Introduction

Are you meticulous, analytical, and searching for a stable, in-demand career that places you at the very heart of the American healthcare system without requiring direct patient contact? If so, the role of a Clinical Data Coder might be your perfect fit. This profession is one of the most critical, yet often unseen, pillars of modern medicine. It's a field where precision saves more than just money—it ensures the integrity of patient data, powers vital medical research, and keeps the engines of hospitals and clinics running smoothly. For those looking to start this journey, understanding the financial landscape is a crucial first step. The entry-level salary for a clinical data coder in and around Quantico, Virginia, is competitive, typically ranging from $45,000 to $60,000 annually, with significant potential for growth.
I once spoke with a senior coding auditor who shared a story that has always stuck with me. She recalled identifying a single, subtle coding error on a complex cancer treatment case that, if left uncorrected, would have resulted in a patient's insurance wrongfully denying tens of thousands of dollars in coverage. Her diligence didn't just fix a billing issue; it lifted an immense financial and emotional burden from a family during their most vulnerable time. This is the profound, tangible impact of a great clinical data coder. You are not just a data entry specialist; you are a guardian of accuracy, a patient advocate, and a vital link in the healthcare chain.
This comprehensive guide is designed to be your definitive resource for launching a career as a clinical data coder, with a specific focus on the opportunities in Quantico, VA, and the broader Washington D.C. metropolitan area. We will dissect salary expectations, explore the factors that can increase your earning potential, and provide a clear, step-by-step roadmap to get you started.
### Table of Contents
- [What Does a Clinical Data Coder Do?](#what-does-a-clinical-data-coder-do)
- [Average Clinical Data Coder Entry Salary in Quantico, VA: A Deep Dive](#average-clinical-data-coder-entry-salary-in-quantico-va-a-deep-dive)
- [Key Factors That Influence Your Salary](#key-factors-that-influence-your-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in a Clinical Coding Career](#how-to-get-started-in-a-clinical-coding-career)
- [Conclusion: Is a Career in Clinical Coding Right for You?](#conclusion-is-a-career-in-clinical-coding-right-for-you)
---
What Does a Clinical Data Coder Do?
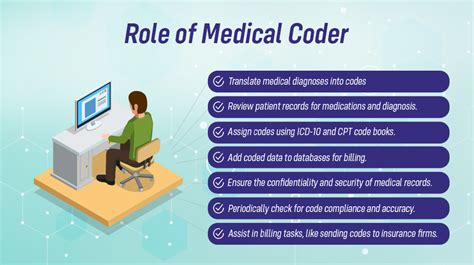
At its core, a Clinical Data Coder, also known as a Medical Coder or Health Information Specialist, is a language translator. They don't translate between spoken languages, but between the detailed language of medicine and the universal language of alphanumeric codes. Every time you visit a doctor, undergo a procedure, or receive a diagnosis, a vast amount of information is generated. It's the coder's job to meticulously review this documentation—physician's notes, lab results, radiologist reports—and translate every billable piece of information into standardized codes.
These codes are part of universally recognized systems, primarily:
- ICD-10-CM (International Classification of Diseases, 10th Revision, Clinical Modification): This system is used to code diagnoses. Everything from a common cold (J00) to a fractured wrist (S62.60-) has a specific code.
- CPT (Current Procedural Terminology): This system is used to code medical, surgical, and diagnostic services and procedures performed by healthcare providers.
- HCPCS Level II (Healthcare Common Procedure Coding System): This system is used to code for products, supplies, and services not included in CPT, such as ambulance services, durable medical equipment, and certain drugs.
The accuracy of this translation is paramount. These codes are the foundation of the entire healthcare revenue cycle. They dictate how much a healthcare provider is reimbursed by insurance companies like Medicare, Medicaid, and private payers. Errors can lead to denied claims, financial losses for the provider, and incorrect bills for the patient. Beyond billing, this coded data is aggregated and used for crucial public health research, tracking disease prevalence, and analyzing treatment outcomes on a massive scale.
### A Day in the Life of an Entry-Level Coder
To make this role more tangible, let's walk through a typical day for an entry-level coder working remotely for a healthcare system in the Northern Virginia area.
