Introduction

Imagine the quiet, focused intensity of an operating room. A human heart, the very engine of life, lies still and exposed, temporarily reliant on the rhythmic pulse of a bypass machine. In this high-stakes environment, a team of experts works in perfect synchrony, and standing shoulder-to-shoulder with the lead surgeon is the Cardiothoracic Physician Assistant (CT PA). This is not merely a job; it is a calling that demands exceptional skill, unwavering composure, and a profound dedication to mending the most vital of organs. For those who can meet this challenge, the rewards—both professional and financial—are among the highest in the medical field.
A career as a CT PA offers a unique blend of intellectual rigor, hands-on surgical work, and the deep satisfaction of giving patients a new lease on life. This demanding specialization also commands a significant salary, with the national average for experienced practitioners often soaring well above $150,000, and top earners in high-demand locations exceeding $200,000 annually. During my time analyzing healthcare career paths, I once interviewed a senior CT PA who had just finished a grueling 12-hour day that included a complex valve replacement. She told me, "The exhaustion is real, but the feeling of seeing that patient sitting up and talking to their family the next morning... that's a payment no bank can issue." It's this profound sense of purpose, coupled with outstanding financial compensation, that makes this one of the most aspirational roles for Physician Assistants today.
This guide will serve as your definitive resource, a comprehensive roadmap to understanding every facet of the cardiothoracic surgery PA salary and the career path that leads to it. We will dissect compensation data, explore the critical factors that influence your earning potential, analyze the robust job outlook, and provide a clear, step-by-step plan to help you launch your own career in this elite field.
### Table of Contents
- [What Does a Cardiothoracic Surgery PA Do?](#what-does-a-cardiothoracic-surgery-pa-do)
- [Average Cardiothoracic Surgery PA Salary: A Deep Dive](#average-cardiothoracic-surgery-pa-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
What Does a Cardiothoracic Surgery PA Do?

To truly understand the value and compensation of a Cardiothoracic Physician Assistant, one must first appreciate the breadth and depth of their responsibilities. A CT PA is far more than a simple assistant; they are a highly skilled clinician and an integral member of the surgical team, exercising a significant degree of autonomy and medical decision-making under the supervision of a cardiothoracic surgeon. Their work spans the entire continuum of patient care: before, during, and after surgery.
The role can be broken down into three primary domains:
1. Pre-Operative Care: Before a patient ever enters the operating room, the CT PA is deeply involved in their preparation. This phase is critical for ensuring a safe and successful surgical outcome.
- Patient Evaluation: Conducting comprehensive patient histories and physical examinations.
- Diagnostic Interpretation: Ordering and interpreting diagnostic tests such as EKGs, chest x-rays, CT scans, and cardiac catheterization reports.
- Patient Education: Explaining the planned surgical procedure, its risks, and its benefits to patients and their families in a clear, compassionate manner. This helps manage expectations and obtain informed consent.
- Surgical Preparation: Ensuring all necessary pre-operative documentation, lab work, and medical clearances are in place.
2. Intra-Operative (Surgical) Responsibilities: This is the heart of the job and where the CT PA's specialized technical skills shine. They typically function as the "first assistant" to the surgeon.
- Endoscopic Vein Harvesting (EVH): This is a cornerstone skill for most CT PAs. Using minimally invasive techniques, the PA expertly harvests the saphenous vein from the patient's leg, which will be used as a graft for coronary artery bypass surgery. Proficient EVH significantly reduces patient morbidity and surgical time.
- Surgical Assisting: This goes far beyond simply holding retractors. The CT PA anticipates the surgeon's needs, provides exposure of the surgical site, assists with suturing and tying knots, and manages hemostasis (controlling bleeding).
- Conduit Harvesting: In addition to veins, PAs may also be responsible for harvesting other conduits like the radial artery or internal mammary artery.
- Opening and Closing: Performing the sternotomy (opening the chest) and, more commonly, closing the chest incision with wires, sutures, and staples at the conclusion of the case.
