Are you driven by a desire to make a tangible, life-altering impact on people's lives? Do you envision a career where you blend medical science with compassionate coaching, helping individuals reclaim their health and vitality after a major cardiac event? If so, a career in cardiac rehabilitation might be your calling. This field is not just about helping hearts heal physically; it's about restoring confidence, hope, and quality of life.
A career in cardiac rehabilitation is one of the most rewarding paths in healthcare, offering a unique blend of patient interaction, clinical expertise, and measurable results. But beyond the profound personal satisfaction, it's also a stable and financially viable profession. While the national average cardiac rehab salary can be complex, professionals in this field typically earn between $65,000 and $95,000 per year, with significant potential for growth based on your specific role, location, and experience.
I once spoke with a gentleman whose life was turned upside down by a sudden heart attack at 52. He told me it wasn't the surgeons who saved his life that he remembered most vividly, but the cardiac rehab team who, over twelve weeks, taught him how to trust his body again and gave him the tools to live a fuller, healthier life than before. That story perfectly encapsulates the power and importance of this incredible profession.
This guide will serve as your definitive resource for understanding every facet of a career in cardiac rehabilitation. We will dissect salary expectations, explore the factors that drive higher earnings, and lay out a clear, step-by-step roadmap for you to begin your journey.
### Table of Contents
- [What Does a Cardiac Rehabilitation Specialist Do?](#what-is-cardiac-rehab)
- [Average Cardiac Rehab Salary: A Deep Dive](#average-salary)
- [Key Factors That Influence Your Salary](#key-factors)
- [Job Outlook and Career Growth](#job-outlook)
- [How to Get Started in a Cardiac Rehab Career](#how-to-start)
- [Conclusion: Is a Career in Cardiac Rehab Right for You?](#conclusion)
What Does a Cardiac Rehabilitation Specialist Do?

A career in "cardiac rehab" isn't a single job title but rather a specialized practice area for a team of dedicated healthcare professionals. Cardiac rehabilitation is a medically supervised, multidisciplinary program designed to help patients recover from heart attacks, heart surgery, heart failure, and other cardiac conditions. The goal is to stabilize, slow, or even reverse the progression of cardiovascular disease.
A specialist in this field is an integral part of a collaborative team that typically includes:
- Registered Nurses (RNs)
- Exercise Physiologists (EPs)
- Physical Therapists (PTs)
- Respiratory Therapists (RTs)
- Registered Dietitians
- Mental Health Professionals
The core responsibilities of the cardiac rehab team are centered around three main pillars:
1. Monitored Exercise and Physical Activity: This is the cornerstone of cardiac rehab. Specialists design and supervise individualized exercise plans, continuously monitoring patients' heart rate, blood pressure, and EKG (electrocardiogram) rhythms during activity. They teach patients how to exercise safely and effectively to strengthen their heart muscle and improve overall fitness.
2. Patient Education and Lifestyle Modification: Specialists provide crucial education on risk factors for heart disease. This includes counseling on nutrition (heart-healthy diets, label reading), stress management techniques (mindfulness, relaxation), smoking cessation, and the importance of medication adherence.
3. Psychosocial Support: Recovering from a cardiac event can be emotionally and psychologically taxing, often leading to anxiety or depression. The rehab team provides a supportive, encouraging environment, helping patients build confidence and address the mental barriers to recovery.
### A Day in the Life of a Cardiac Rehab Specialist
To make this tangible, let's imagine a day in the life of "Maria," a Clinical Exercise Physiologist in a hospital's outpatient cardiac rehab center.
- 8:00 AM: Maria arrives, reviews the schedule of patients for the day, and checks for any updates or red flags in their electronic health records. She huddles with the on-staff RN to discuss any patients with recent medication changes or reported symptoms.
- 8:30 AM: The first group of patients arrives. Maria greets them, helps them get set up with their heart monitors, and takes their pre-exercise vital signs.
- 9:00 AM - 12:00 PM: Maria leads three back-to-back, one-hour group exercise sessions. She moves continuously around the gym, adjusting treadmill speeds, demonstrating proper form on resistance machines, and offering words of encouragement. She keeps a vigilant eye on the central EKG monitoring station, communicating any abnormalities to the RN. Between patients, she's charting their progress, noting their exercise tolerance, and documenting their vitals.
- 12:00 PM: Lunch break.