- 8:30 AM: Sarah, a newly certified coder, logs into her secure work portal. Her queue is populated with a list of outpatient charts from the previous day's clinic visits. Her primary tool is the Electronic Health Record (EHR) system, like Epic or Cerner, and a specialized coding software encoder.
- 9:00 AM: She opens her first chart: a patient who presented with knee pain. She carefully reads the physician's notes, reviewing the history of the present illness, the physical exam findings, and the final assessment. The doctor diagnosed a "medial meniscus tear." Sarah uses her knowledge of anatomy and medical terminology to navigate her coding software and accurately assign the ICD-10 code `S83.21` (Bucket-handle tear of medial meniscus, current injury).
- 10:15 AM: The next chart is more complex. The physician performed an injection in the patient's shoulder. Sarah must verify the exact medication used and the type of injection (e.g., with or without ultrasound guidance) to select the correct CPT and HCPCS codes. The documentation isn't perfectly clear on the guidance aspect.
- 10:30 AM: Instead of guessing, Sarah drafts a professional, concise query to the physician through the EHR's secure messaging system. This is a critical skill: communicating effectively with providers to clarify documentation without leading them to a specific answer. She flags the chart and moves to the next one while she awaits a response.
- 12:00 PM: Lunch break.
- 1:00 PM: Sarah joins a brief team video call. Her supervisor discusses a recent update from the Centers for Medicare & Medicaid Services (CMS) that affects how certain telehealth visits are coded. Continuous learning is a non-negotiable part of the job.
- 1:30 PM: The physician has responded to her query, clarifying that ultrasound guidance was used. Sarah can now confidently complete the chart, adding the appropriate CPT code for the guided injection. This simple clarification ensures proper reimbursement and data accuracy.
- 3:00 PM: She spends the next couple of hours focused on production coding, working through a variety of cases from dermatology to family practice. She consistently cross-references her official coding manuals (or their digital equivalents) to ensure compliance.
- 4:45 PM: Sarah reviews her daily productivity and accuracy report. Most employers have targets for both the number of charts coded per hour and the accuracy rate (typically 95% or higher). She meets her goals for the day.
- 5:00 PM: She logs out, her work contributing directly to the financial health of her organization and the integrity of national health data.
---
Average Clinical Data Coder Entry Salary in Quantico, VA: A Deep Dive
Determining the precise salary for an entry-level clinical data coder in Quantico, VA, requires a nuanced approach. Quantico itself is a small town, dominated by the Marine Corps base. Consequently, salary data for this specific location is often bundled into the larger, more economically robust regions it belongs to: Prince William County and the Washington-Arlington-Alexandria, DC-VA-MD-WV Metropolitan Statistical Area (MSA). This is actually an advantage for job seekers, as salaries in this high-cost-of-living area are significantly higher than the national average.
### National Salary Benchmarks
First, let's establish a national baseline. The U.S. Bureau of Labor Statistics (BLS) groups Clinical Data Coders under the broader category of "Medical Records and Health Information Specialists."
- According to the most recent BLS data (May 2023), the national median annual wage for this occupation was $48,780, or approximately $23.45 per hour.
- The lowest 10 percent earned less than $34,570, which often represents true entry-level or uncertified positions in low-cost-of-living areas.
- The highest 10 percent earned more than $81,320, reflecting the earning potential for experienced, specialized, or management-level coders.
*(Source: U.S. Bureau of Labor Statistics, Occupational Outlook Handbook, Medical Records and Health Information Specialists. Data retrieved October 2024.)*
### Local Salary Data: Quantico and the Washington D.C. Metro Area
The Quantico area benefits immensely from its proximity to Washington D.C., a hub for government, healthcare, and technology. This drives up both the cost of living and wages. Reputable salary aggregators confirm this trend.
- Salary.com: Reports that the average Medical Coder I (entry-level) salary in Quantico, VA, as of September 2024, is $50,076, with a typical range falling between $44,057 and $57,212. This is a highly specific and valuable data point.
- Payscale.com: For the broader Washington D.C. area, the average salary for a Medical Coder is around $59,500. While not exclusively for entry-level, this figure indicates the strong earning environment of the region.
- Glassdoor.com: Lists the estimated total pay for a Medical Coder in the Washington D.C. area as $64,000 per year, with a likely range of $53,000 to $78,000. This often includes base pay plus potential additional compensation.
Synthesizing this data, a newly certified, entry-level clinical data coder in the Quantico, VA, region can realistically expect to earn between $45,000 and $60,000 per year. Candidates with a relevant degree (like an Associate's in Health Information Technology) and a strong certification (like the CPC) will likely land at the higher end of this range.
### Salary Growth by Experience Level in the Quantico/D.C. Area
One of the most attractive aspects of a coding career is the clear and rewarding trajectory for salary growth as you gain experience and expertise. Here is a typical progression in the competitive D.C. metro market:
| Experience Level | Years of Experience | Typical Salary Range (Quantico/D.C. Metro Area) | Key Responsibilities & Milestones |
| :--- | :--- | :--- | :--- |
| Entry-Level Coder | 0-2 Years | $45,000 - $60,000 | Production coding, learning EHR systems, achieving accuracy/productivity targets, removing apprentice status from certification (e.g., CPC-A to CPC). |
| Mid-Career Coder | 3-8 Years | $60,000 - $75,000 | Handling more complex charts (e.g., surgical or inpatient), mentoring new coders, possibly specializing in a specific medical field like cardiology or oncology. |
| Senior Coder / Auditor | 9+ Years | $75,000 - $90,000+ | Auditing other coders' work for quality assurance, training staff, serving as a subject matter expert, resolving complex billing issues, Clinical Documentation Improvement (CDI). |
| Coding Manager / Director | 12+ Years | $90,000 - $120,000+ | Managing a team of coders, overseeing department budgets, developing coding policies, ensuring compliance with federal regulations, strategic planning for the revenue cycle. |
*(Salary ranges are estimates compiled from BLS, Salary.com, and industry reports for the Washington D.C. MSA, updated for 2024.)*
### Beyond the Base Salary: Total Compensation
Your salary is just one piece of the puzzle. When evaluating a job offer, it's crucial to consider the full compensation package, which can add significant value.
- Bonuses: Some organizations, particularly in the private sector, offer performance-based bonuses tied to meeting or exceeding productivity and accuracy goals.
- Health Insurance: In the U.S., a comprehensive health insurance plan with low premiums and deductibles is a major financial benefit.
- Retirement Savings: Look for employers that offer a 401(k) or 403(b) plan, especially those with a generous matching contribution. This is essentially free money for your retirement.
- Paid Time Off (PTO): A generous PTO policy (including vacation, sick leave, and holidays) is essential for work-life balance.
- Professional Development: Many employers will pay for your annual certification maintenance fees, continuing education units (CEUs), and even tuition for advanced degrees or specialized certifications. This is a direct investment in your career growth.
---
Key Factors That Influence Your Salary
While location and experience are primary drivers of your salary, several other factors can significantly impact your earning potential. Aspiring and current coders who strategically focus on these areas can accelerate their career and compensation growth far beyond the average.
###
1. Education and Certifications: The Cornerstones of Value
In clinical coding, certifications are often more influential than the specific level of a college degree, but the combination is powerful.
Education:
- High School Diploma/GED: This is the minimum requirement to enter a coding certification program. While you can find a job with just a diploma and a certification, your starting salary and opportunities may be on the lower end.
- Certificate/Diploma Program: These focused programs (typically 9-12 months) are the most common entry point. They provide the core knowledge of anatomy, physiology, and coding guidelines needed to sit for a certification exam.
- Associate of Applied Science (A.A.S.) in Health Information Technology (HIT): This two-year degree is highly regarded. It provides a deeper understanding of the entire health information lifecycle, including data management, legal principles, and revenue cycle management. Graduates with an HIT degree who also hold a certification are often preferred by employers and may command a starting salary at the top of the entry-level range. Earning this degree also makes you eligible to sit for the Registered Health Information Technician (RHIT) exam from AHIMA.
- Bachelor of Science (B.S.) in Health Information Management (HIM): This four-year degree is the gold standard for those with leadership aspirations. It positions you for roles in management, compliance, data analytics, and informatics. Graduates are eligible for the Registered Health Information Administrator (RHIA) credential, leading to significantly higher-paying roles outside of pure production coding.
Certifications: Your Non-Negotiable Asset
Certification is the universal standard that proves your competence to employers. The two main credentialing bodies are AAPC and AHIMA.
- Certified Professional Coder (CPC®) from AAPC: This is the most recognized certification for outpatient and physician-based coding. Many entry-level jobs list the CPC as a requirement. New coders pass the exam to become a CPC-A (Apprentice). The "A" can be removed after two years of work experience (or one year of experience plus 80 hours of coding education). A full CPC is more valuable than a CPC-A.
- Certified Coding Specialist (CCS®) from AHIMA: This is a mastery-level certification that demonstrates proficiency in coding in both inpatient hospital settings (using ICD-10-PCS for procedures) and outpatient settings. It is generally considered more difficult to obtain than the CPC and is highly valued, often leading to higher pay.
- Specialty Certifications: Once you have a core credential and experience, obtaining specialty certifications can provide a significant salary bump. These signal expertise in a complex and often higher-reimbursing area. Examples include:
- Certified Risk Adjustment Coder (CRC®): In high demand due to the shift to value-based care.
- Certified Inpatient Coder (CIC®): For hospital inpatient coding.
- Certified Outpatient Coder (COC®): For hospital outpatient departments/ambulatory surgery centers.
- Specialty-specific credentials like Certified Cardiology Coder (CCC™) or Certified General Surgery Coder (CGSC™).
An investment in certification pays direct dividends. According to AAPC's 2024 salary survey, coders with at least one certification earn, on average, 29% more than their uncertified counterparts.
###
2. Years of Experience: The Path from Novice to Expert
As shown in the salary table, experience is a powerful driver. Here’s why your value increases so dramatically over time:
- Speed and Efficiency (Years 0-2): New coders are focused on learning the systems and building accuracy. As you gain experience, your speed naturally increases, allowing you to process more charts per hour while maintaining high accuracy.
- Handling Complexity (Years 3-5): You move from routine cases (like strep throat or simple fractures) to more complex scenarios involving multiple chronic conditions, surgeries, or ambiguous documentation. You become adept at provider queries and navigating complex coding guidelines.
- Subject Matter Expertise (Years 5-10): You may become the go-to person for a specific specialty, like orthopedics or oncology. You understand the nuances of that field's procedures and common diagnoses, making you an invaluable asset.
- Mentorship and Leadership (Years 10+): Senior coders transition from pure production to quality assurance and leadership. They audit, train, and guide junior coders, directly impacting the entire department's performance. This shift from "doing" to "enabling" is what warrants top-tier salaries.
###
3. Geographic Location: The Cost-of-Living Factor
Where you work matters immensely. The high cost of living in the Washington D.C. metropolitan area directly translates to higher salaries for clinical coders compared to other parts of Virginia or the country.
Salary Comparison by Location (Medical Coder, 2-4 Years Experience)
| Location | Typical Salary Range | Cost of Living Index (100 = National Avg) |
| :--- | :--- | :--- |
| Quantico / Northern Virginia | $58,000 - $72,000 | ~140 |
| Richmond, VA | $52,000 - $65,000 | ~96 |
| Roanoke, VA | $48,000 - $60,000 | ~80 |
| National Average | $50,000 - $63,000 | 100 |
*(Source: Data compiled from Payscale and Salary.com regional data, 2024. Cost of Living Index from BestPlaces.net.)*
The rise of remote work has slightly complicated this factor. Many coders now work from home for companies based in different states. In these cases, companies may pay based on:
1. The company's location: A coder living in a low-cost area could earn a high salary working for a company based in New York City.
2. The employee's location: Some companies adjust salaries based on the employee's local cost of living.
3. A national standard: A single pay scale regardless of location.
For those in Quantico, seeking remote work from companies based in high-cost areas can be a highly effective salary maximization strategy.
