Introduction

Embarking on a career as a cardiologist represents the pinnacle of medical ambition for many. It is a path defined by rigorous intellectual challenge, profound human impact, and the opportunity to work on the very frontier of life-saving science. For those who set their sights on practicing in the vibrant, high-stakes environment of New York City, these ambitions are magnified. NYC is not just a city; it's a global epicenter for medicine, research, and innovation, offering a unique landscape for a cardiologist's career to flourish. But with this high-stakes environment comes a critical question for any aspiring or practicing physician: What is the financial reality? What can one truly expect for a cardiologist salary in NYC?
The answer is as complex and multifaceted as the city itself. While the earning potential is substantial, with average salaries comfortably soaring into the high six-figures, the final number on your paycheck is influenced by a dizzying array of factors. This guide is designed to be your definitive resource, moving beyond simple averages to provide a granular, authoritative analysis of cardiologist compensation in New York City. We will dissect every component, from the type of practice you choose to the subspecialty you master, giving you the data-driven insights needed to navigate your career with confidence.
I remember speaking with a family friend, a seasoned interventional cardiologist at a major Manhattan hospital. He described a particularly grueling 24-hour on-call shift that culminated in a life-saving emergency angioplasty at 3 AM. He said, "The exhaustion vanishes the moment you see that artery open up on the screen. You've just given someone back their future. The compensation allows you to live in this demanding city, but that moment... that's the *real* currency." His words perfectly capture the duality of this profession—it is both a calling and a highly-skilled, well-compensated career. This article will honor both aspects, providing a clear-eyed view of the financial rewards that accompany one of medicine's most demanding and respected roles.
### Table of Contents
- [What Does a Cardiologist in NYC Do?](#what-does-a-cardiologist-do)
- [Average Cardiologist Salary in NYC: A Deep Dive](#average-salary-deep-dive)
- [Key Factors That Influence a Cardiologist's Salary](#key-factors)
- [Job Outlook and Career Growth for Cardiologists in NYC](#job-outlook)
- [How to Become a Cardiologist: The Step-by-Step Path](#how-to-get-started)
- [Conclusion: Is a Cardiology Career in NYC Right for You?](#conclusion)
What Does a Cardiologist in NYC Do?
A cardiologist is a specialized physician expert in diagnosing, treating, and preventing diseases of the heart and blood vessels—the cardiovascular system. In a fast-paced, high-stress metropolis like New York City, their role is particularly vital, addressing everything from congenital heart defects in newborns to heart attacks in high-powered executives and chronic heart failure in the elderly population. The work is a demanding blend of deep scientific knowledge, intricate technical skill, and profound patient empathy.
Their core responsibilities can be categorized into three main areas:
1. Diagnosis: Cardiologists are medical detectives of the heart. They use a sophisticated arsenal of tools and techniques to identify the root cause of a patient's symptoms. This involves conducting thorough physical exams, taking detailed patient histories, and ordering and interpreting a wide range of diagnostic tests, such as:
- Electrocardiograms (ECGs or EKGs): To record the heart's electrical activity.
- Echocardiograms: Using ultrasound to create images of the heart's chambers, valves, and blood flow.
- Stress Tests: Monitoring heart function while a patient exercises on a treadmill or is given medication to simulate exercise.
- Cardiac Catheterization: An invasive procedure to visualize coronary arteries and measure pressure within the heart.
- Holter and Event Monitors: Portable devices that record heart rhythms over extended periods.
2. Treatment: Once a diagnosis is made, the cardiologist develops a comprehensive treatment plan. This can range from conservative management to life-saving interventions. Treatment modalities include:
- Medication Management: Prescribing and managing drugs to control blood pressure, lower cholesterol, manage arrhythmias, or prevent blood clots.
- Lifestyle Counseling: Providing crucial guidance on diet, exercise, smoking cessation, and stress management to prevent disease progression.
- Interventional Procedures: Performing minimally invasive procedures like angioplasty (opening blocked arteries) and stent placement.
- Electrophysiology Procedures: Implanting pacemakers and defibrillators (ICDs) or performing ablations to correct abnormal heart rhythms.
3. Prevention and Ongoing Management: A significant part of a cardiologist's work is focused on prevention. This involves identifying at-risk patients and implementing strategies to mitigate their risk factors. For patients with chronic conditions like coronary artery disease or heart failure, the cardiologist provides long-term care, monitoring their condition and adjusting treatment plans as needed to optimize their quality of life.
