospital can easily see their total compensation exceed their base salary by 15-25% or more.
Key Factors That Influence a Nurse's Salary
While experience and designation set the foundation, several other key factors create the significant salary variance seen across the country. Understanding these variables is critical for anyone planning a nursing career in Canada, as your choices can directly impact your earning potential by tens of thousands of dollars per year.
### `
` Level of Education & Advanced Certification
Education is the single most powerful lever for increasing a nurse's salary ceiling. The progression is clear and substantial.
- Diploma vs. Bachelor's Degree: The primary distinction is between an LPN (diploma) and an RN (degree). As shown in the previous section, an RN with a four-year BScN degree earns, on average, 30-40% more per hour than an LPN with a two-year diploma. This reflects the RN's broader scope of practice, increased autonomy, and greater responsibility for complex patient care. Many LPNs eventually "bridge" to an RN program to unlock this higher earning potential.
- Master's and Doctoral Degrees: The leap to a Nurse Practitioner (NP) role, which requires a Master of Nursing (MN) or a Doctor of Nursing Practice (DNP), represents the most significant salary jump. NPs earn, on average, 25-35% more than senior RNs. Their ability to diagnose, prescribe, and manage patient care independently commands a premium salary, often ranging from $110,000 to over $140,000 annually. [Source: Glassdoor, NP Salary Canada]. Other master's-level roles, such as Clinical Nurse Specialist (CNS), Nurse Educator, or Nursing Manager, also come with significant salary increases over a staff RN position, reflecting their leadership, specialized expertise, and administrative responsibilities.
- Specialty Certifications: While a bachelor's degree gets you in the door as an RN, obtaining specialty certification from the Canadian Nurses Association (CNA) demonstrates a higher level of competency and knowledge in a specific area. There are over 20 specialties, including:
- Critical Care Nursing (CCN)
- Emergency Nursing (CEN)
- Perioperative (Operating Room) Nursing (CPN)
- Oncology Nursing (CON)
- Palliative Care Nursing (CHPCN)
While not all employers offer a direct pay premium for certification, many do. More importantly, these certifications make a nurse a far more competitive candidate for high-demand, high-acuity positions (like in the ICU or ER) which often come with more opportunities for overtime and specialized roles, indirectly boosting income.
### `
` Years of Experience
As highlighted earlier, the impact of experience is formalized and transparent in Canada's unionized healthcare sector. Nursing collective agreements contain a "pay grid" or "wage scale" with multiple steps. Each year, a nurse automatically moves to the next step, receiving a predetermined salary increase.
For example, the British Columbia Nurses' Union (BCNU) collective agreement has a 9-step grid. A new graduate starts at Step 1, and after accumulating the required hours (typically one year of full-time work), they move to Step 2, and so on, until they reach the top of the scale at Step 9.
- New Graduate (Step 1): ~$38.50/hour
- 5 Years Experience (Step 5): ~$45.00/hour
- 9+ Years Experience (Step 9): ~$50.00/hour
This structure provides a predictable and steady salary growth trajectory, rewarding loyalty and continued practice. It ensures that a nurse's growing expertise is financially recognized year after year, independent of performance reviews or individual negotiations.
### `
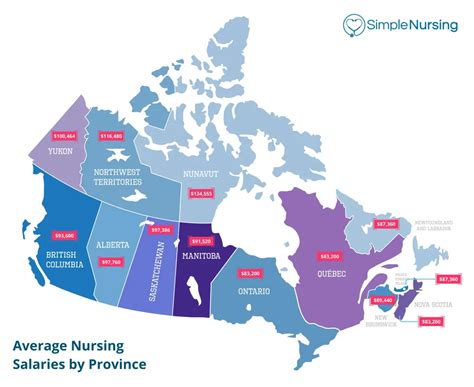
` Geographic Location: The Provincial Divide
Location is arguably the most significant factor influencing a nurse's salary in Canada. There is no national pay scale; each province and territory negotiates its own collective agreements, leading to substantial differences in pay for the exact same job.
Here is a comparative breakdown of approximate hourly wage ranges for a Registered Nurse (RN) across Canada, from highest to lowest paying regions.
| Province/Territory | Approximate RN Hourly Wage Range | Key Considerations |
| ------------------------ | ----------------------------------- | --------------------------------------------------------------------------------------------------------------------------- |
| The Territories (NU, NT, YT) | $50.00 - $70.00+ | Highest pay in Canada to compensate for high cost of living, remoteness, and challenging work environments. Includes significant Northern Living Allowances. |
| Alberta | $39.00 - $52.00 | Historically one of the highest-paying provinces, with strong union (UNA) contracts. |
| British Columbia | $38.50 - $50.00 | Competitive salaries, especially for experienced nurses, but a very high cost of living in major cities like Vancouver. |
| Ontario | $35.00 - $50.00 | Large and diverse job market. The ONA contract is a benchmark for many. Recent legislation changes are impacting wage growth. |
| Saskatchewan | $38.00 - $49.00 | Strong wages relative to the cost of living. |
| Newfoundland & Labrador| $36.00 - $47.00 | Solid wages, with recent increases to attract and retain nurses. |
| Atlantic Canada (NS, NB, PEI) | $35.00 - $45.00 | Salaries are generally lower than in Western and Central Canada, but so is the cost of living. |
| Quebec | $26.00 - $46.00 | Wages have historically lagged behind other large provinces, though recent negotiations aim to close the gap. Fluency in French is essential. |
[Sources: Job Bank Canada, various provincial nursing union collective agreements (UNA, BCNU, ONA, SUN), media reports on salary negotiations].
Why the Discrepancy?
- Cost of Living: Higher wages in places like Alberta and BC are partially offset by a higher cost of living. Conversely, lower wages in the Atlantic provinces are paired with more affordable housing and lifestyles.
