Introduction

Are you searching for a stable, in-demand career that places you at the very heart of the healthcare industry, but without the hands-on clinical responsibilities? Do you possess a keen eye for detail, a knack for investigation, and a desire for a role that offers significant growth potential? If so, a career in medical coding and billing might be the perfect fit for you. This profession is the financial backbone of healthcare, a critical function that ensures medical providers are properly compensated for their life-saving services. The average coding and billing salary reflects this importance, with experienced and certified professionals earning a comfortable and rewarding living. For many, this path offers the ideal blend of purpose, stability, and financial security in a rapidly growing field.
I once worked alongside a hospital's revenue cycle management team, and I was consistently amazed by their diligence. A single misplaced decimal or an incorrect diagnostic code could mean the difference between a claim being paid in full or being rejected, a difference of thousands of dollars that directly impacted the hospital's ability to care for patients. It was a powerful lesson in how these behind-the-scenes professionals are the unsung heroes of healthcare finance, wielding knowledge and precision to keep the entire system running.
This comprehensive guide is designed to be your definitive resource, exploring every facet of a medical coding and billing career. We will dissect salary expectations, uncover the factors that can maximize your earning potential, analyze the promising job outlook, and provide a clear, step-by-step roadmap to get you started.
### Table of Contents
- [What Does a Medical Coder and Biller Do?](#what-does-a-medical-coder-and-biller-do)
- [Average Medical Coding and Billing Salary: A Deep Dive](#average-medical-coding-and-billing-salary-a-deep-dive)
- [Key Factors That Influence Your Coding and Billing Salary](#key-factors-that-influence-your-coding-and-billing-salary)
- [Job Outlook and Career Growth in Coding and Billing](#job-outlook-and-career-growth-in-coding-and-billing)
- [How to Get Started in a Medical Coding and Billing Career](#how-to-get-started-in-a-medical-coding-and-billing-career)
- [Conclusion: Is a Career in Medical Coding and Billing Right for You?](#conclusion-is-a-career-in-medical-coding-and-billing-right-for-you)
---
What Does a Medical Coder and Biller Do?
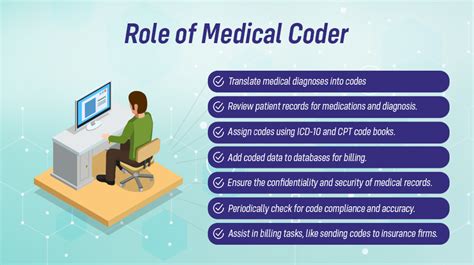
At its core, the role of a medical coder and biller is to manage the healthcare revenue cycle. While the titles are often used interchangeably, they represent two distinct, yet deeply interconnected, functions. Think of them as two halves of the same coin, both essential for turning a patient visit into a paid claim.
Medical Coding: The Language of Healthcare
A medical coder is a translator. Their primary responsibility is to review a patient's medical records—including physician's notes, lab results, and procedural reports—and translate every piece of information into a set of universal alphanumeric codes. This is not a simple data entry task; it's an analytical process requiring a deep understanding of medical terminology, anatomy, and complex coding guidelines.
The main code sets they use are:
- ICD-10-CM (International Classification of Diseases, 10th Revision, Clinical Modification): These codes represent a patient's diagnoses, symptoms, and conditions. For example, "J45.909" is the code for an unspecified asthma attack.
- CPT (Current Procedural Terminology): These codes represent the services and procedures performed by the healthcare provider, such as a physical exam, a blood draw, or a major surgery.
- HCPCS Level II (Healthcare Common Procedure Coding System): These codes cover supplies, equipment, and services not included in CPT, like ambulance services, durable medical equipment, and certain drugs.
A coder’s job is to ensure that the codes assigned are accurate, complete, and fully supported by the medical documentation. This accuracy is paramount, as these codes dictate the entire financial narrative of a patient encounter.
Medical Billing: Securing the Revenue
Once the coder has translated the patient visit into a set of codes, the medical biller takes over. The biller is the financial specialist who uses these codes to create a "superbill" or claim. This claim is a formal request for payment sent to the patient's insurance company (the payer).
A biller's responsibilities include:
- Claim Creation: Inputting codes, patient demographics, and insurance information into a claim form.
- Claim Submission: Electronically submitting claims to various payers, from large private insurers like UnitedHealthcare and Aetna to government programs like Medicare and Medicaid.
- Payment Posting: Accurately posting payments received from insurance companies.
- Denial Management: Investigating why a claim was denied, correcting any errors, and resubmitting it for payment. This is a critical, problem-solving aspect of the job.
- Patient Billing: Creating and sending statements to patients for their portion of the bill (deductibles, copayments, etc.).
### A Day in the Life of a Medical Coder/Biller
To make this more concrete, let's imagine a typical day for "Sarah," a certified coder working remotely for a multi-physician cardiology practice.
- 8:30 AM: Sarah logs into her secure portal and accesses the Electronic Health Record (EHR) system. Her queue is populated with patient charts from the previous day.
- 9:00 AM: She opens the first chart. The patient presented with chest pain. Sarah meticulously reads the physician’s notes, EKG results, and lab work. She identifies the final diagnosis as "unstable angina" and the procedures performed as a comprehensive office visit and an EKG. She assigns the correct ICD-10 and CPT codes, ensuring they meet medical necessity guidelines.
- 11:00 AM: An instant message pops up from one of the physicians. He has a question about the appropriate code for a new, experimental procedure. Sarah researches the code set and payer guidelines, provides an answer, and flags the chart for follow-up.
- 12:30 PM: Lunch break.
- 1:30 PM: Sarah shifts her focus to the billing software. She reviews a report of denied claims from the previous week. One claim for a cardiac stress test was denied for "lack of pre-authorization." She investigates the patient's file, finds the pre-authorization number that was mistakenly omitted, appends it to the claim, and resubmits it electronically.
- 3:30 PM: She receives an email about an upcoming update to the ICD-10 code set. She bookmarks the resource from the American Academy of Professional Coders (AAPC) to review later and ensure she's up-to-date for her continuing education units (CEUs).
- 5:00 PM: Sarah finishes her last chart, runs a report summarizing the day's coded encounters, and logs off, having played a vital role in securing over $15,000 in revenue for the practice.
---
Average Medical Coding and Billing Salary: A Deep Dive

One of the most compelling aspects of this career is its solid and reliable earning potential. A coding and billing salary is influenced by numerous factors, but we can establish a strong baseline using data from authoritative sources. It’s important to note that professionals who hold both coding and billing skills, especially with certification, are often more valuable and can command higher salaries.
### National Averages and Salary Ranges
The most reliable government source, the U.S. Bureau of Labor Statistics (BLS), groups medical coders under the category of "Medical Records and Health Information Specialists." As of May 2023, the BLS reports the following:
- Median Annual Wage: $48,780 (or $23.45 per hour). The median is the wage at which half the workers in an occupation earned more than that amount and half earned less.
- Salary Range: The lowest 10 percent earned less than $34,440, while the highest 10 percent earned more than $81,320.
This provides a solid, big-picture view. However, industry-specific surveys from professional organizations offer an even more granular look, particularly highlighting the impact of certification.
The American Academy of Professional Coders (AAPC), the largest training and credentialing organization for this field, conducts an annual salary survey that is highly regarded. According to the 2024 AAPC Salary Survey, which reflects 2023 salary data:
- Average Salary (All Credentials): $64,895
- Average Salary for Coders (Holding at least one CPC credential): $62,207
- Average Salary for Billers (Holding a CPB credential): $58,680
The significant difference between the BLS median and the AAPC average can be attributed to the fact that the AAPC survey exclusively polls its credentialed members, who generally have higher qualifications and earning power than the workforce as a whole. This powerfully illustrates the financial benefit of earning a professional certification.
### Salary by Years of Experience
Like any profession, experience is a primary driver of income growth. A new coder with a fresh certification will start at one level, but with dedication and skill development, their salary can increase substantially over their career.