###
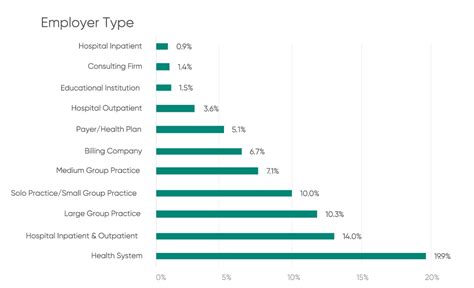
4. Company Type & Size: The Impact of Your Employer
The type of organization you work for has a distinct impact on salary, culture, and benefits.
- Large Hospital Systems (e.g., INOVA, Sentara, HCA): These are often the highest-paying employers. They offer robust benefits, clear career ladders, and opportunities for specialization. The work can be demanding with strict productivity targets.
- Government/Federal Contractors: Given Quantico's proximity to Washington D.C. and its own large federal presence, government jobs are a significant opportunity. Roles with the Department of Veterans Affairs (VA), Department of Defense (DoD), or contractors supporting them often pay on the General Schedule (GS) scale. A certified coder could start at a GS-5 or GS-6 level and advance to GS-9 or higher as a senior coder or auditor, with excellent job security and federal benefits.
- Small Physician Practices: These may offer lower starting salaries but can provide a more intimate work environment and a broader range of responsibilities. You might be involved in billing and patient scheduling in addition to coding.
- Third-Party Coding Companies (e.g., Optum, nThrive): These firms are hired by hospitals and clinics to handle their coding. They offer a huge variety of work and are often leaders in remote opportunities. Pay is competitive but can be heavily tied to productivity metrics.
- Insurance Companies (Payers): Working on the "other side" for an insurer like Anthem or Aetna involves reviewing claims for accuracy, fraud, and abuse. These roles often require experienced coders and can be very stable and well-compensated.
###
5. In-Demand Skills and Specializations
Beyond your core coding ability, developing a portfolio of high-value skills can set you apart and justify a higher salary.
- Inpatient Coding: Coding for hospital stays is significantly more complex than outpatient coding. It uses the ICD-10-PCS procedural coding system and a payment methodology based on Diagnosis-Related Groups (DRGs). Coders with proven inpatient skills (often with a CCS or CIC certification) are in high demand and earn a premium.
- Surgical Coding: Accurately coding complex surgical procedures requires a deep understanding of anatomy and surgical techniques. It's a lucrative specialization.
- Risk Adjustment Coding (Hierarchical Condition Categories - HCC): This involves reviewing patient charts to ensure all chronic conditions are properly documented and coded. It directly impacts the reimbursement that health plans receive for patients, especially in Medicare Advantage plans. Coders with a CRC certification are highly sought after.
- Clinical Documentation Improvement (CDI): CDI specialists work proactively with physicians to ensure medical documentation is complete and specific *before* coding. This role requires excellent communication skills and clinical knowledge and is a high-paying career path that bridges clinical care and coding.
- EHR/Software Proficiency: Expertise in major EHR systems like Epic and Cerner is a highly marketable skill. Experience with specialized coding encoders and computer-assisted coding (CAC) software is also a plus.
- Data Analytics and Auditing: Skills in using data to identify trends, audit for compliance, and present findings are hallmarks of a senior-level professional and command top dollar.
---
Job Outlook and Career Growth

The future for clinical data coders is exceptionally bright, both nationally and in the healthcare-rich Northern Virginia region. This career offers a rare combination of high demand, stability, and a clear path for advancement.
### A Profession on the Rise
The U.S. Bureau of Labor Statistics projects that employment for Medical Records and Health Information Specialists will grow by 7 percent from 2022 to 2032, which is "much faster than the average for all occupations."
- Projected Job Openings: The BLS anticipates about 15,200 openings for these specialists each year, on average, over the decade. These openings are expected to result from both the creation of new jobs and the need to replace workers who transfer to different occupations or exit the labor force, such as to retire.
*(Source: U.S. Bureau of Labor Statistics, Occupational Outlook Handbook, retrieved October 2024.)*
What's driving this robust growth?
1. Aging Population: As the large baby-boomer population ages, they will require more medical services, leading to a higher volume of claims that need to be processed and coded.