Table of Contents

- [Introduction](#introduction)
- [What Does a Dermatologist Do? A Look Beyond the Surface](#what-does-a-dermatologist-do)
- [Average Dermatologist Salary: A Deep Dive into Your Earning Potential](#average-dermatologist-salary)
- [Key Factors That Influence a Dermatologist's Salary](#key-factors-that-influence-salary)
- [Dermatologist Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Become a Dermatologist: Your Step-by-Step Roadmap](#how-to-become-a-dermatologist)
- [Conclusion: Is a Career in Dermatology Right for You?](#conclusion)
Introduction

For those with a passion for science, a desire for meaningful patient interaction, and an eye for detail, a career in dermatology presents one of the most compelling opportunities in all of medicine. It's a field that beautifully melds the diagnostic rigor of internal medicine, the procedural skill of surgery, and the aesthetic artistry of cosmetic enhancement. But beyond the intellectual and personal fulfillment, let's be direct: dermatology is also renowned for its exceptional financial rewards and favorable work-life balance. If you're standing at the beginning of your medical journey, dreaming of a specialty that is both challenging and highly lucrative, understanding the financial landscape is a critical first step.
So, what can you realistically expect to earn? While the journey is long, the rewards are substantial. The average starting salary for a dermatologist fresh out of residency typically falls in the impressive range of $250,000 to $350,000 per year. However, this is merely the launchpad. With experience, strategic career choices, and potential for practice ownership, total compensation can soar well past $500,000 annually.
I recall a conversation with a family friend, a newly minted dermatologist who had just accepted her first position. She spoke not just of the relief of finally earning a substantial income after over a decade of training and debt accumulation, but of the profound sense of agency it gave her. She could aggressively pay down her student loans, invest in her future, and, most importantly, focus entirely on providing the best possible care for her patients without the immediate financial anxieties that plague so many new physicians. Her story underscores the powerful combination of professional satisfaction and financial security that makes dermatology such a sought-after specialty.
This guide is designed to be your definitive resource for understanding a dermatologist's salary and career trajectory. We will dissect compensation data from authoritative sources, explore the crucial factors that dictate your earning potential, and lay out a clear, actionable roadmap to achieving your career goals. Whether you are a high school student fascinated by biology or a medical student weighing your specialty options, this article will provide the clarity and data you need to make an informed decision.
What Does a Dermatologist Do? A Look Beyond the Surface

A dermatologist is a medical doctor (MD or DO) who specializes in diagnosing and treating conditions related to the skin, hair, nails, and mucous membranes. The skin is the body's largest organ, and its health is a window into a person's overall well-being. Consequently, the scope of a dermatologist's work is incredibly broad and varied, extending far beyond the common public perception of treating acne and warts.
The field is broadly divided into three main pillars:
1. Medical Dermatology: This is the diagnostic core of the specialty. Dermatologists identify and manage over 3,000 different conditions. These include chronic inflammatory diseases like eczema (atopic dermatitis) and psoriasis, infectious diseases like fungal infections and cellulitis, autoimmune disorders such as lupus and dermatomyositis, and the critical early detection and management of skin cancers like melanoma, basal cell carcinoma, and squamous cell carcinoma.
2. Surgical Dermatology: Many dermatologists are also skilled surgeons. This involves performing procedures to remove both benign growths (cysts, moles) and malignant tumors. The most specialized form of this is Mohs micrographic surgery, a precise technique used to remove skin cancers layer by layer, offering the highest cure rate while sparing healthy tissue. Other common surgical procedures include biopsies, excisions, cryosurgery (freezing with liquid nitrogen), and laser surgery.
3. Cosmetic Dermatology: This rapidly growing area focuses on improving the patient's aesthetic appearance. These are typically elective, cash-based procedures that are not covered by insurance. They include administering botulinum toxin (Botox) to reduce wrinkles, injecting dermal fillers to restore volume, performing chemical peels, laser hair removal, and treatments for scarring and sun damage.
### A Day in the Life of a General Dermatologist
To make this more tangible, let's walk through a typical day for a dermatologist in a private group practice.
- 8:00 AM - 8:30 AM: Arrive at the office. Review the day's patient schedule with the medical assistant, flagging complex cases or procedures. Look over pathology reports that have come in overnight from biopsies performed earlier in the week.