Here is a typical salary progression based on data aggregated from sources like Payscale and the AAPC survey:
| Experience Level | Typical Years of Experience |
| :--- | :--- |
| Entry-Level (e.g., CPC-A) | 0-2 Years |
| Mid-Career Coder | 3-9 Years |
| Senior/Experienced Coder | 10-19 Years |
| Veteran/Lead Coder/Auditor | 20+ Years |
| Average Annual Salary Range |
| :--- |
| $42,000 - $52,000 |
| $55,000 - $68,000 |
| $65,000 - $75,000 |
| $70,000 - $85,000+ |
*Source: Synthesized data from Payscale.com, Salary.com, and the 2024 AAPC Salary Survey.*
An entry-level coder often holds an "Apprentice" (CPC-A) designation, which signals to employers that they have the knowledge but lack extensive hands-on experience. After one to two years of work and meeting specific educational requirements, the "A" can be removed, typically corresponding with a significant salary bump. As professionals gain more experience, they can move into roles like medical auditing, compliance, or management, which offer even higher salary potential.
### Breakdown of Compensation: Beyond the Base Salary
Your total compensation is more than just your hourly wage or annual salary. Many medical coding and billing positions come with additional financial benefits that enhance the overall package.
- Bonuses: Annual or quarterly bonuses are common, especially in private practices or for-profit hospital systems. These are often tied to performance metrics such as coding accuracy rates (e.g., maintaining a 95% or higher accuracy), productivity (number of charts coded per hour), or the team's success in reducing claim denial rates. Bonuses can range from a few hundred to several thousand dollars per year.
- Profit Sharing: While less common, some smaller, private physician practices may offer profit-sharing plans, where a portion of the practice's annual profits is distributed among employees. This directly incentivizes coders and billers to maximize revenue through accurate and efficient work.
- Overtime Pay: For non-exempt (hourly) employees, overtime is a potential source of additional income, particularly during busy periods like the end of a fiscal year or when implementing new coding updates.
- Benefits Package: This is a crucial part of total compensation. A strong benefits package can be worth thousands of dollars annually. Look for:
- Health Insurance: Comprehensive medical, dental, and vision coverage.
- Retirement Savings: Access to a 401(k) or 403(b) plan, often with an employer match.
- Paid Time Off (PTO): Including vacation, sick leave, and holidays.
- Professional Development: Many employers will pay for your annual association memberships (e.g., AAPC) and the cost of continuing education units (CEUs) required to maintain your certifications. This is a highly valuable perk that supports your career growth.
When evaluating a job offer, it's essential to look at the entire compensation structure—base salary, bonus potential, and the value of the benefits—to understand your true earning potential.
---
Key Factors That Influence Your Coding and Billing Salary
While the national averages provide a useful benchmark, your individual coding and billing salary will be determined by a specific set of factors. Understanding and strategically navigating these elements is the key to maximizing your income and accelerating your career trajectory. This section provides an exhaustive breakdown of the variables that matter most.
### `
` Professional Certifications: The Single Biggest Salary Booster `
`In the world of medical coding and billing, certification is not just a line on a resume—it is the gold standard that validates your expertise and unlocks higher earning potential. Employers overwhelmingly prefer, and often require, certified candidates because it guarantees a proven level of competency and commitment to the profession.
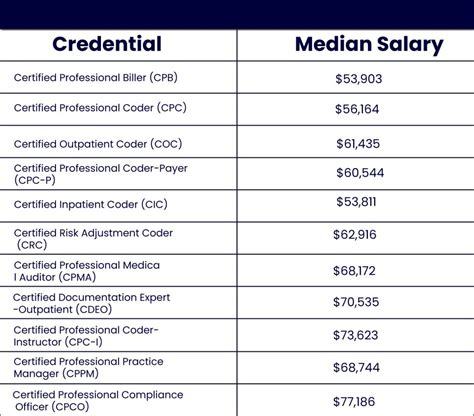
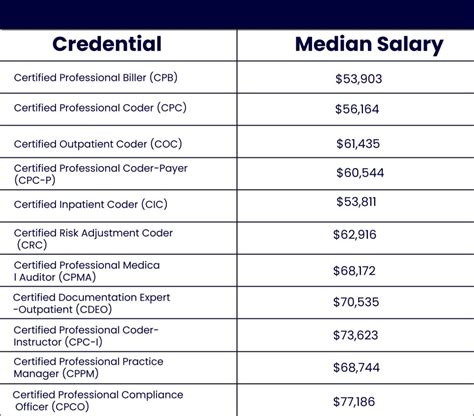
According to the 2024 AAPC Salary Survey, professionals holding at least one certification earn, on average, 30% more than their non-certified counterparts. The specific certification(s) you hold will directly impact your salary.
Core Certifications and Their Salary Impact:
- CPC (Certified Professional Coder): Offered by the AAPC, this is the most recognized certification for physician-based (outpatient) coding. It demonstrates proficiency in CPT, ICD-10-CM, and HCPCS Level II.
- *Average Salary with CPC:* $62,207 (AAPC 2024)
- CCS (Certified Coding Specialist): Offered by the American Health Information Management Association (AHIMA), this credential is highly respected for its focus on hospital-based (inpatient) coding, which is often more complex.
- *Average Salary with CCS:* Often slightly higher than the CPC, typically in the $65,000 - $75,000 range depending on setting and experience.
- CPB (Certified Professional Biller): Also from the AAPC, this certification focuses on the entire billing process, from claim submission to denial management and compliance.
- *Average Salary with CPB:* $58,680 (AAPC 2024)
The Power of Multiple and Specialized Certifications:
The real salary growth comes from stacking credentials. As you gain experience, earning specialized certifications can dramatically increase your value.
- CPC + Specialty Certification: A coder with a CPC who adds a specialty credential in a complex area like Cardiology (CCC) or General Surgery (CGSC) can often earn $5,000 to $15,000 more per year.
- CRC (Certified Risk Adjustment Coder): This is one of the highest-paying certifications. Risk adjustment coding is crucial for Medicare Advantage plans and is in extremely high demand.
- *Average Salary with CRC:* $71,833 (AAPC 2024)
- CPMA (Certified Professional Medical Auditor): Auditors review the work of other coders for accuracy and compliance. This is an advanced role requiring deep expertise.
- *Average Salary with CPMA:* $77,414 (AAPC 2024)
The data is clear: investing in certifications pays significant dividends. Professionals with two credentials average $71,118, and those with three or more credentials average $79,848, according to the AAPC.
### `
` Level of Education `
`While certification is paramount, your formal education also plays a role.
- High School Diploma / GED: This is the minimum requirement to enter a certificate program. It is possible to have a successful career with only a diploma and strong certifications.
- Certificate Program: This is the most common educational path. These focused programs (typically 6-12 months) are offered by vocational schools, community colleges, and online providers like the AAPC. They prepare you directly for the certification exam.
- Associate's Degree (e.g., in Health Information Technology): An associate's degree can provide a broader base of knowledge and may be preferred by some larger employers, particularly hospitals. It can lead to a slightly higher starting salary and may be a stepping stone to management roles.
- Bachelor's Degree (e.g., in Health Information Management - HIM): A bachelor's degree is typically required for higher-level management and leadership positions, such as HIM Director or Revenue Cycle Manager. These roles come with significantly higher salaries, often exceeding $100,000. For a standard coding role, a bachelor's is generally not required, but it opens doors to the highest rungs of the career ladder.
### `
` Years of Experience `
`As detailed in the previous section, experience is a linear driver of salary growth. Here's a more detailed look at the career and salary trajectory:
- Apprentice (0-2 years): Your primary goal is to absorb as much as you can and get your "A" removed from your CPC credential. You'll likely handle more straightforward cases and work under close supervision. Salary is in the entry-level range ($42k - $52k).
- Journey-Level Coder (3-9 years): You are now a fully proficient coder, trusted to handle a wide range of cases with minimal supervision. You've likely found a specialty you enjoy. Your salary sees its most significant growth during this period, moving firmly into the $55k - $68k range.
- Senior Coder / Mentor (10-19 years): At this stage, you are an expert. You handle the most complex cases (e.g., multi-system surgeries, rare diagnoses), mentor junior coders, and may serve as a resource for physicians. You may also be involved in preliminary audits. Salary solidifies in the $65k - $75k+ range.
