Introduction

For anyone dreaming of a career in medicine, the path is paved with immense dedication, intellectual rigor, and a profound desire to heal. But as you stand at the beginning of this journey, a crucial question often arises: Should you pursue a Doctor of Medicine (M.D.) or a Doctor of Osteopathic Medicine (D.O.) degree? This decision is frequently followed by a more pragmatic, yet equally important query: "Is there a difference between a D.O. salary and an M.D. salary?" It's a question that cuts to the heart of long-term career planning, financial stability, and the perceived value of your hard-earned credentials.
The simple answer, which we will explore in exhaustive detail, is that the choice between an M.D. and a D.O. has a negligible direct impact on your earning potential. The letters after your name are far less important than the specialty you choose, the location where you practice, and the type of healthcare system you work within. Physicians in the United States are among the highest-paid professionals, with the U.S. Bureau of Labor Statistics (BLS) reporting a median annual salary of $229,300 for physicians and surgeons in May 2022. However, this single number barely scratches the surface of a compensation landscape that can range from approximately $150,000 for some primary care roles to well over $700,000 for highly specialized surgeons.
I recall a conversation years ago with a family friend, a pre-med student agonizing over her application strategy. She was convinced that applying to D.O. schools was a "backup plan" that would relegate her to a lower salary tier for life. Years later, she is a thriving and highly compensated D.O. specializing in emergency medicine, earning a salary identical to her M.D. colleagues in the same hospital group. Her story underscores a fundamental truth: competence, specialization, and business acumen—not the type of medical degree—are the true drivers of a physician's financial success.
This guide is designed to be your definitive resource on the topic of D.O. vs. M.D. salary. We will dissect every factor that influences physician compensation, backed by the latest data from authoritative sources. We will demystify the two educational paths, explore the job outlook, and provide a clear roadmap for how to begin your own journey into this incredibly rewarding field.
### Table of Contents
- [M.D. vs. D.O.: Understanding the Degrees Before the Dollars](#md-vs-do-understanding-the-degrees-before-the-dollars)
- [Average D.O. vs. M.D. Salary: A Deep Dive](#average-do-vs-md-salary-a-deep-dive)
- [Key Factors That Influence Physician Salary](#key-factors-that-influence-physician-salary)
- [Job Outlook and Career Growth for Physicians](#job-outlook-and-career-growth-for-physicians)
- [How to Become a Physician: The M.D. and D.O. Pathways](#how-to-become-a-physician-the-md-and-do-pathways)
- [Conclusion: Focusing on What Truly Matters](#conclusion-focusing-on-what-truly-matters)
M.D. vs. D.O.: Understanding the Degrees Before the Dollars
Before we can meaningfully compare salaries, it's essential to understand the fundamental similarities and subtle differences between the two degrees that grant full medical practice rights in the United States. In the eyes of the public, patients, hospitals, and insurance companies, both M.D.s and D.O.s are simply "doctors." They undergo similarly rigorous training, are held to the same high standards of care, and have identical rights and responsibilities.
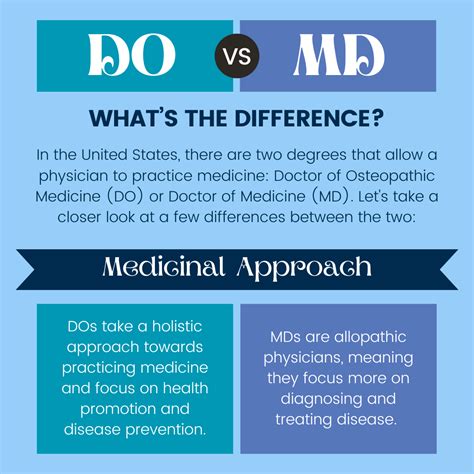
Doctor of Medicine (M.D.)
The M.D. degree comes from the allopathic school of medicine, which is the most common form of medical training worldwide. The allopathic approach focuses on diagnosing and treating diseases and conditions using evidence-based practices, such as medication, surgery, and other established therapies. M.D.s are trained to target specific symptoms and diseases to restore patient health.
Doctor of Osteopathic Medicine (D.O.)