- 1:00 PM: Maria meets with a new patient for their initial assessment. She conducts a thorough review of their medical history, performs a six-minute walk test to establish a baseline fitness level, and collaborates with the patient to set realistic, personal goals for their 12-week program.
- 2:00 PM: Maria leads a 45-minute educational session for a group of patients and their families on "Understanding Food Labels for a Heart-Healthy Diet." She answers questions and provides practical tips for grocery shopping.
- 3:00 PM: The final exercise session of the day begins. This group includes a patient who is "graduating" from the program. Maria celebrates their progress, provides them with a detailed home exercise plan, and reinforces the strategies they've learned.
- 4:00 PM - 4:30 PM: Maria finishes her patient charting, responds to emails, and prepares the patient files for the next day's sessions, ensuring a seamless handover for the morning team.
This "day in the life" illustrates the dynamic, patient-focused, and highly interactive nature of the role. It requires a unique combination of clinical knowledge, coaching skills, and genuine empathy.
Average Cardiac Rehab Salary: A Deep Dive
Understanding the salary potential in cardiac rehabilitation requires a nuanced approach. Because the field is comprised of various licensed professionals, the "average cardiac rehab salary" is not a single number but a spectrum. Your specific professional background—whether you are an RN, a PT, an Exercise Physiologist, or another specialist—is the primary determinant of your earning potential.
Let's break down the salary landscape based on the most common roles within a cardiac rehab team, using data from the U.S. Bureau of Labor Statistics (BLS) and leading salary aggregators.
### Cardiac Rehab Salary by Core Profession
The most direct way to estimate your potential salary is to look at the national median pay for your underlying profession. Professionals working in a specialized area like cardiac rehab often earn at or slightly above the median for their field due to the advanced skills required.
Estimated Salary Ranges for Common Cardiac Rehab Roles (2023-2024 Data)
| Professional Role | Median Annual Salary (BLS, May 2023) | Typical Salary Range (Payscale, Salary.com) | Core Educational Requirement |
| :--- | :--- | :--- | :--- |
| Exercise Physiologist | $54,950 | $45,000 - $78,000 | Bachelor's or Master's Degree |
| Registered Nurse (RN) | $86,070 | $72,000 - $105,000 | Associate's or Bachelor's Degree |
| Respiratory Therapist | $77,930 | $65,000 - $89,000 | Associate's Degree |
| Registered Dietitian/Nutritionist| $70,460 | $61,000 - $84,000 | Bachelor's or Master's Degree |
| Physical Therapist (PT) | $99,710 | $85,000 - $115,000+ | Doctorate (DPT) |
| Occupational Therapist (OT) | $96,370 | $82,000 - $110,000+ | Master's or Doctorate |
*Sources: [U.S. Bureau of Labor Statistics Occupational Outlook Handbook](https://www.bls.gov/ooh/), [Payscale.com](https://www.payscale.com/), and [Salary.com](https://www.salary.com/), accessed 2024.*
As the table shows, a Physical Therapist with a doctorate degree working in cardiac rehab will command a significantly higher salary than an Exercise Physiologist with a bachelor's degree. This distinction is the most critical factor in understanding compensation in this field.
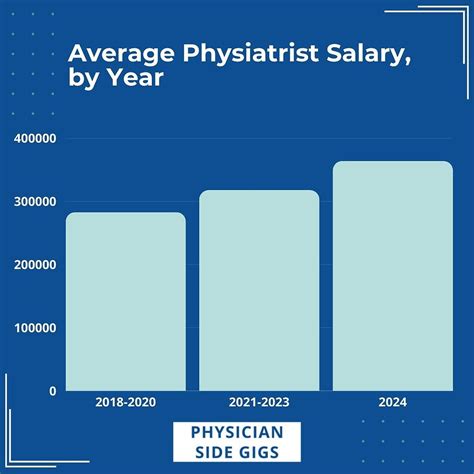
### Salary Progression by Experience Level
Regardless of your specific role, your salary will grow with experience. As you gain expertise, develop specialized skills, and take on more responsibility, your value to your employer increases.
Here is a general breakdown of how salary can progress for a mid-range role like a Cardiac Rehab RN or Exercise Physiologist:
- Entry-Level (0-2 Years):
- Typical Salary: $55,000 - $70,000
- Focus: Learning the core protocols, mastering patient monitoring (EKG interpretation, vital signs), and developing patient education skills under the supervision of senior staff.