- 8:30 AM - 12:00 PM: Morning patient block. The pace is often quick, with appointments scheduled every 15-20 minutes.
- 8:30 AM: A teenager for an acne follow-up, adjusting their prescription and discussing skincare routines.
- 8:45 AM: An elderly patient for a full-body skin exam, identifying and performing cryosurgery on several pre-cancerous spots (actinic keratoses).
- 9:15 AM: A new patient with a suspicious mole. After examination with a dermatoscope, a shave biopsy is performed to send for analysis.
- 9:45 AM: A patient with severe psoriasis to discuss starting a biologic medication, including potential side effects and the insurance approval process.
- 10:30 AM: A 30-minute slot for a surgical excision of a confirmed basal cell carcinoma on a patient's back.
- 11:00 AM - 12:00 PM: A mix of rash evaluations, wart treatments, and follow-up appointments.
- 12:00 PM - 1:00 PM: Lunch break, which is often spent catching up on charting in the Electronic Health Record (EHR), signing off on prescription refills, and making phone calls to patients with their biopsy results.
- 1:00 PM - 4:30 PM: Afternoon patient block. This might be designated as a "cosmetic" or "procedure" afternoon.
- 1:00 PM: A consultation for a patient interested in Botox and fillers.
- 1:30 PM: A patient receiving Botox injections for forehead lines.
- 2:00 PM: A patient for a laser treatment to reduce facial redness from rosacea.
- 2:45 PM: A follow-up visit for a patient who had a chemical peel two weeks prior.
- 3:15 PM: An excision of a benign but bothersome cyst on a patient's scalp.
- 4:30 PM - 5:30 PM: Administrative wrap-up. Finalizing all patient notes for the day, reviewing and signing off on charts prepared by medical assistants, responding to emails, and handling any urgent patient queries.
This schedule highlights the immense variety in a dermatologist's day—a blend of detective work, patient education, precise procedural skills, and long-term relationship building.
Average Dermatologist Salary: A Deep Dive into Your Earning Potential
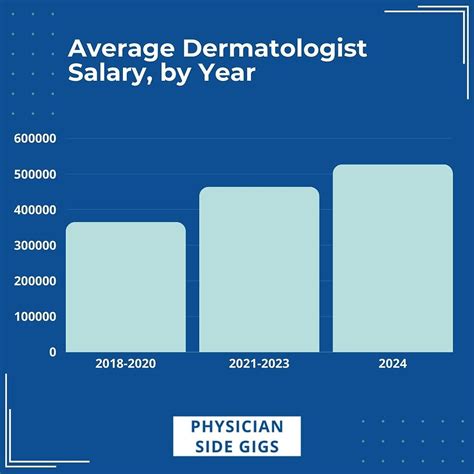
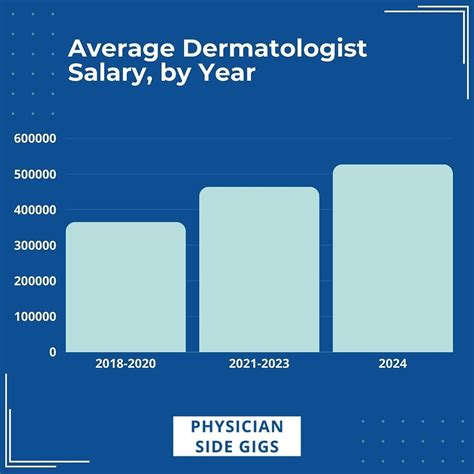
The financial prospects for dermatologists are among the best in the medical field. The high demand for their services, combined with a limited supply of specialists, creates a favorable market for compensation. It's important to analyze data from multiple reputable sources to get a well-rounded picture.
According to the Medscape Dermatologist Compensation Report 2023, one of the most respected industry benchmarks, the average annual income for a dermatologist is $443,000. This figure represents an aggregate of dermatologists at all career stages, practice types, and locations.
Let's break down what this means for you at different points in your career.