The D.O. degree comes from the osteopathic school of medicine, a philosophy that originated in the late 19th century. Osteopathic medicine embraces all the tools and technologies of modern medicine but also includes a more holistic philosophy. It emphasizes the interconnectedness of the body's systems and the importance of the musculoskeletal system in overall health. In addition to the standard medical curriculum, D.O. students receive several hundred hours of training in a technique called Osteopathic Manipulative Treatment (OMT). OMT involves using the hands to diagnose, treat, and prevent illness or injury by moving a patient's muscles and joints.
The Overwhelming Similarities
Despite the philosophical distinction, the practical realities of training and practice are nearly identical:
- Licensing: Both M.D.s and D.O.s must pass national board licensing exams to practice. M.D.s typically take the United States Medical Licensing Examination (USMLE) series, while D.O.s traditionally take the Comprehensive Osteopathic Medical Licensing Examination (COMLEX-USA). However, many D.O.s also choose to take the USMLE to enhance their competitiveness for residency programs.
- Residency Training: Since 2020, the residency and fellowship application process has been unified into a single system managed by the Accreditation Council for Graduate Medical Education (ACGME). This historic merger means M.D. and D.O. graduates apply to and compete for the same residency positions, regardless of specialty.
- Scope of Practice: Both M.D.s and D.O.s are licensed to practice medicine in all 50 states and can prescribe medication, perform surgery, and work in any medical specialty.
### A Day in the Life: A Family Medicine Physician (M.D. or D.O.)
To illustrate the practical interchangeability of the roles, consider a typical day for a family medicine physician in a busy outpatient clinic. This day would look virtually identical for a D.O. or an M.D.
- 7:30 AM: Arrives at the clinic, reviews the day's patient schedule, and checks lab results and messages that came in overnight.
- 8:00 AM - 12:00 PM: Begins seeing patients. Appointments are scheduled every 15-20 minutes and cover a wide range of issues: a 6-year-old with an ear infection, a 45-year-old for a diabetes management follow-up, a 30-year-old with acute anxiety, and a 75-year-old for an annual wellness exam. The physician performs physical exams, orders tests, prescribes medications, and provides patient education.
- 12:00 PM - 1:00 PM: A quick lunch while catching up on charting, signing prescription refills, and returning urgent phone calls.
- 1:00 PM - 4:30 PM: Afternoon patient appointments continue. This might include a minor procedure like a skin tag removal, a consultation for chronic back pain, or a new patient visit.
- 4:30 PM - 6:00 PM (or later): "Desktop medicine" begins. The physician finishes patient notes in the Electronic Health Record (EHR), reviews consultant reports, follows up on imaging results, and handles prior authorization paperwork for insurance companies.
The only potential difference? The D.O. physician, when faced with the patient with chronic back pain, might incorporate OMT into their physical exam and treatment plan as an additional, non-pharmacological tool. However, both physicians would follow the same evidence-based guidelines for diagnosis and management.
Average D.O. vs. M.D. Salary: A Deep Dive
Now we arrive at the central question. While decades ago there may have been a perception-driven pay gap, today's data reveals a different story. Reputable, large-scale industry surveys consistently show that when you control for factors like specialty, location, and experience, the salary difference between M.D.s and D.O.s is statistically insignificant.
The most comprehensive data comes from Medscape's annual Physician Compensation Report. According to the Medscape 2023 Physician Compensation Report, which surveyed over 10,000 physicians:
- Average M.D. Annual Compensation: $357,000
- Average D.O. Annual Compensation: $344,000
At first glance, this shows a slight edge of $13,000 for M.D.s. However, Medscape itself clarifies the reason for this small discrepancy: it's not due to employers paying D.O.s less for the same job. Instead, it reflects historical trends in specialty choice. A higher percentage of D.O.s have traditionally chosen to enter primary care fields (like family medicine, pediatrics, and internal medicine), which are on the lower end of the physician pay scale compared to surgical and procedural specialties. As more D.O.s enter high-paying specialties—a trend that is rapidly accelerating thanks to the unified GME system—this small statistical gap is expected to disappear entirely.
The Doximity 2023 Physician Compensation Report, another industry-leading source, further reinforces this point by focusing on compensation within the same specialties, finding no significant pay gap based on the degree credential alone. Their data shows that a D.O. orthopedist and an M.D. orthopedist in the same market with similar experience will have comparable earning potential.