---
### A Day in the Life of an NYC Cardiologist
To make this role more tangible, consider a "hybrid" day for a cardiologist who splits their time between a private practice office in Midtown Manhattan and a major affiliated hospital.
- 7:00 AM - 8:30 AM (Hospital Rounds): The day begins at the hospital. Review charts of admitted patients, check overnight events, and speak with the on-call residents. Visit each patient at their bedside, discussing progress, answering family questions, and adjusting care plans. Order follow-up tests and coordinate with other specialists.
- 8:30 AM - 9:00 AM (Commute & Prep): Grab a quick coffee and take the subway or a cab to the private office. Briefly huddle with the office manager and nurses to review the day's patient schedule and any urgent messages.
- 9:00 AM - 1:00 PM (Morning Clinic): See a series of scheduled patients. This could include a new patient with chest pain, a follow-up for a patient post-stent placement, an elderly patient with congestive heart failure, and an annual check-up for a patient with high cholesterol. Each 20-30 minute slot is a whirlwind of examination, EKG interpretation, and focused conversation.
- 1:00 PM - 2:00 PM (Lunch & Administrative Tasks): A quick lunch, often at the desk while catching up on administrative work. This is the time for returning urgent phone calls to patients, reviewing test results that came in (echocardiograms, stress tests), signing prescription refills, and dictating patient notes into the Electronic Health Record (EHR) system.
- 2:00 PM - 5:00 PM (Afternoon Clinic & Procedures): The afternoon might involve more patient consultations or could be a dedicated block for in-office procedures. This might include reading and interpreting a batch of echocardiograms performed by a sonographer or overseeing nuclear stress tests.
- 5:00 PM - 6:30 PM (Wrapping Up): The last patient leaves, but the day isn't over. The cardiologist spends another hour finalizing all patient charts from the day, following up on critical lab values, and creating a "to-do" list for the next morning.
- After 6:30 PM (On-Call Responsibility): Even after leaving the office, the cardiologist may be on call for the practice or the hospital. This means being available by phone to handle patient emergencies or to be called back to the hospital for an urgent procedure, like a heart attack, at any hour of the night.
---
This schedule highlights the intense intellectual, emotional, and time commitment required. The high salary of an NYC cardiologist is a direct reflection of this level of responsibility, the extensive training required, and the life-or-death decisions made daily.
Average Cardiologist Salary in NYC: A Deep Dive
When analyzing compensation for a role as specialized as a cardiologist, looking at a single number can be misleading. The financial landscape is a spectrum, influenced by a multitude of factors we will explore later. However, establishing a baseline is crucial. By synthesizing data from leading salary aggregators and industry reports, we can paint a clear picture of the earning potential in New York City.
It's important to note that NYC salaries for physicians are consistently among the highest in the nation, but this is also balanced by a significantly higher cost of living.
### National vs. NYC Cardiologist Salaries
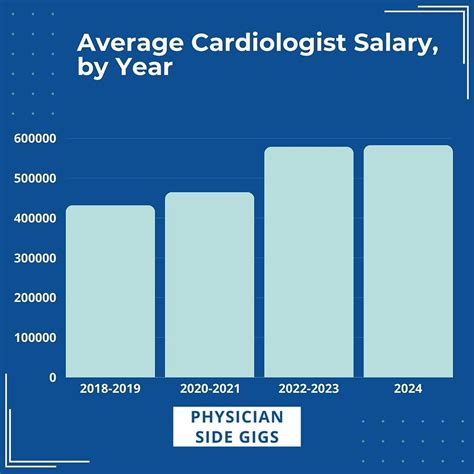
First, let's establish a national benchmark. According to the 2023 Medscape Physician Compensation Report, one of the most comprehensive surveys in the industry, the average salary for a cardiologist in the United States is $507,000 per year. This figure places cardiology among the top-earning medical specialties.
Now, let's zoom in on New York City. Data from various sources consistently shows a premium for practicing in the NYC metropolitan area.
- Salary.com, which provides granular, real-time compensation data, reports that the average base salary for a cardiologist in New York, NY, is $476,011 as of late 2023. However, the typical salary range is much wider, generally falling between $385,811 and $599,013.
- Glassdoor reports a slightly higher average, with the "likely range" for a cardiologist in the NYC area being between $318,000 and $553,000, with an average base pay around $416,500.
- ZipRecruiter data shows an average annual salary for a cardiologist in New York City of $394,402, with top earners reaching as high as $614,500.