- Procedural Assistance: Assisting in cannulation for cardiopulmonary bypass and the insertion of chest tubes and drainage systems.
3. Post-Operative Management: The PA's responsibility does not end when the patient leaves the OR. They are crucial to managing the patient's recovery, which is often a complex and delicate process.
- Intensive Care Unit (ICU) Management: PAs often manage patients in the CVICU (Cardiovascular Intensive Care Unit) immediately following surgery. This includes managing ventilators, titrating vasoactive medications (pressors), monitoring hemodynamics, and addressing acute complications like bleeding or arrhythmias.
- Daily Rounds: Conducting daily rounds on post-operative patients on the surgical floor, assessing their progress, managing medications, and adjusting the plan of care.
- Procedure Performance: Removing chest tubes, pacing wires, and surgical drains at the bedside.
- Discharge Planning: Preparing patients for discharge by providing education on medications, activity restrictions, and follow-up care, and writing discharge summaries.
### A Day in the Life of a CT PA
To make this concrete, here is a plausible snapshot of a typical day:
- 5:30 AM: Arrive at the hospital. Begin "pre-rounding" on the CVICU and step-down unit patients. Review overnight events, vital signs, lab results, and imaging for all post-operative patients on the service.
- 6:30 AM: Meet with the surgical team and the attending surgeon to round on every patient. Present findings, discuss care plans, and make adjustments to medications and treatments.
- 7:30 AM: Head to the pre-operative holding area to see the first surgical patient of the day. Perform a final check, answer last-minute questions, and confirm consent.
- 8:00 AM - 1:00 PM: In the Operating Room for a Coronary Artery Bypass Grafting (CABG) x4. Perform the endoscopic vein harvest while the surgeon prepares the chest. First-assist the surgeon throughout the entire four-hour procedure. Close the chest incision at the end of the case.
- 1:00 PM: A brief lunch while writing the post-operative orders for the CABG patient and checking on any urgent pages from the floor.
- 1:30 PM - 4:00 PM: In the OR again, this time for an aortic valve replacement. First-assist the surgeon.
- 4:00 PM: The case finishes. While the patient is being transported to the ICU, check on the morning's CABG patient, who is now settled in the unit. Assess their stability and make any necessary adjustments to their care.
- 4:30 PM - 6:00 PM: Perform "late rounds" on all floor patients, address any new issues that arose during the day, write progress notes, and ensure a smooth handoff to the on-call PA or resident for the night.
- 6:30 PM: Sign out to the on-call provider and head home, ready to do it all again the next day.
This schedule highlights the demanding but incredibly rewarding nature of the role—a dynamic mix of clinical evaluation, precise surgical skill, and critical care management.
Average Cardiothoracic Surgery PA Salary: A Deep Dive
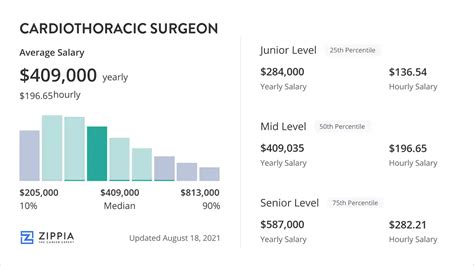
The compensation for a Cardiothoracic Surgery Physician Assistant reflects the high level of skill, long hours, and immense responsibility inherent in the role. It is consistently one of the highest-paying specialties for PAs. While salaries can vary significantly based on the factors we will explore in the next section, we can establish a clear baseline using data from the most reputable sources in the industry.
The American Academy of Physician Associates (AAPA) publishes the most comprehensive and authoritative salary report for the profession. According to the 2023 AAPA Salary Report, which surveyed over 13,000 PAs, those specializing in cardiovascular and thoracic surgery are among the top earners.
- National Median Base Salary (Cardiovascular/Cardiothoracic Surgery): The median base salary for a PA in this specialty was $140,000 per year.
- National Median Total Compensation: When including bonuses, the median total compensation rose to $152,000. Total compensation is a more accurate measure as it reflects the reality of production-based incentives common in surgical fields.