### Dermatologist Salary by Experience Level
Salary progression in dermatology is significant. Your income grows as you build your patient base, become more efficient, and potentially take on partnership or ownership roles.
| Career Stage | Years of Experience | Typical Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Starting / Entry-Level | 0-3 Years | $250,000 - $375,000 | Post-residency. Often on a guaranteed salary or a lower production-based model. Focused on building a patient roster. |
| Mid-Career | 4-10 Years | $380,000 - $550,000 | Established patient panel, high efficiency. Often transitioning to a full productivity-based compensation model. Potential for partnership. |
| Senior / Experienced | 10+ Years | $450,000 - $700,000+ | Peak earning years. Often a partner or owner of a successful practice. Strong reputation in the community. |
*Sources: Data compiled and synthesized from Medscape Physician Compensation Report 2023, Doximity Physician Compensation Report 2023, and Salary.com.*
- A Note on Starting Salaries: Your very first contract out of residency is crucial. Many practices offer a guaranteed base salary for the first one to two years. This provides security while you build your practice. For example, a common offer might be a $300,000 guarantee for two years, or a base of $275,000 plus a percentage of collections, whichever is higher. After this initial period, compensation almost always shifts to a productivity-based model.
### Understanding Your Compensation Package
A dermatologist's income is rarely just a flat salary. The total compensation package is a mosaic of different components, especially in private practice.
- Base Salary: The fixed, guaranteed amount you earn, common in academic and hospital-employed positions, and as an initial offer in private practice.
- Productivity-Based Pay (Collections Model): This is the most common model in private practice. You receive a percentage of the revenue you generate for the practice. A typical arrangement is receiving 35% to 50% of your net collections. For example, if you generate $1 million in revenue for the practice in a year, at a 40% collection rate, your gross income would be $400,000. This model directly incentivizes efficiency and hard work.
- Relative Value Units (RVUs): Some hospital systems use RVUs to measure physician productivity. Every patient encounter and procedure is assigned a certain RVU value. Your compensation is then tied to the total number of RVUs you generate.
- Bonuses: These can be tied to productivity (exceeding a certain collection threshold), quality metrics, patient satisfaction scores, or year-end practice profitability. Signing bonuses, ranging from $10,000 to $50,000 or more, are also common for attracting talent to a new position, especially in less saturated areas.
- Profit Sharing / Partnership Income: For those who become partners in a private practice, a significant portion of their income comes from a share of the practice's overall profits. This represents the highest earning potential but also comes with the responsibilities of business ownership.
- Ancillary Benefits: The value of your benefits package should not be underestimated. This often includes:
- Health, Dental, and Vision Insurance: Comprehensive plans for you and your family.
- Malpractice Insurance: Absolutely essential. Most employers cover the full cost of "claims-made" or "occurrence" policies.
- Retirement Plans: Access to 401(k) or 403(b) plans, often with a generous employer match.
- Continuing Medical Education (CME) Allowance: An annual stipend (e.g., $2,500 - $5,000) to cover costs for conferences and educational materials required to maintain your medical license.
- Paid Time Off (PTO): Typically 4-6 weeks per year for vacation and sick leave.
- Relocation Assistance: A one-time payment to help with the costs of moving for a new job.
When evaluating a job offer, it's critical to look at the total compensation, not just the base salary. A lower base salary with a strong productivity bonus structure and excellent benefits can often be more lucrative in the long run than a high-guaranteed salary with no upside.
Key Factors That Influence a Dermatologist's Salary

Your starting salary and long-term earning potential are not set in stone. They are influenced by a complex interplay of personal choices, market forces, and geographic realities. Understanding these factors will empower you to make strategic decisions that maximize your income throughout your career.
### ### Level of Education & Advanced Training (Fellowships)
While all dermatologists complete a rigorous educational path, pursuing an additional fellowship after residency is the single most powerful educational step you can take to amplify your salary. A fellowship is 1-2 years of intensive, sub-specialized training.
- Mohs Micrographic Surgery: This is the undisputed king of compensation in dermatology. Mohs surgeons specialize in a highly precise method for removing skin cancers, primarily on the face and other cosmetically sensitive areas. Because the procedure is complex, time-consuming, and highly reimbursed by insurance, Mohs surgeons are in exceptionally high demand. A dermatologist with a Mohs fellowship can expect to earn $150,000 to $300,000+ more per year than a general dermatologist. Starting salaries for Mohs surgeons often begin in the $450,000 to $600,000 range.
- Dermatopathology: This fellowship involves training to diagnose skin diseases at a microscopic level. Dermatopathologists spend most of their time in a lab reading slides from biopsies. While they have less direct patient contact, their expertise is crucial. Their income is high and stable, often comparable to or slightly higher than general medical dermatologists.