- Mid-Career (3-9 Years):
- Typical Salary: $70,000 - $90,000
- Focus: Working with greater autonomy, handling more complex patient cases (e.g., patients with LVADs or recent transplants), contributing to program development, and potentially mentoring new staff. Obtaining a professional certification like the AACVPR's Certified Cardiac Rehab Professional (CCRP) is common at this stage and can boost earnings.
- Senior/Lead (10+ Years):
- Typical Salary: $85,000 - $110,000+
- Focus: This level often transitions into leadership. Responsibilities may include Program Coordinator or Manager, overseeing daily operations, ensuring regulatory compliance (e.g., with AACVPR program certification), managing budgets, and leading quality improvement initiatives. Salaries at this level can vary significantly based on the size and scope of the program.
### Total Compensation: Beyond the Base Salary
When evaluating a job offer, it's crucial to look beyond the annual salary and consider the total compensation package. Healthcare roles, especially those within established hospital systems, often come with robust benefits that add significant value.
- Bonuses: While less common than in corporate settings, some hospital systems offer performance-based bonuses or annual incentives tied to patient outcomes or departmental goals.
- Sign-On Bonuses: In competitive markets or for hard-to-fill roles, employers may offer a sign-on bonus to attract top talent.
- Health Insurance: Comprehensive medical, dental, and vision insurance is standard. The value of an employer-sponsored plan with low premiums and deductibles can be worth thousands of dollars annually.
- Retirement Savings: Most healthcare employers offer a 401(k) or 403(b) retirement plan, often with a generous employer match (e.g., matching 50% of your contributions up to 6% of your salary).
- Paid Time Off (PTO): Generous PTO, including vacation, sick leave, and holidays, is a key benefit that contributes to a healthy work-life balance.
- Continuing Education Stipend: Many employers encourage professional development and will provide an annual allowance to cover the costs of conferences, workshops, and certification renewals.
- Tuition Reimbursement: Some larger hospital systems offer tuition assistance for employees pursuing advanced degrees, which can be a massive financial benefit.
A base salary of $80,000 combined with a strong benefits package can easily equate to a total compensation value well over $100,000.
Key Factors That Influence Your Salary
Your final salary offer is not a fixed number; it's a dynamic figure influenced by a combination of your personal qualifications and external market forces. Understanding these factors will empower you to negotiate effectively and maximize your earning potential throughout your career. This is the most critical section for anyone looking to build a high-earning and sustainable career in cardiac rehab.
### 1. Level of Education and Professional Credentials
This is, without a doubt, the most significant factor. The baseline salary for any role in cardiac rehab is set by the educational requirements of the underlying profession.
- Associate's Degree: This is the minimum requirement for Registered Nurses (ADN) and Respiratory Therapists (AS). While it's a fast track into the healthcare field, professionals with a Bachelor's degree often have a higher starting salary and more opportunities for advancement.
- Bachelor's Degree: A Bachelor of Science in Nursing (BSN) is becoming the industry standard for RNs and is often preferred by top-tier hospitals, leading to higher pay. A Bachelor's in Kinesiology or Exercise Science is the standard entry point for an Exercise Physiologist. For Registered Dietitians, a bachelor's degree is the minimum, but a master's is increasingly required.
- Master's Degree: This level of education significantly boosts earning potential. For Exercise Physiologists, a Master's degree is highly desirable and often required for leadership roles or positions in more clinically intensive settings. It demonstrates a higher level of expertise in exercise prescription for clinical populations. For Occupational Therapists and, increasingly, Registered Dietitians, a master's is the standard entry-level degree.
- Doctorate Degree: This represents the pinnacle of education in therapy roles. All new Physical Therapists are now required to hold a Doctor of Physical Therapy (DPT) degree. Similarly, many Occupational Therapists hold a Doctorate of Occupational Therapy (OTD). This advanced clinical training and expertise place them at the top of the earnings spectrum within the cardiac rehab team.
Specialized Certifications: Beyond your primary degree and license, professional certifications act as powerful salary boosters. The premier certification in this field is the Certified Cardiac Rehab Professional (CCRP) offered by the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR). Earning your CCRP validates your specialized knowledge and experience, making you a more valuable candidate and often qualifying you for a higher pay grade or a promotion. Other valuable certifications include those from the American College of Sports Medicine (ACSM), such as the Certified Clinical Exercise Physiologist (CEP).