- Subject Matter Expert / Auditor / Manager (20+ years): Veteran professionals often move beyond daily production coding into specialized, high-value roles. They may become full-time auditors (CPMA), compliance specialists, educators, or department managers. These positions leverage decades of experience and command the highest salaries in the field, often $80,000 to $95,000 or more.
### `
` Geographic Location `
`Where you live and work has a massive impact on your salary, largely due to variations in cost of living and regional demand. A high salary in a high-cost-of-living city may not have the same purchasing power as a slightly lower salary in an affordable area.
Top-Paying States for Medical Coders and Billers:
According to both BLS data and the 2024 AAPC survey, the following states consistently offer the highest average salaries:
1. California: Average salaries often exceed $75,000, especially in major metro areas like San Francisco and Los Angeles.
2. New Jersey: High concentration of pharmaceutical and healthcare companies drives salaries up, averaging around $73,000.
3. District of Columbia (D.C.): Averages around $73,000, driven by government and large hospital systems.
4. Washington: Strong healthcare sector in the Seattle area pushes averages to about $71,000.
5. Massachusetts: Boston's world-class hospitals and biotech industry contribute to an average salary around $70,000.
Lower-Paying States:
Conversely, states in the Southeast and parts of the Midwest tend to have lower average salaries, often in the $50,000 - $55,000 range. States like Alabama, Arkansas, and Mississippi fall into this category. However, the lower cost of living in these areas can offset the salary difference.
The Rise of Remote Work:
The pandemic accelerated the trend of remote work in medical coding. This has begun to flatten salary landscapes somewhat. Some national employers are moving toward standardized pay bands regardless of location, while others still adjust pay based on the employee's geographic "zone." A remote job can be a huge advantage, potentially allowing you to earn a salary based on a higher-paying region while living in a lower-cost-of-living area.
### `
` Work Setting and Company Type `
`The type of organization you work for is another key salary determinant.
- Large Hospital Systems: These are often the highest-paying employers. They handle a high volume of complex inpatient and outpatient cases, requiring specialized, experienced coders. They also tend to have structured salary grades and better benefits. Inpatient hospital coders, in particular, often earn a premium.
- Physician's Offices / Small to Mid-Sized Clinics: Salaries here may be slightly lower than at large hospitals, but the work environment can be more tight-knit. Coders may also have broader responsibilities, including billing and front-office tasks.
- Specialty Practices (e.g., Oncology, Orthopedics, Cardiology): Coding for specialties is more complex and requires a deeper knowledge base. As such, these roles often command higher-than-average salaries.
- Third-Party Billing Companies: These companies handle coding and billing for multiple clients. The pay can be competitive, and the environment is often fast-paced and production-driven.
- Government (e.g., VA Hospitals): Government jobs are known for their excellent benefits, job security, and structured pay scales (like the GS system). While the base salary might not be the absolute highest, the total compensation package is often superior.
- Freelance/Consulting: Highly experienced coders and auditors can work for themselves. This path offers the highest earning potential and flexibility, but it comes with the challenges of running a business, finding clients, and managing your own benefits and taxes. Successful consultants can earn well over $100,000 annually.
### `
` In-Demand Skills and Specializations `
`Beyond formal credentials, a specific set of skills will make you a more valuable—and better-paid—professional.
- Technical Proficiency: Expertise in major EHR/EMR systems like Epic and Cerner is a huge plus. Advanced skills in Microsoft Excel for data analysis and reporting are also highly valued.
- Anatomy and Physiology Knowledge: A deep, clinical-level understanding of the human body is non-negotiable for accurate coding, especially in surgical and specialty fields.
- Understanding of Payer Policies: The ability to navigate the complex and ever-changing rules of Medicare, Medicaid, and major commercial insurance companies is a critical skill for both coders and billers.
- Auditing and Compliance: Skills in identifying coding errors, understanding compliance regulations like HIPAA, and providing feedback to other coders are hallmarks of a senior-level professional.
- Soft Skills:
- Communication: The ability to write clear, concise queries to physicians to clarify documentation is essential for accuracy and revenue integrity.