Why the variation? These platforms use different data sets and methodologies. Salary.com often reflects HR-reported data from employers, while Glassdoor relies on self-reported data from employees. Medscape's report is based on a large-scale physician survey. The key takeaway is that an average baseline in NYC sits comfortably in the $400,000 to $500,000 range, with significant upward potential.
### Cardiologist Salary by Experience Level in NYC
Experience is one of the most powerful drivers of salary growth. A cardiologist's earning potential increases significantly after completing their fellowship and gaining real-world experience.
Here is a representative breakdown of how salary might progress in the New York City market, synthesized from sources like Salary.com and Payscale:
| Career Stage | Years of Experience | Typical Base Salary Range (NYC) | Notes |
| :--- | :--- | :--- | :--- |
| Early Career | 0-3 Years | $320,000 - $400,000 | Position just out of fellowship. Often includes a starting bonus and a structured ramp-up period. Lower initial productivity expectations. |
| Mid-Career | 4-9 Years | $400,000 - $525,000 | Has established a patient base and is working at full productivity. Compensation often has a larger variable component tied to wRVUs. |
| Experienced | 10-19 Years | $480,000 - $650,000+ | At the peak of their clinical career. May have taken on leadership roles (e.g., Director of a cath lab). Highly efficient and in-demand. |
| Late Career / Senior | 20+ Years | $500,000 - $700,000+ | Often holds senior partnership in a private practice or a significant administrative/leadership role in a hospital system. May work fewer clinical hours but has high value. |
*Source: Synthesized data from Salary.com, Medscape Compensation Report, and industry analysis for the NYC market.*
### Deconstructing the Compensation Package: More Than Just a Salary
A cardiologist's total compensation is rarely just a flat salary. The package is a complex structure designed to incentivize productivity and reward expertise. Understanding these components is essential.
- Base Salary: The guaranteed annual income, which forms the foundation of the compensation plan. In hospital-employed models, this is often a fixed amount for the first 1-2 years before transitioning to a productivity-based model.
- Productivity Bonus (wRVU-Based): This is the most significant variable component for most cardiologists. Compensation is tied to Work Relative Value Units (wRVUs). Each patient encounter, procedure, and test is assigned a wRVU value by the Centers for Medicare & Medicaid Services (CMS). Physicians are often paid a certain dollar amount per wRVU generated above a set threshold. An interventional cardiologist performing multiple complex procedures will generate far more wRVUs than a non-invasive cardiologist focused on office consultations. This system directly rewards proceduralists.
- Performance & Quality Bonuses: An increasing number of health systems are incorporating bonuses tied to quality metrics. These can include patient satisfaction scores (HCAHPS), adherence to clinical guidelines (e.g., prescribing statins for post-MI patients), and hospital-wide performance goals.
- Signing Bonus: A one-time, upfront payment to attract a new cardiologist, especially in a competitive market like NYC. These can range from $20,000 to $50,000 or more.
- Relocation Assistance: A stipend to cover the costs of moving to New York City.
- Retirement Benefits: Typically a 401(k) or 403(b) plan with an employer match. In private practice, this can include more lucrative profit-sharing or defined-benefit plans.
- Continuing Medical Education (CME) Allowance: An annual stipend (e.g., $5,000 - $15,000) to cover the cost of attending conferences, subscribing to journals, and maintaining board certification, which is crucial for staying current in the field.
- Malpractice Insurance: Employer-paid malpractice coverage is a standard and highly valuable benefit. It's critical to understand the type of policy offered ("claims-made" vs. "occurrence") and who pays for "tail coverage" if you leave the practice.
- Health Insurance and Other Benefits: Comprehensive health, dental, and vision insurance, as well as life and disability insurance.
- Partnership Track (Private Practice): For those joining a private group, the offer may include a track to become a partner after a few years. This involves "buying in" to the practice but provides a share of the group's overall profits, significantly boosting long-term earning potential.
When evaluating a job offer in NYC, it is vital to look at the Total Compensation—the sum of the base salary plus the value of all bonuses and benefits—to get a true sense of the offer's strength.
Key Factors That Influence a Cardiologist's Salary

The difference between a cardiologist earning $350,000 and one earning over $750,000 in New York City lies in a combination of deliberate career choices and market dynamics. This section breaks down the most critical factors that shape your earning potential.
###
1. Subspecialization: The Great Differentiator
Within cardiology, not all paths lead to the same paycheck. The choice of subspecialty fellowship after the general cardiology fellowship is perhaps the single most important decision influencing income. Procedural-based subspecialties, which generate high wRVUs, command significantly higher salaries.
- Interventional Cardiology: (Highest Earning Potential) These are the proceduralists who perform angioplasty, stenting, and increasingly, structural heart procedures like TAVR (transcatheter aortic valve replacement) and MitraClip. Due to the high wRVU values of these life-saving interventions, they are consistently the top earners. An experienced interventionalist in a productive NYC practice can easily earn $600,000 to $900,000+, with top performers in private practice exceeding $1 million.
- Electrophysiology (EP): (Very High Earning Potential) EP specialists diagnose and treat heart rhythm disorders. They perform complex ablations and implant devices like pacemakers and implantable cardioverter-defibrillators (ICDs). These are also high-wRVU procedures, placing EP salaries just below or on par with interventional cardiology, typically in the $550,000 to $800,000+ range.
- Non-Invasive Cardiology: (Strong Earning Potential) These cardiologists focus on diagnosis and management through consultation and testing (echocardiography, nuclear cardiology, stress tests). While they do not perform catheter-based interventions, they are the backbone of most cardiology practices. Their compensation is robust but generally lower than their interventional colleagues. In NYC, a non-invasive cardiologist can expect to earn in the $380,000 to $550,000 range, with income heavily influenced by the volume of patients seen and tests read.
- Advanced Heart Failure & Transplant Cardiology: This is a highly specialized, cognitively demanding field focused on managing patients with end-stage heart failure, ventricular assist devices (VADs), and heart transplants. While it involves some procedures, it is less procedure-heavy than interventional or EP. Salaries are very respectable, often in the $400,000 to $600,000 range, particularly in large academic centers with transplant programs like those in NYC.
- Other Subspecialties: Fields like preventive cardiology, cardio-oncology, and adult congenital heart disease are growing. They are typically more cognitive and less procedural, with salaries often aligning more closely with non-invasive cardiology.
###
2. Practice Setting: The Business Model Matters
Where you choose to work has a profound impact on your compensation structure and ceiling.
- Private Practice (Physician-Owned Group): This setting traditionally offers the highest long-term earning potential. Initially, a new cardiologist joins as an employee with a salary and bonus structure. After 2-3 years, they are typically offered a partnership track, which requires a "buy-in." As a partner, they receive a share of the practice's overall profits, including ancillary services like in-office nuclear imaging and echocardiography labs, which can be extremely lucrative. A senior partner in a successful multi-physician private cardiology group in the NYC metro area can be among the highest earners in medicine. However, this model also comes with the greatest risk and administrative burden—partners are business owners responsible for overhead, staffing, billing, and malpractice costs.
- Hospital or Large Health System Employment: This has become the most common model for physicians, including cardiologists. It offers stability, predictable hours (relative to private practice), and relief from administrative headaches. The hospital handles billing, staffing, and overhead. Compensation is typically a base salary plus a productivity (wRVU) bonus. While the ceiling might be lower than a private practice partnership, top-producing cardiologists in major NYC health systems like Northwell Health, Mount Sinai, or NYU Langone can still earn $500,000 to $700,000+, especially in interventional subspecialties.
- Academic Medical Center: Working for an academic institution (e.g., Columbia University Irving Medical Center, Weill Cornell Medicine) often involves a trade-off. Base salaries are typically 10-20% lower than in private or hospital-employed settings. However, the overall mission is different. The role is a tripartite mission of clinical care, research, and teaching medical students and residents. The "compensation" is not just monetary; it includes protected time for research, the prestige of the institution, and opportunities to become a thought leader in the field. Total income can be supplemented by research grants and honoraria for speaking engagements.
- Locum Tenens: This involves working as a temporary, independent contractor to fill in for other physicians. *Locum tenens* cardiologists are paid a high daily or hourly rate and often have travel and housing expenses covered. While it lacks stability, it can be very lucrative for short periods and offers high flexibility.
###
3. Geographic Location (Within the NYC Metro Area)
Even within the New York City metropolitan area, salaries can vary.
- Manhattan: Tends to have the highest concentration of prestigious academic centers and large hospital systems. Competition is fierce, but the salaries for top talent at elite institutions are among the highest. However, the cost of living and practice overhead are also astronomical.