### 2. Years of Experience and Career Trajectory
As detailed in the previous section, experience is a powerful driver of salary growth. Here's a more granular look at the value of experience:
- Novice (0-2 years): You are building foundational skills. Your value is in your potential and willingness to learn. Salary is typically at the lower end of the scale for your profession.
- Competent Professional (3-5 years): You are proficient in your role. You can manage a full patient load independently and are beginning to handle more complex cases. This is where you see the first significant salary jump. You are a reliable and productive member of the team.
- Proficient Specialist (6-10 years): You have deep expertise. You are the go-to person for tough cases, you likely have your CCRP certification, and you may be involved in mentoring junior staff or leading small projects. Your salary should be well above the median for your profession.
- Expert / Leader (10+ years): At this stage, your value extends beyond direct patient care. You are a leader, a mentor, and a strategist. You may be in a formal leadership role like a Program Manager, where your responsibilities include budget management, staff supervision, and program certification. Your salary will be at the highest end of the spectrum and may include leadership bonuses.
### 3. Geographic Location
Where you work matters—a lot. Cost of living and demand for healthcare professionals create significant salary disparities across the country. A Cardiac Rehab RN in a high-cost urban center can easily earn 30-50% more than a colleague with the same experience in a low-cost rural area.
High-Paying States and Metropolitan Areas:
These locations typically combine high demand with a high cost of living, driving salaries upward.
- California: Cities like San Francisco, San Jose, Los Angeles, and Sacramento consistently rank as the highest-paying for healthcare professionals. An experienced RN or PT in these areas can earn well over $120,000.
- New York: The New York City metropolitan area offers highly competitive salaries to offset the extreme cost of living.
- Massachusetts: Boston's world-class hospital systems create a competitive market for talent.
- Oregon and Washington: These states, particularly in the Portland and Seattle metro areas, offer strong salaries for healthcare workers.
- Alaska and Hawaii: Due to their remote nature and high cost of living, these states offer some of the highest wages in the country to attract professionals.
Lower-Paying States:
These states generally have a lower cost of living, which is reflected in their salary ranges.
- Mississippi
- Alabama
- Arkansas
- South Dakota
- West Virginia
*Data Reference:* The BLS provides detailed [state](https://www.bls.gov/oes/current/oessrcst.htm) and [metropolitan area](https://www.bls.gov/oes/current/oessrcma.htm) employment and wage data for all major occupations, allowing you to research specific locations.
### 4. Work Setting and Employer Type
The type of facility you work in directly impacts your compensation and work environment.
- Large, Urban Hospital Systems: These are often the top-paying employers. They have larger budgets, are frequently unionized (which can lead to higher, standardized wages and better benefits), and handle the most complex patient cases. Working at a prestigious academic medical center can also add a significant boost to your resume.
- Outpatient Clinics (Hospital-Affiliated or Private): These are the most common settings for cardiac rehab. Salaries are competitive, often just below those of large inpatient hospitals. The work-life balance can be more predictable, with no night or weekend shifts typically required.
- Physician's Offices or Cardiology Groups: Some larger cardiology practices run their own small-scale cardiac rehab programs. Salaries can be variable but are generally competitive with outpatient clinics.
- Long-Term Care or Skilled Nursing Facilities: These facilities may offer sub-acute rehab services. Pay can be competitive but the work environment and patient population are different from traditional outpatient rehab.
- Government/VA Hospitals: The Department of Veterans Affairs (VA) is a major employer of cardiac rehab specialists. Salaries are based on a transparent, government-set pay scale (the GS scale) and often come with exceptional federal benefits and job security.
### 5. In-Demand Skills and Sub-Specializations
To move from an average earner to a top earner, you need to cultivate a specific set of high-value skills.
Clinical/Hard Skills:
- Advanced EKG Interpretation: The ability to confidently identify a wide range of arrhythmias and ischemic changes on a live EKG is paramount. This is a non-negotiable, high-value skill.
- Advanced Exercise Prescription: Going beyond basic templates and being able to design highly individualized exercise plans for patients with multiple comorbidities (e.g., diabetes, COPD, kidney disease) is a key differentiator.
- Knowledge of Advanced Cardiac Therapies: Expertise in working with patients who have Left Ventricular Assist Devices (LVADs), pacemakers/ICDs, or are post-transplant is highly sought after.
- Data Analysis and Reporting: The ability to track patient outcomes, analyze program effectiveness, and report on key metrics for quality improvement and program certification is crucial, especially for leadership roles.