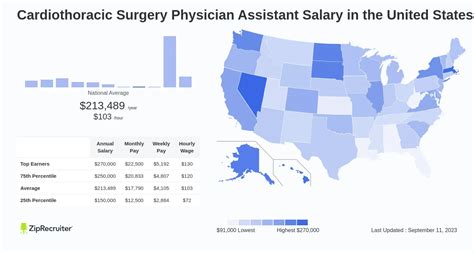
Other reputable salary aggregators provide corroborating data, often reflecting slightly different datasets or calculation methods:
- Salary.com reports a higher average range, suggesting the median base salary for a "Physician Assistant - Surgical" is around $138,401, with the top 10% of earners reaching over $160,563 before bonuses. Their data for CT-specific roles often trends even higher.
- Payscale.com indicates a national average base salary for PAs in Cardiothoracic Surgery is approximately $129,500, with a total pay range (including bonuses and on-call pay) stretching from $103,000 to $168,000+.
- Glassdoor lists an estimated total pay for a "Cardiothoracic PA" around $146,000 per year, with a likely range between $124,000 and $173,000.
Key Takeaway: A conservative estimate for the national average base salary for a CT PA is between $130,000 and $145,000, with average *total compensation* falling between $145,000 and $160,000.
### Salary Progression by Experience Level
A PA's salary is not static; it grows significantly with experience, skill acquisition, and increased autonomy. A newly graduated PA entering a CT surgery role (often through a post-graduate residency) will earn less than a seasoned veteran who can operate with near-independence.
Here is a breakdown of typical salary brackets based on years of experience in the specialty. These figures are estimates synthesized from AAPA data and market analysis.
| Experience Level | Years in Specialty | Typical Base Salary Range | Typical Total Compensation Range | Key Responsibilities & Skills |
| ----------------------- | ------------------ | ----------------------------- | -------------------------------- | ----------------------------------------------------------------------------------------------------- |
| Entry-Level / Resident | 0-1 years | $95,000 - $115,000 | $100,000 - $120,000 | Primarily floor/clinic duties, learning to harvest vein, basic second-assisting, intensive training. |
| Early-Career | 2-4 years | $115,000 - $135,000 | $125,000 - $150,000 | Proficient in EVH, competent first-assisting, managing post-op patients with some supervision. |
| Mid-Career | 5-9 years | $135,000 - $155,000 | $150,000 - $180,000 | Highly autonomous, proficient in all standard procedures, trains junior PAs, manages complex patients. |
| Senior / Lead PA | 10+ years | $155,000 - $180,000+ | $175,000 - $220,000+ | Expert first-assist, often serves as Lead PA, involved in administrative/leadership duties, top producer. |
### Understanding the Full Compensation Package
Base salary is only one piece of the puzzle. Surgical PA compensation packages are often multifaceted and designed to reward productivity and commitment. When evaluating a job offer, it's crucial to look at the entire picture.
- Base Salary: The guaranteed annual income.
- Bonuses: This is a major component. Bonuses can be tied to:
- Productivity: Based on Relative Value Units (RVUs) generated.
- Surgical Volume: A bonus for each case participated in.
- Group Performance: A share of the service line's or practice's profits.
- Quality Metrics: Achieving specific patient outcome goals (e.g., low infection rates).
- According to the AAPA, over 60% of PAs in this specialty receive a bonus, with a median value of $10,000.
- On-Call Pay: CT surgery is not a 9-to-5 job. PAs are required to take call for nights, weekends, and holidays to handle emergencies (e.g., a patient needing to return to the OR for bleeding). This is compensated in several ways:
- A daily stipend for carrying the pager.
- An hourly rate for time spent in the hospital while on call.
- A flat fee per call shift.
- On-call pay can add $10,000 to $30,000+ to an annual salary, depending on the frequency and structure.
- Overtime Pay: For hourly employees, this is pay for hours worked beyond the standard 40-hour week. For salaried employees, some institutions offer extra pay for taking on additional, non-call-related shifts.
- Sign-On Bonus & Relocation Assistance: To attract top talent, especially in high-need areas, employers often offer substantial sign-on bonuses (from $5,000 to $25,000+) and financial assistance for moving expenses.
- Continuing Medical Education (CME) Allowance: Health systems provide an annual allowance (typically $1,500 - $4,000) and paid time off for PAs to attend conferences and maintain their certification and skills.
- Retirement Benefits: This includes 401(k) or 403(b) plans, with the employer matching contribution being a key factor. A strong match (e.g., 5-10% of salary) is a significant part of long-term compensation.
- Other Benefits: Comprehensive health, dental, and vision insurance, life insurance, disability insurance, and coverage for licensing fees and professional memberships (like AAPA and APACVS).
A job offer with a $130,000 base salary but a generous bonus structure, robust on-call pay, and a 10% retirement match could be far more lucrative than a flat $145,000 salary with minimal extras.
Key Factors That Influence Salary

While the national averages provide a solid benchmark, a CT PA's actual salary is determined by a complex interplay of several key factors. Understanding these variables is essential for negotiating the best possible compensation package and for strategically planning your career trajectory to maximize your earning potential. Two PAs with the same job title in the same hospital can have vastly different incomes based on these elements.
### Level of Education and Certification
While a Master's degree from an accredited PA program is the standard entry-level requirement for all Physician Assistants, advanced credentials can significantly impact authority and, consequently, salary in a hyper-specialized field like cardiothoracic surgery.
- Master's Degree (MPAS, MHS, MSc): This is the foundational degree and the prerequisite for taking the PANCE certifying exam. There is generally no significant salary difference between the various types of master's degrees.
- Post-Graduate Residency/Fellowship Certificate: This is perhaps the most impactful educational differentiator for new graduates. Completing a 12-month post-graduate residency in CT surgery (offered at institutions like the Mayo Clinic, Cleveland Clinic, or Duke University) provides intensive, structured training that is highly valued by employers. While the residency year itself comes with a lower stipend (typically $50,000 - $70,000), graduates of these programs are far more competitive. They can bypass the steep learning curve of on-the-job training, command a higher starting salary (often equivalent to a PA with 2-3 years of experience), and are entrusted with more responsibility sooner.
- Certificate of Added Qualifications (CAQ) in Cardiovascular and Thoracic Surgery: Offered by the NCCPA (National Commission on Certification of Physician Assistants), the CAQ is a voluntary credential that demonstrates advanced knowledge and experience in the specialty. To be eligible, a PA needs a PANCE certification, a license, and must meet specific experience, CME, and procedural requirements. Earning the CVT Surgery CAQ is a powerful signal of expertise to an employer. It validates a PA's advanced skill set and can be a significant lever in salary negotiations, often leading to a salary premium or qualifying the PA for a higher-tiered clinical ladder position.
- Doctorate of Medical Science (DMSc): The DMSc is a relatively new doctoral degree for PAs, with concentrations often in leadership, education, or advanced clinical practice. While its direct impact on the salary of a clinical CT PA is still evolving, it can be a major asset for those aspiring to leadership roles. A PA with a DMSc may be better positioned for roles like Director of Advanced Practice Providers (APPs), a position that blends administrative duties with clinical practice and comes with a corresponding executive-level salary.
### Years of Experience
As illustrated in the previous section, experience is arguably the single most powerful driver of salary growth for a CT PA. This is not just about time served; it's about the accumulation of skills, speed, and clinical judgment.
- 0-2 Years (The Learning Phase): New PAs, even those from top programs, require significant training. They are learning to harvest vein efficiently, becoming familiar with the surgeon's preferences, and mastering basic post-operative management. Their value is in their potential, and their salary reflects this training period.
- 3-7 Years (The Proficient Phase): By this stage, the CT PA is a reliable and highly functional member of the team. They are fast and proficient at EVH, can first-assist in a wide range of standard cases (CABG, valves) with minimal guidance, and can autonomously manage most post-operative floor patients. Their increased efficiency directly contributes to the OR's throughput and the service's productivity, justifying a significant salary increase.
- 8+ Years (The Expert Phase): The senior CT PA is a master clinician. They can handle the most complex cases (e.g., dissections, re-operations, LVAD/transplant), often perform other advanced procedures like radial artery harvesting, and may be a robotic first-assistant. Crucially, they serve as a force multiplier for the team by training junior PAs and residents, troubleshooting complex post-operative complications, and acting as the surgeon's true right hand. This level of expertise and leadership commands the highest salaries in the field, with total compensation packages frequently breaking the $200,000 barrier in the right settings.
### Geographic Location
Where you practice has a dramatic impact on your paycheck. This variation is driven by local market demand, the cost of living, and state-level scope-of-practice laws.
- High-Paying States: States with high costs of living and/or large, high-volume cardiac centers tend to offer the highest salaries. According to general PA salary data from the BLS and AAPA, states like California, New York, Alaska, Washington, and Connecticut consistently rank among the highest paying. A CT PA position in a major metropolitan area like Los Angeles, New York City, or San Francisco could offer a base salary 15-30% higher than the national average, though this is offset by a much higher cost of living.
- Lower-Paying States: Conversely, states in the Southeast and parts of the Midwest tend to have lower average salaries, but this is often balanced by a significantly lower cost of living. A $130,000 salary in Alabama or Arkansas may provide a higher quality of life than a $160,000 salary in San Diego.
- Urban vs. Rural/Underserved Areas: The dynamic here can be surprising. While major urban academic centers are hubs of activity, some of the most lucrative opportunities can be found in smaller cities or regional medical centers that are trying to attract scarce talent. A hospital in a less "desirable" location may offer a premium salary, a massive sign-on bonus, and student loan repayment assistance to successfully recruit a skilled CT PA.
- Regional Differences: For example, the Northeast (e.g., Boston, NYC, Philadelphia) is dense with prestigious academic medical centers, creating high demand and competitive salaries. The West Coast is known for high salaries driven by powerful unions (in some systems) and high cost of living.
### Practice Setting & Employer Type
The type of institution you work for is a critical determinant of your compensation structure and overall earning potential.
- Academic Medical Centers: These are large, university-affiliated hospitals.
- Pros: High prestige, cutting-edge cases, involvement in research and teaching, excellent benefits, and often a structured clinical ladder for advancement.
- Cons: Salaries may be slightly lower (5-10%) than top-tier private hospitals. The pace can be slower due to the teaching mission (working with residents and fellows).
- Large Private/Community Hospital Systems: These are often the highest payers. They are run as businesses focused on efficiency and surgical volume.
- Pros: Top-tier salaries, aggressive bonus structures tied to productivity (RVUs), and often very high case volumes.
- Cons: Can be a high-pressure "production" environment. Work-life balance can be challenging.
- Private Surgeon's Group: Working directly for a small group of surgeons who contract with a hospital.
- Pros: Potential for extremely high income via profit-sharing and direct bonuses. More autonomy and a close working relationship with a small team of surgeons.
- Cons: Benefits package may be less robust than a large hospital system. Job security is tied directly to the success and reputation of the surgeons.
- Locum Tenens: This involves working as a temporary, independent contractor to fill short-term needs (e.g., covering for a PA on maternity leave or during a staff shortage).
- Pros: Extremely high daily or weekly pay rates (often equivalent to an annual salary of $250,000+). Offers flexibility and travel opportunities.
- Cons: No benefits (health insurance, retirement), no paid time off, and constant travel. It's a high-income but less stable career model.
### Area of Specialization (Within CT Surgery)
While "Cardiothoracic Surgery" is a specialty, there are sub-specializations within it that can influence complexity and pay.
- Adult Cardiac Surgery: This is the most common area, focusing on coronary artery bypass grafts (CABG) and valve replacements. It forms the baseline for CT PA salaries.
- General Thoracic Surgery: This focuses on the lungs (lobectomies, wedge resections), esophagus, and mediastinum. Salaries are generally