- Union Strength and Negotiation Cycles: The timing and success of collective bargaining play a huge role. A province with a recent, favourable contract will temporarily pull ahead of others.
- Provincial Budgets and Politics: The financial health of a province and the political priorities of its government directly impact how much funding is allocated to healthcare and, consequently, to nurse salaries.
- Recruitment and Retention Strategies: The territories and some rural regions offer massive premiums, recruitment bonuses, and housing subsidies as incentives to attract nurses to underserved areas.
### `
` Company Type & Work Setting
Where a nurse works has a profound impact on their salary and overall compensation.
- Public Hospitals (Unionized): This is the gold standard for compensation. Nurses working in publicly funded hospitals are represented by powerful unions that negotiate high base wages, structured pay grids, shift premiums, excellent benefits, and defined-benefit pension plans. The vast majority of Canadian nurses work in this sector.
- Private Clinics and Surgery Centers: Salaries in private settings can be more variable. While some specialized private surgical clinics may offer competitive or even higher base salaries to attract top talent, they often lack the robust pension plans, shift premiums, and job security of the public sector. Pay may be based more on negotiation than a fixed grid.
- Long-Term Care (LTC): The LTC sector has a mix of public, non-profit, and for-profit facilities. Pay for nurses in LTC has historically lagged behind hospitals, but significant recent investments and public attention are helping to close this gap.
- Community & Public Health: Nurses working for public health units, community health centres, or in home care roles generally have salaries comparable to their hospital counterparts, as they are often part of the same provincial health authority and union. Their work hours are typically more regular (e.g., Monday-Friday, 9-5), so total earnings may be lower due to the lack of shift premiums and overtime.
- Travel Nursing: Travel nursing agencies offer a unique model. Nurses take on short-term contracts (e.g., 8-12 weeks) in locations with critical shortages. They are paid a very high hourly wage (often $60 - $100+ per hour) and receive housing stipends and travel reimbursements. While the pay is excellent, it lacks the stability, pension, and long-term benefits of a permanent position.
- Federal Government: Nurses employed by the federal government, for example with Indigenous Services Canada to work in remote First Nations communities or with the Canadian Armed Forces, have their own distinct and very competitive pay scales and benefits packages.
### `
` Area of Specialization
Within the RN role, specialization can significantly boost earning potential, primarily by opening doors to higher-paying roles and environments.
- High-Acuity Specialties: Areas like the Intensive Care Unit (ICU), Emergency Room (ER), Cardiac Care Unit (CCU), and Operating Room (OR) are in constant high demand. While the base pay is often the same as a general medicine floor, these roles provide more opportunities for overtime, "on-call" pay (for OR nurses), and career advancement into specialized leadership or education roles.
- Specialized Outpatient Clinics: Roles in highly specialized clinics like oncology/chemotherapy, dialysis, or fertility clinics can sometimes command higher salaries due to the advanced knowledge and skills required.
- Mental Health and Psychiatry: With a growing focus on mental healthcare, psychiatric nurses are in high demand. Specialized roles in this field, particularly in community outreach or crisis intervention, can be well-compensated.
### `
` In-Demand Skills
Beyond formal qualifications, possessing specific skills can make a nurse more valuable and lead to higher pay or better job opportunities.
- Bilingualism: In many parts of Canada (particularly Ontario, Quebec, and New Brunswick), fluency in both English and French is a major asset and can be a requirement for many positions, often coming with a bilingualism bonus.
- Technical Skills: Proficiency with specific electronic health record systems (e.g., Epic, Cerner), advanced life support certifications (ACLS, PALS), and skills in areas like ventilation management or ECMO are highly sought after.
- Leadership and Management: Skills in delegation, conflict resolution, and team leadership can pave the way to Charge Nurse, Team Lead, and eventually management positions, all of which come with significant pay increases.
Job Outlook and Career Growth for Nurses in Canada
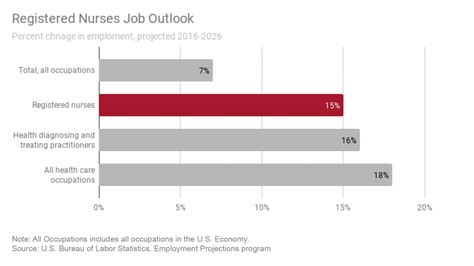
For anyone considering investing years in education and training, the long-term career outlook is a critical consideration. For nursing in Canada, the forecast is exceptionally strong. The profession is characterized by high demand, excellent job security, and a wealth of opportunities for advancement and specialization.
### A Profession in High Demand
The Government of Canada's Job Bank has assigned its highest possible rating of "Very Good" to the job outlook for Registered Nurses across nearly every single province and territory for the 2023-2025 period. This indicates that the number of job seekers is expected to be significantly lower than the number of job openings, creating a highly favourable market for qualified nurses.
Several powerful, long-term trends are driving this demand:
- Aging Population: Canada has a large and aging baby boomer generation. As this cohort ages, the demand for healthcare services—from chronic disease management and acute hospital care to long-term and palliative care—is increasing exponentially. Nurses are at the forefront of providing this care.
- Retiring Nursing Workforce: A significant percentage of the current nursing workforce is also approaching retirement age. The Canadian Nurses Association (CNA) has been sounding the alarm for years about this impending wave of retirements, which will create a massive number of vacancies that need to be filled by new graduates and internationally educated nurses.
- Increased Complexity of Care: Medical advancements mean that patients are living longer with more complex, chronic health conditions. This requires more intensive and specialized nursing care, further driving demand for skilled RNs and NPs.
- Focus on Primary and Community Care: Healthcare systems are shifting towards providing more care outside of traditional hospital settings. This is creating new roles for nurses in community health centres, home care,