- The Other Boroughs (Brooklyn, Queens, The Bronx, Staten Island): These boroughs have a massive and diverse patient population, creating high demand for cardiologists in both hospital and community-based private practices. Compensation can be very competitive, sometimes exceeding Manhattan salaries as practices compete for talent to serve these large communities.
- Long Island & Westchester County: These affluent suburban areas are home to many successful private practices and burgeoning health system satellite campuses. Cardiologists here often enjoy slightly lower practice overhead and a different patient demographic, with compensation packages that are highly competitive with, and often exceed, those in the five boroughs. According to the Medscape report, the Northeast is the highest-paying region for cardiologists in the U.S.
###
4. Years of Experience and Reputation
As detailed in the salary table, experience is a linear driver of income. In the early years, a cardiologist is building speed, efficiency, and a patient referral base. With 10+ years of experience, a cardiologist has a well-established reputation among referring primary care physicians and other specialists. An experienced interventionalist known for successfully handling complex cases will be in high demand, giving them significant leverage in salary negotiations or driving higher patient volume in private practice.
###
5. Level of Education and Advanced Training
The baseline educational path for a cardiologist is already extensive: 4 years of undergraduate, 4 years of medical school, 3 years of internal medicine residency, and 3 years of general cardiology fellowship. That's a minimum of 14 years post-high school.
Additional training further boosts earning potential:
- Subspecialty Fellowship: As discussed, an extra 1-2+ years for interventional, EP, or heart failure fellowship directly translates to a higher salary tier.
- Advanced Degrees: While not common, a cardiologist with an MBA may be fast-tracked into administrative leadership roles (e.g., Chief of Cardiology, Chief Medical Officer), which come with significant stipends and higher overall compensation. An MPH (Master of Public Health) can be valuable for roles in public health and policy.
- Board Certifications: Initial board certification in Internal Medicine and Cardiovascular Disease is required. Maintaining these certifications (MOC) and gaining additional certifications in subspecialties like echocardiography, nuclear cardiology, or interventional cardiology is essential and signals a high level of expertise that employers value.
###
6. In-Demand Skills and Procedural Expertise
Cardiology is a field in constant evolution. Physicians who master new, high-demand technologies and procedures can command a premium salary.
- Structural Heart Procedures: Expertise in TAVR, MitraClip, WATCHMAN device implantation, and PFO closure is one of the most significant salary drivers in modern cardiology. Cardiologists with this skillset are highly sought after by major medical centers.
- Complex Coronary Intervention: Skills in handling challenging cases like chronic total occlusions (CTOs) set an interventionalist apart.
- Advanced Electrophysiology: Proficiency in complex ablations for atrial fibrillation and ventricular tachycardia, as well as leadless pacemaker implantation.
- Leadership and Administrative Skills: The ability to lead a department, manage a budget, and oversee quality improvement initiatives is highly valuable. A Medical Director of a non-invasive lab or cath lab will receive an additional stipend on top of their clinical compensation.
- Telehealth Proficiency: In the post-pandemic era, being comfortable and efficient with virtual consultations is an increasingly important skill that allows practices to expand their reach and improve efficiency.
Job Outlook and Career Growth for Cardiologists in NYC

The long-term career outlook for cardiologists, particularly in a densely populated and aging region like New York City, is exceptionally strong. The demand for cardiovascular care is projected to grow steadily, driven by powerful demographic and public health trends.
### National Job Growth Projections
The U.S. Bureau of Labor Statistics (BLS) groups cardiologists under the broader category of "Physicians and Surgeons." According to the BLS's Occupational Outlook Handbook, employment for this group is projected to grow 3 percent from 2022 to 2032, which is about as fast as the average for all occupations.
While 3% might seem modest, it's essential to understand the context. This translates to about 24,000 total job openings for physicians and surgeons projected each year, on average, over the decade. Many of those openings are expected to result from the need to replace workers who transfer to different occupations or exit the labor force, such as to retire.
The primary drivers for this sustained demand include:
- An Aging Population: The baby boomer generation is aging, leading to a higher incidence of age-related cardiovascular diseases like coronary artery disease, atrial fibrillation, and heart failure. This demographic shift is a fundamental engine of demand for cardiologists.
- Rising Prevalence of Chronic Diseases: Increased rates of obesity, diabetes, and hypertension—major risk factors for heart disease—continue to fuel the need for cardiovascular specialists for both treatment and prevention.
- Advances in Treatment: New diagnostic tools, medications, and minimally invasive procedures have transformed cardiology