Interpersonal/Soft Skills:
- Motivational Interviewing: This is a counseling technique used to help patients find their own motivation to change behavior. Mastering this skill leads to better patient adherence and outcomes, making you a more effective clinician.
- Patient Education and Health Literacy: The ability to break down complex medical information into simple, actionable advice for patients from all backgrounds is a core competency.
- Empathy and Rapport Building: Patients are often scared and vulnerable. The ability to connect with them on a human level builds the trust necessary for a successful recovery.
- Team Collaboration: Cardiac rehab is a team sport. Being an excellent communicator and collaborator who works seamlessly with nurses, dietitians, and physicians is essential.
By strategically developing these factors—pursuing advanced education, gaining diverse experience, and honing in-demand skills—you can actively steer your career towards higher compensation and greater professional fulfillment.
Job Outlook and Career Growth

For those considering a career in cardiac rehabilitation, the future is exceptionally bright. The demand for qualified specialists is strong and projected to grow significantly over the next decade. This robust outlook is driven by powerful, long-term demographic and healthcare trends.
### Strong Growth Projections Across the Board
The U.S. Bureau of Labor Statistics (BLS) projects strong growth for all the core professions that make up a cardiac rehab team. The overall demand for healthcare occupations is projected to grow 13 percent from 2022 to 2032, much faster than the average for all occupations, adding about 1.8 million new jobs.
Here are the specific 10-year growth projections for key cardiac rehab roles (2022-2032):
- Physical Therapists: 15% growth (Much faster than average)
- Occupational Therapists: 12% growth (Much faster than average)
- Exercise Physiologists: 9% growth (Faster than average)
- Registered Nurses: 6% growth (Faster than average)
- Respiratory Therapists: 13% growth (Much faster than average)
- Dietitians and Nutritionists: 7% growth (Faster than average)
*Source: [U.S. Bureau of Labor Statistics, Occupational Outlook Handbook](https://www.bls.gov/ooh/), accessed 2024.*
### Key Drivers of Job Growth
Several key factors are fueling this sustained demand:
1. The Aging Population: The large Baby Boomer generation is aging, leading to a higher incidence of chronic conditions, including heart disease. As this demographic requires more cardiovascular care, the need for rehabilitative services will surge.
2. Increased Survival Rates: Advances in medical and surgical treatments mean that more people are surviving heart attacks and other major cardiac events. These survivors are prime candidates for cardiac rehab to improve their long-term health and prevent future events.
3. A Shift Towards Preventative Care: There is a growing emphasis in healthcare on prevention and wellness. Cardiac rehab is recognized as a highly effective, evidence-based intervention that reduces hospital readmissions, lowers healthcare costs, and improves quality of life. Insurers and hospital systems are increasingly promoting and investing in these programs.
4. Expanded Indications for Rehab: The list of conditions for which cardiac rehab is recommended and covered by insurance continues to grow, now including stable angina, heart failure, and certain congenital heart diseases, further expanding the pool of eligible patients.
### Emerging Trends and Future Opportunities
The field of cardiac rehabilitation is not static. Staying ahead of emerging trends will be key to career advancement and long-term success.
- Telehealth and Hybrid Rehab: The COVID-19 pandemic accelerated the adoption of virtual care. Hybrid models, combining in-person sessions with remote monitoring and virtual coaching, are becoming more common. Professionals who are comfortable with technology and telehealth platforms will be in high demand.
- Integration of Wearable Technology: Devices like smartwatches and fitness trackers are becoming powerful tools for remote patient monitoring. Specialists who can effectively integrate data from these wearables into patient care plans will be at the forefront of the field.
- Focus on Comorbidities: Patients rarely have just one health issue. The future of cardiac rehab involves a more holistic approach to managing related conditions like diabetes, obesity, and depression simultaneously.
- Value-Based Care: Healthcare is moving away from a fee-for-service model to a value-based model, where providers are compensated based on patient outcomes. Cardiac rehab programs that can demonstrate their value through data—showing reduced readmissions, improved biometrics, and higher patient satisfaction—will thrive.
### Advancing Your Career in Cardiac Rehab
Your career doesn't have to stop at being a staff clinician. With experience and strategic planning, you can move into various leadership and specialized roles:
- Team Lead or Senior Specialist: The first step up, involving mentoring new staff and handling the most complex patient cases.
- Program Coordinator/Manager: Overseeing the day-to-day operations of a cardiac rehab program, including staffing, scheduling, budgeting, and ensuring compliance with AACV