### Physician Salary by Experience Level
Physician salary follows a distinct and dramatic trajectory based on career stage. The journey begins with the modest salaries of residency and fellowship, followed by a significant jump to attending physician status, and then a gradual increase with experience.
While this data is not typically broken down by M.D. vs. D.O., it applies equally to both pathways. The following table, with data aggregated from sources like Salary.com and Payscale for a "Physician - General Practice" role, illustrates this typical progression.
| Career Stage | Years of Experience | Typical Annual Salary Range | Notes |
| :--- | :--- | :--- | :--- |
| Resident Physician | 0-3 (Post-Med School) | $60,000 - $80,000 | Salary is set by the hospital/institution. PGY-1 (Post-Graduate Year 1) earns the least, with small raises each year. |
| Fellow | 3-5+ | $70,000 - $90,000 | Similar to residency, but for physicians pursuing sub-specialty training after their initial residency. |
| Entry-Level Attending | 0-5 (Post-Residency) | $180,000 - $250,000 | This is the first "real" physician salary. A massive jump from training wages. |
| Mid-Career Physician | 5-15 | $240,000 - $350,000+ | Peak earning years for many. Experience, efficiency, and patient volume drive growth. |
| Senior/Experienced Physician | 15+ | $260,000 - $400,000+ | Salary may plateau but remains high. Many transition to leadership, teaching, or part-time roles. |
*(Source: Data compiled and synthesized from Salary.com, Payscale, and industry reports for a generalist physician role. Ranges for specialists will be significantly higher.)*
### Beyond the Base Salary: Understanding Total Compensation
A physician's salary is rarely a single, flat number. Total compensation is a package that includes multiple components, which are crucial for comparing job offers.
- Base Salary: The guaranteed annual pay. This can be a fixed amount or based on a work schedule (e.g., a set number of shifts per month for an emergency physician).
- Productivity Bonuses: This is a major component for many physicians. It's often based on Work Relative Value Units (wRVUs). An RVU is a measure of value used by Medicare that factors in the time, skill, and intensity required to provide a patient service. Physicians are often given a base salary and then earn a bonus for every wRVU they generate over a certain threshold. This directly rewards physicians who are more efficient or see more complex cases.
- Sign-On Bonus: A one-time payment, often ranging from $10,000 to $100,000+, offered by employers to attract physicians, especially in high-need areas or specialties.
- Retention Bonus: A bonus paid to a physician for staying with an employer for a specified period (e.g., an extra $50,000 paid out after completing year three of a contract).
- Quality Bonuses: Increasingly common in value-based care models. Physicians can earn bonuses for meeting specific quality metrics, such as patient satisfaction scores, preventative care screening rates (e.g., mammograms, colonoscopies), or chronic disease management outcomes (e.g., a certain percentage of diabetic patients with controlled A1c levels).
- Benefits Package: The value of this package can be substantial, often worth an additional $50,000 - $100,000 per year.
- Health, Dental, and Vision Insurance: For the physician and their family.
- Malpractice Insurance: Typically covered by the employer. "Tail coverage," which covers claims made after the physician leaves the practice, is a critical negotiation point.
- Retirement Plans: 401(k) or 403(b) plans, often with a generous employer match.
- Continuing Medical Education (CME): An annual allowance (e.g., $3,000 - $5,000) and paid time off to attend conferences and maintain medical licenses.
- Paid Time Off (PTO): Including vacation, holidays, and sick leave.
- Loan Repayment Assistance: Some employers, particularly in underserved areas, offer significant assistance with paying off medical school debt.
When comparing D.O. vs. M.D. opportunities, the structure of these compensation packages is identical. The negotiation will hinge on the candidate's specialty, experience, and the employer's needs, not on their degree type.
Key Factors That Influence Physician Salary
This is the most critical section for understanding physician income. The variation in pay is not random; it is driven by a predictable set of powerful factors. The D.O. vs. M.D. debate is a footnote compared to the impact of the elements below.
### `
`1. Area of Specialization: The Single Biggest Driver`
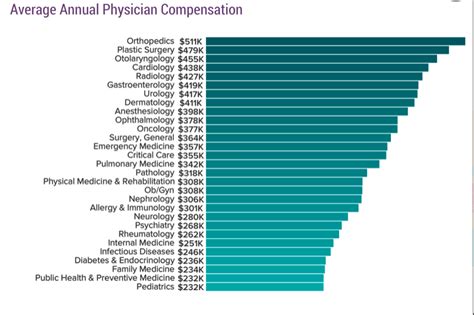
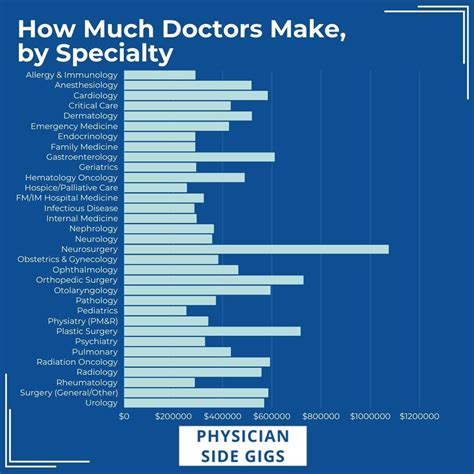
`Your choice of medical specialty will have a more profound impact on your lifetime earning potential than any other single decision. The gap between the highest- and lowest-paying specialties can be more than $500,000 per year. Procedural and surgical specialties that generate high revenue for hospitals (e.g., through surgeries, imaging, and interventions) consistently command the highest salaries.
Below is a table derived from the Medscape 2023 Physician Compensation Report, showcasing the dramatic variance in average annual compensation across different specialties. It's crucial to remember that both M.D.s and D.O.s practice and are board-certified in every one of these fields.
| Specialty | Average Annual Compensation | Notes |
| :--- | :--- | :--- |
| Highest Paying Specialties | | |
| Neurosurgery | $788,313 | The pinnacle of physician earning, requiring extensive and highly competitive training. |
| Thoracic Surgery | $706,775 | Involves surgery on the heart, lungs, esophagus, and other organs in the chest. |
| Orthopedic Surgery | $624,043 | Focuses on the musculoskeletal system; high volume of lucrative procedures (joint replacements, etc.). |
| Plastic Surgery | $571,373 | Includes both reconstructive and cosmetic procedures. |
| Cardiology (Invasive) | $544,293 | Performs procedures like angioplasty and stenting. |
| Mid-Range Specialties | | |
| Gastroenterology | $500,642 | Performs procedures like colonoscopies and endoscopies. |
| Radiology | $483,227 | Diagnostic and interventional imaging specialists. |
| Anesthesiology | $448,014 | Critical role in surgery and pain management. |
| Emergency Medicine | $385,827 | Typically shift-based work with high intensity. |
| General Surgery | $412,467 | Broad surgical practice. |
| Lower Paying Specialties (Still High Incomes) | | |
| Internal Medicine | $273,000 | Primary care for adults. |
| Family Medicine | $255,000 | Primary care for all ages. |
| Pediatrics | $244,000 | Primary care for children. |
| Public Health & Preventive Medicine | $243,000 | Focuses on population health rather than individual patient care. |
| Diabetes & Endocrinology | $257,000 | Sub-specialty of internal medicine focused on hormonal systems. |
*(Source: Medscape 2023 Physician Compensation Report. Figures represent total average compensation.)*
The key takeaway is undeniable: a D.O. who becomes an orthopedic surgeon will earn vastly more than an M.D. who becomes a pediatrician. The specialty, not the degree, dictates the salary bracket.
### `
`2. Geographic Location: Where You Practice Matters`
`Physician salaries vary significantly by state and even by metropolitan area. This variation is driven by supply and demand, cost of living, and the local healthcare market dynamics (e.g., the dominance of a few large hospital systems vs. a competitive private practice environment).
Interestingly, the highest-paying states are often not the ones with the highest cost of living, such as New York or California. Instead, they are frequently in the Midwest and Southeast, where there is a greater need to offer competitive salaries to attract physicians.
Top-Paying States for Physicians (Average Annual Compensation):
According to the Doximity 2023 report, the states where physicians earn the most are:
1. Oklahoma: $425,772
2. Georgia: $422,907
3. Iowa: $419,054
4. Missouri: $417,041
5. Alabama: $416,527
Lowest-Paying States for Physicians:
Conversely, states in the Northeast and some western states, often with a high density of physicians and academic centers, tend to have lower average compensation:
1. Maryland: $341,202
2. New Mexico: $345,730
3. District of Columbia: $346,598
4. Massachusetts: $357,690
5. Delaware: $359,005
*(Source: Doximity 2023 Physician Compensation Report)*
A physician, whether M.D. or D.O., could potentially increase their annual income by over $80,000 simply by moving from a practice in Maryland to one in Oklahoma. This geographic arbitrage is a powerful tool for maximizing income, especially early in a career when paying off student loans is a priority.
### `
`3. Practice Setting & Employment Model`
`The type of organization a physician works for also plays a major role in their compensation and work-life balance.
- Physician-Owned Private Practice: This model offers the highest earning potential. Physician-owners not only earn a clinical salary but also share in the profits of the practice. The Medscape report shows that self-employed physicians (practice owners) earn an average of $402,000 annually, compared to $339,000 for employed physicians. However, this comes with the added responsibilities and risks of running a business, including managing staff, billing, and overhead.
- Hospital or Healthcare System Employment: This is the most common model today. It offers a stable, predictable salary, excellent benefits, and freedom from administrative burdens. While the ceiling on earnings may be lower than in private practice, the floor is higher and more secure.
- Academic Medical Centers: Physicians working for universities typically earn less than their counterparts in private or hospital-based practice. The Medscape 2023 report notes academics earn about 11% less. This "pay cut" is often balanced by non-monetary benefits like teaching opportunities, research support, a more predictable schedule, and the prestige of an academic appointment.
- Government Positions: Physicians working for the VA (Veterans Health Administration), the military, or other government agencies generally have lower salaries. However, they benefit from exceptional job security, generous federal benefits and pensions, and often a better work-life balance.
- Locum Tenens: This involves working as a temporary, independent contractor to fill in for other physicians. Locum tenens work often pays a very high daily or hourly rate to compensate for the lack of benefits and job security.
### `
`4. Years of Experience & Career Trajectory`
`As detailed in the "Deep Dive" section, experience is a linear driver of salary, particularly in the first 10-15 years post-residency. An entry-level attending physician is learning to be efficient and build a patient panel. A mid-career physician has optimized their workflow, built a strong reputation, and is likely at peak productivity, especially in a wRVU-based compensation model. Senior physicians may see a slight plateau or decline in income if they choose to scale back their clinical hours, but their base of experience still commands a high salary.
### `
`5. In-Demand Skills & Procedural Abilities`
`Within any given specialty, physicians who are trained in the latest, most in-demand procedures can command a premium salary. These are not just "skills" but often require fellowship training or specialized certification. Examples include:
- Surgical Robotics: Surgeons (urologists, general surgeons, gynecologists) proficient with systems like the da Vinci robot are highly sought after by hospitals that have invested millions in this technology.
- Interventional Procedures: Cardiologists who can perform TAVR (transcatheter aortic valve replacement) or interventional radiologists who perform complex embolizations are top earners.
- Advanced Imaging: Radiologists with fellowship training in neuroradiology or musculoskeletal MRI can interpret more complex and higher-reimbursing studies.
- Bilingualism: In many parts of the country, physicians who are fluent in Spanish or other languages are highly valuable and may be offered a stipend or higher starting salary.
- Leadership and Administrative Skills: Physicians who take on administrative roles like Medical Director, Department Chair, or Chief Medical Officer receive an additional stipend or a significantly higher salary for their leadership responsibilities.
Job Outlook and Career Growth for Physicians
The demand for physicians and surgeons in the United States is projected to remain strong, driven by several key demographic and healthcare trends.
According to the U.S. Bureau of Labor Statistics (BLS) Occupational Outlook Handbook, employment for physicians and surgeons is projected to grow 3 percent from 2022 to 2032. While this percentage is about as fast as the average for all occupations, it's essential to understand the context. This growth translates to an average of about 24,100 openings for physicians and surgeons each year over the decade. These openings will arise not only from new job creation but also from the need to replace physicians who are retiring or leaving the profession.
Key Drivers of Physician Demand:
- An Aging Population: The large baby-boomer generation is aging, and older adults typically require more medical care, from primary care management of chronic conditions to specialized surgical interventions.
- **Physician Retirements