- Pediatric Dermatology: This fellowship focuses on the unique skin conditions affecting infants, children, and adolescents. While financially rewarding, the salary premium is generally less pronounced than for Mohs surgery. The motivation here is often a passion for working with a younger patient population.
- Cosmetic Dermatology Fellowship: While some cosmetic training is included in residency, a dedicated fellowship provides advanced skills in lasers, injectables, and other aesthetic procedures. This can dramatically increase earning potential, as these services are cash-based and highly profitable.
Takeaway: If maximizing income is a primary goal, completing a fellowship in Mohs surgery is the most direct path.
### ### Years of Experience & Practice Maturity
As detailed in the previous section, experience is a primary driver of salary growth. This isn't just about age; it's about the maturation of your practice.
- Years 1-2 (Ramp-up Phase): Your schedule may have open slots as you build a referral network and patient roster. You are learning the specific workflows of your new practice. A guaranteed salary is common during this phase to provide stability.
- Years 3-10 (Peak Productivity Phase): Your schedule is full, often booked out for months. You can perform procedures more efficiently, manage complex cases with confidence, and have a loyal patient following. This is when a productivity-based model becomes highly lucrative. Many dermatologists become partners in their practice during this period.
- Years 10+ (Ownership/Leadership Phase): Your clinical income may plateau, but your total compensation can continue to grow through practice ownership. As a practice owner, you earn not only from your own clinical work but also from the profits generated by other physicians, physician assistants, aestheticians, and ancillary services (like an in-house pathology lab or cosmetic product sales). According to the Medscape Physician Wealth & Debt Report 2023, physicians who are self-employed (i.e., practice owners/partners) report significantly higher net worth than their employed counterparts.
### ### Geographic Location
Where you choose to practice has a massive impact on your salary, often in counterintuitive ways. High demand in less-populated or less "desirable" areas often drives salaries up to attract talent.
According to the Doximity 2023 Physician Compensation Report, here is a look at how geography can influence pay:
Top 5 Highest Paying Metropolitan Areas for Physicians (Illustrative for Specialists):
1. Charlotte, NC
2. St. Louis, MO
3. Oklahoma City, OK
4. San Jose, CA
5. Minneapolis, MN
Top 5 Highest Paying States for Physicians (Illustrative for Specialists):
1. Oklahoma
2. Georgia
3. Utah
4. Missouri
5. Alabama
Conversely, areas with a high density of dermatologists and a desirable lifestyle, like major cities in the Northeast (New York City, Boston) or Southern California (Los Angeles), can be more competitive. While the nominal salaries are still high, they may not be as elevated when adjusted for the staggering cost of living. A $400,000 salary in rural Wisconsin may afford a much higher quality of life than a $450,000 salary in San Francisco.
Rural vs. Urban: Practices in rural or underserved areas often offer significant financial incentives to attract dermatologists. These can include:
- Higher starting salaries and/or a higher percentage of collections.
- Substantial signing bonuses.
- Student loan repayment assistance programs (sometimes up to $100,000 or more).
- A faster track to partnership.
Takeaway: Don't just look at the big coastal cities. Your highest earning potential, especially early in your career, may be in the Midwest or Southeast.
### ### Practice Type & Ownership Model
The setting in which you work is a critical determinant of both your income and your day-to-day professional life.
- Private Practice (Group): This is the most common and often the most lucrative model for dermatologists. You start as an employee and work towards becoming a partner. The practice handles the administrative burdens (billing, staffing, IT), and you focus on seeing patients. Income is typically production-based.
- Private Practice (Solo): The entrepreneurial path. You are the owner from day one. This offers the highest potential reward, as you keep 100% of the profits after expenses. However, it also carries the highest risk and the full weight of running a business, including marketing, HR, and financial management.
- Hospital or Health System-Employed: You are an employee of the hospital. This model offers stability, a predictable salary, excellent benefits, and minimal administrative hassle. However, the earning potential is generally lower than in private practice, as there is no path to ownership and productivity bonuses may be capped. This can be an excellent choice for those prioritizing work-life balance and stability.
- Academic Medicine: You work at a university medical center. The mission is threefold: clinical care, teaching residents and medical students, and research. Salaries in academia are consistently the lowest across all specialties. According to Medscape, the average academic physician earns about 15-25% less than their private practice counterpart. The compensation comes in non-monetary forms: intellectual stimulation, prestige, and the opportunity to work on cutting-edge cases and research.
- Government/VA: Working for the Department of Veterans Affairs (VA) or the military offers excellent benefits, job security, and a pension, but with lower salaries compared to the private sector.
### ### Area of Specialization & Procedural Mix
Within your practice, the types of services you offer will shape your income.
- Medical/General Dermatology: This forms the foundation of most practices. While essential, it is generally less profitable on a per-visit basis than procedural work.
- Cosmetic Dermatology: This is a major profit center. Procedures like Botox, fillers, and certain laser treatments have high margins and are paid for directly by the patient, avoiding the hassles and lower reimbursement rates of insurance companies. A practice with a strong cosmetic component will almost always have higher revenue.
- Surgical Dermatology: Procedures, particularly excisions and Mohs surgery, are reimbursed at a much higher rate than standard office visits. A dermatologist who is surgically-oriented will generate more revenue than one who primarily manages chronic conditions.
- Ancillary Services: Successful practices often add other revenue streams. These can include:
- In-house Dermatopathology: If the practice is large enough, having its own pathologist to read its biopsies can be a significant source of revenue.
- Selling Skincare Products: Curating and selling a line of medical-grade skincare products (sunscreen, retinoids, etc.) can add a surprisingly large and high-margin revenue stream.
- Aesthetician Services: Employing licensed aestheticians to perform services like facials, microdermabrasion, and light chemical peels.
### ### In-Demand Skills & Business Acumen
Beyond your clinical diploma, certain soft and hard skills can significantly enhance your value and income.
- Efficiency and Time Management: In a production-based model, time is money. The ability to see patients efficiently without compromising quality of care is a learned skill that directly translates to higher income.
- Excellent "Bedside Manner": Patients who feel heard, respected, and well-cared-for are more likely to return, adhere to treatment, and refer friends and family. This builds your practice and your reputation.
- Business & Financial Literacy: For those in or aspiring to private practice, this is non-negotiable. Understanding profit and loss statements, negotiating with vendors, managing staff, and marketing your services are skills that determine the success or failure of a practice.
- Leadership & Mentoring: The ability to lead a team, mentor physician assistants (PAs) and nurse practitioners (NPs), and contribute to a positive work culture makes you a more valuable partner or senior physician.
Dermatologist Job Outlook and Career Growth

The future for dermatologists is exceptionally bright. The demand for their expertise is robust and projected to grow steadily for the foreseeable future, ensuring strong job security and continued high earning potential.
### ### Job Growth Projections
The U.S. Bureau of Labor Statistics (BLS) groups dermatologists under the broader category of "Physicians and Surgeons." In its Occupational Outlook Handbook, the BLS projects that employment for this group will grow by 3% from 2022 to 2032. While this may seem modest, it's important to understand the context for dermatology specifically. The demand for dermatologists far outstrips this general physician growth rate due to several key factors:
1. An Aging Population: The massive Baby Boomer generation is entering its senior years. Older individuals have a significantly higher incidence of skin cancers (basal cell, squamous cell, melanoma) and other age-related skin conditions, driving demand for both screening and treatment.
2. Increased Public Awareness: Public health campaigns have successfully increased awareness of the dangers of sun exposure and the importance of early skin cancer detection. This leads to more people seeking preventative full-body skin exams.
3. The Rise of Cosmetic Dermatology: There is a powerful and growing societal trend towards aesthetic and anti-aging treatments. The demand for minimally invasive procedures like Botox, fillers, and laser therapies is booming and shows no signs of slowing down. This provides a massive, cash-based market for dermatological services.
4. Limited Supply of Dermatologists: Dermatology residency positions are among the most competitive in all of medicine. The number of new dermatologists trained each year is strictly limited, creating a perpetual shortage. It is common for patients in many parts of the country to wait three to six months or even longer for a routine appointment, a clear indicator of overwhelming demand.
This supply-demand imbalance is the fundamental economic reason why dermatologists command high salaries and have their choice of practice opportunities upon finishing residency.
### ### Emerging Trends and Future Challenges
The field is not static. To thrive, dermatologists must adapt to new technologies and navigate evolving healthcare landscapes.
Emerging Trends: