Table of Contents

- [Introduction](#introduction)
- [What Does a Certified Nurse-Midwife (CNM) Do?](#what-does-a-cnm-do)
- [Average CNM Nurse Salary: A Deep Dive](#average-cnm-salary-a-deep-dive)
- [Key Factors That Influence CNM Nurse Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth for CNMs](#job-outlook-and-career-growth)
- [How to Become a Certified Nurse-Midwife](#how-to-get-started-in-this-career)
- [Conclusion: Is a Career as a CNM Right for You?](#conclusion)
---
Introduction

For those drawn to the profound intersection of science, compassion, and the miracle of life, a career as a Certified Nurse-Midwife (CNM) is more than a job—it is a calling. It's a profession that empowers women, champions patient-centered care, and places you at the very forefront of some of life's most intimate and powerful moments. Beyond the immense personal satisfaction, this advanced practice nursing role also offers significant financial rewards and a robust career outlook, making it one of the most compelling paths in modern healthcare. Aspiring CNMs often begin their journey with a crucial question: What is the real earning potential? The average CNM nurse salary reflects the high level of skill, responsibility, and education required, with most professionals earning well over six figures.
The national median salary for nurse-midwives falls within the impressive $125,000 to $130,000 range, with top earners in high-demand areas exceeding $170,000 annually. This positions the career as not only emotionally fulfilling but also financially stable and lucrative. I once had the privilege of observing a CNM guide a family through a long and challenging labor. Her blend of calm authority, evidence-based clinical expertise, and genuine, unwavering emotional support transformed a potentially frightening experience into one of empowerment and joy. It was a masterclass in what modern, holistic healthcare should look like, and it solidified my understanding of the immense value these professionals bring to our healthcare system.
This guide is designed to be your definitive resource on the CNM nurse salary and the career path as a whole. We will dissect national salary data, explore the critical factors that can increase your earning potential, analyze the future job market, and provide a clear, step-by-step roadmap for how to embark on this incredible journey. Whether you are a nursing student, a practicing RN considering a new specialty, or simply curious about this dynamic field, this article will provide the authoritative, in-depth information you need to make an informed decision about your future.
---
What Does a Certified Nurse-Midwife (CNM) Do?
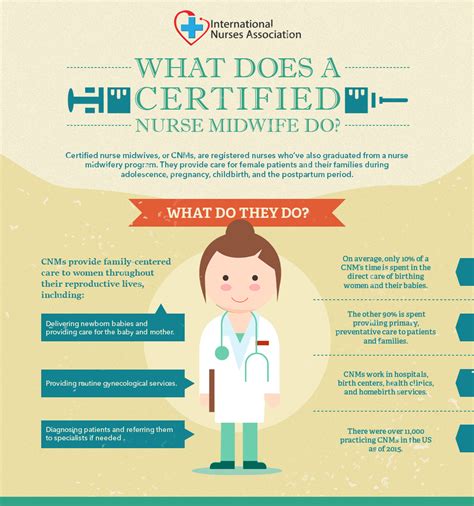
The title "Nurse-Midwife" often conjures an image of a professional solely focused on pregnancy and childbirth. While this is a central and defining aspect of the role, the true scope of a CNM's practice is far broader and more comprehensive. Certified Nurse-Midwives are advanced practice registered nurses (APRNs) who provide a full spectrum of primary, gynecological, and reproductive healthcare to women from adolescence through menopause and beyond.
At their core, CNMs are champions of the midwifery model of care. This philosophy emphasizes partnership with the patient, a deep respect for the normal, physiological processes of a woman's life cycle, and a focus on minimizing unnecessary medical interventions while maintaining a vigilant watch for complications. They are rigorously trained in both nursing and midwifery, blending scientific evidence with a holistic, personalized approach.
Core Responsibilities and Daily Tasks:
A CNM's duties extend far beyond the labor and delivery room. Their practice encompasses:
- Primary Care: Performing annual physical exams, health screenings, and wellness counseling.
- Gynecological Care: Managing common gynecological issues, performing Pap tests, and treating infections.
- Family Planning and Contraception: Providing counseling on and prescribing all forms of contraception.
- Preconception Care: Helping women prepare for a healthy pregnancy.
- Antenatal (Prenatal) Care: Monitoring the health of both mother and baby throughout pregnancy through regular check-ups, ordering and interpreting diagnostic tests, and providing education.
- Intrapartum Care (Labor and Birth): Managing labor, delivering babies, and monitoring the mother's and baby's well-being. They are experts in low-intervention births but are also trained to identify and manage obstetric emergencies, often working collaboratively with physicians.
- Postpartum Care: Supporting mothers in the weeks and months following birth, including managing physical recovery, providing lactation support, and screening for postpartum depression.
- Care of the Newborn: Providing initial care and assessment for healthy newborns during the first 28 days of life.
- Menopausal Care: Providing counseling and treatment for symptoms related to perimenopause and menopause.
A Day in the Life of a CNM:
The daily life of a CNM can vary dramatically depending on their work setting. To illustrate, consider two common scenarios:
- A Clinic Day: The day begins at 8:00 AM with a review of the day's patient schedule. The morning is filled with a mix of appointments: a 16-year-old seeking her first contraceptive prescription, a 28-week prenatal check-up, a 45-year-old for her annual exam, and a 6-week postpartum follow-up. Between patients, the CNM returns calls, refills prescriptions through the electronic health record (EHR), and consults with a collaborating physician about a patient with newly elevated blood pressure. The afternoon follows a similar pattern, ending with an hour of charting to ensure all patient records are accurate and complete.
- A Hospital On-Call Day: The CNM might be on a 12- or 24-hour shift at a hospital. The day is unpredictable. It could start with "rounding" on postpartum patients, checking their recovery and assisting with breastfeeding. Suddenly, a call comes from the labor and delivery unit: one of their patients has arrived in active labor. The CNM spends the next several hours providing continuous labor support, monitoring fetal heart tones, and managing the patient's progress. After a successful delivery, they complete the initial newborn exam and stitch a minor tear. Just as they sit down to chart, another patient calls to say her water has broken. This dynamic environment requires immense stamina, critical thinking, and the ability to switch contexts rapidly from routine care to high-stakes decision-making.
In both settings, the CNM acts as a primary healthcare provider, educator, advocate, and trusted partner, embodying a unique and vital role in women's health.
---
Average CNM Nurse Salary: A Deep Dive
A career as a Certified Nurse-Midwife is not only professionally rewarding but also financially lucrative, reflecting the advanced education, clinical autonomy, and immense responsibility the role entails. Understanding the compensation landscape is a critical step for anyone considering this demanding yet fulfilling profession.
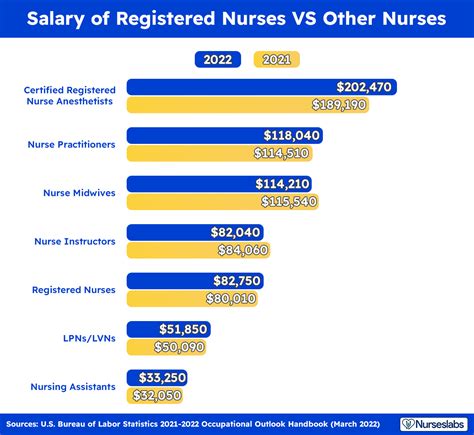
According to the U.S. Bureau of Labor Statistics (BLS), nurse-midwives are grouped with nurse anesthetists and nurse practitioners in their salary data. For this combined group of APRNs, the median annual wage was $128,470 as of May 2023. The lowest 10 percent earned less than $87,340, while the highest 10 percent earned more than $209,920. While this figure provides a strong benchmark, data specific to CNMs from professional organizations and salary aggregators offers a more granular view.
The American College of Nurse-Midwives (ACNM), the leading professional organization for the field, regularly conducts compensation surveys. Their data consistently shows a strong six-figure income for full-time practitioners. Similarly, reputable salary aggregators provide a detailed picture:
- Salary.com reports that the median annual salary for a Certified Nurse-Midwife in the United States is $125,567 as of late 2023. The typical salary range falls between $115,556 and $144,385.
- Payscale.com indicates a slightly lower average base salary of around $110,000, but this often excludes bonuses and other compensation, which can significantly increase total earnings.
- Glassdoor.com, which aggregates self-reported salaries, shows a total pay average for CNMs at approximately $134,858 per year, with a likely range between $117,000 and $156,000.
These figures confirm that a CNM is a high-earning profession, competitive with other advanced healthcare roles. The variation between sources highlights the importance of considering a range of factors, which we will explore in the next section.
### Salary Progression by Experience Level
Like most professions, compensation for a CNM grows significantly with experience. As a midwife gains clinical confidence, develops specialized skills, and takes on more complex responsibilities, their value to an employer increases.
Here is a typical salary progression based on national data from sources like Salary.com and Payscale:
| Experience Level | Years of Experience | Typical Annual Salary Range | Key Responsibilities & Skills |
| ----------------------- | ------------------- | --------------------------- | -------------------------------------------------------------------------------------------------------------- |
| Entry-Level CNM | 0-2 Years | $95,000 - $115,000 | Performing routine prenatal/postpartum care, attending low-risk births, basic gynecological services under mentorship. |
| Mid-Career CNM | 3-9 Years | $115,000 - $135,000 | Handling more complex cases, increased autonomy, mentoring new midwives, participating in practice committees. |
| Experienced/Senior CNM | 10-19 Years | $130,000 - $155,000+ | Managing high-risk patients (in collaboration), taking on leadership roles (e.g., Director of Midwifery). |
| Late-Career CNM | 20+ Years | $140,000 - $170,000+ | Often in senior leadership, practice ownership, academia, or policy-making roles. Deep clinical expertise. |
*Note: These are national averages and can be significantly higher in certain geographic locations and work settings.*
### Beyond the Base Salary: A Look at Total Compensation
The annual salary is just one piece of the financial puzzle. A comprehensive compensation package for a CNM often includes a variety of valuable benefits and incentives that substantially increase their overall earnings and job satisfaction. When evaluating a job offer, it is crucial to look beyond the base pay.
Common Components of a CNM Compensation Package:
- Base Salary: The guaranteed annual pay for the role.
- On-Call Pay: Many CNM positions, especially in hospital settings or private practices, require being on-call for births. This is often compensated with an hourly rate for being available and a different, higher rate or call-back pay for time spent managing a patient or attending a birth.
- Bonuses: These can come in several forms:
- Sign-On Bonus: A one-time payment to attract a candidate to a new position, particularly in high-demand areas. These can range from $5,000 to $20,000 or more.
- Performance Bonus: An annual or quarterly bonus tied to specific metrics, such as patient volume, patient satisfaction scores, or quality-of-care outcomes.
- Retention Bonus: Offered to tenured midwives to encourage them to stay with the practice or hospital system.
- Profit Sharing: In private midwifery practices, experienced CNMs or partners may receive a share of the practice's annual profits.
- Overtime Pay: For hourly CNMs, working beyond a standard 40-hour week results in time-and-a-half pay, which can add up quickly during busy periods.
- Health and Wellness Benefits: Comprehensive medical, dental, and vision insurance for the CNM and their family.
- Retirement Plans: Access to 401(k) or 403(b) retirement savings plans, often with a generous employer match (e.g., 3-6% of salary).
- Professional Liability (Malpractice) Insurance: This is an absolute necessity. Most employers cover the full cost of this expensive but crucial insurance.
- Continuing Education (CE) Stipend: Employers typically provide an annual allowance (e.g., $1,500 - $3,000) and paid time off to attend conferences and complete the continuing education units required to maintain certification and licensure.
- Licensure and Certification Fee Reimbursement: Coverage for the costs of renewing state licenses and national AMCB certification.
- Paid Time Off (PTO): A generous allotment of vacation, sick, and personal days is standard.
When all these elements are combined, the total compensation for a CNM can be 15-25% higher than their base salary alone, making it a truly comprehensive and competitive financial package.
---
Key Factors That Influence CNM Nurse Salary

While the national averages provide a solid baseline, a Certified Nurse-Midwife's actual salary is a dynamic figure influenced by a complex interplay of factors. Understanding these variables is key to maximizing your earning potential throughout your career. This section provides an extensive breakdown of the elements that have the most significant impact on a CNM nurse salary.
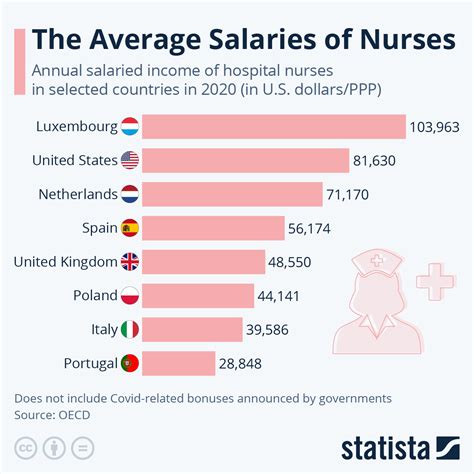
### 1. Geographic Location
Where you practice is arguably the single most powerful determinant of your salary. The demand for CNMs, cost of living, and, most importantly, state-level regulations create vast disparities in compensation across the country.
- State Scope of Practice Laws: This is the most critical sub-factor. States are generally categorized into three tiers regarding APRN practice authority:
- Full Practice Authority (FPA): In these states (e.g., Oregon, Washington, New Mexico, Maryland), CNMs can practice to the full extent of their training and education without mandatory physician supervision. This autonomy makes them highly valuable and cost-effective providers, often leading to higher salaries and more opportunities for private practice.
- Reduced Practice: These states require a career-long collaborative agreement with a physician for at least one element of practice.
- Restricted Practice: These states (e.g., California, Texas, Florida) require career-long supervision, delegation, or team management by a physician. This can limit a CNM's autonomy and suppress wages, as they are seen as an extension of a physician's practice rather than independent providers.
- Metropolitan vs. Rural Areas: Large, high-cost-of-living metropolitan areas (e.g., New York City, San Francisco, Los Angeles) naturally offer higher nominal salaries to offset expenses. However, some of the highest *real* wages (adjusted for cost of living) can be found in rural or underserved areas where hospitals and clinics use significant financial incentives, including loan repayment programs, to attract qualified providers.
Top-Paying States and Metropolitan Areas for Nurse-Midwives:
Data from the BLS (May 2023 for the APRN group) and other salary sources consistently highlight the following areas as high-paying:
| State / Metro Area | Estimated Average Annual Salary | Key Driving Factors |
| ------------------ | ------------------------------- | ------------------------------------------------------------------------------------------------ |
| California | $165,000 - $180,000+ | High cost of living, strong union presence (Kaiser Permanente), high demand in major metro areas. |
| New York | $150,000 - $170,000+ | Very high cost of living, large academic medical centers, high demand in NYC and suburbs. |
| Oregon | $145,000 - $160,000+ | Full Practice Authority, high integration of midwives into the healthcare system, progressive culture. |
| Washington | $140,000 - $155,000+ | Full Practice Authority, strong demand, competitive hospital systems in the Seattle area. |
| Massachusetts | $140,000 - $155,000+ | High cost of living, world-renowned academic medical centers, competitive healthcare market. |
Conversely, states in the Southeast and parts of the Midwest with lower costs of living and more restrictive practice laws tend to offer lower average salaries, often in the $95,000 to $115,000 range. However, a $110,000 salary in Alabama may offer a higher quality of life than a $140,000 salary in San Jose, California, due to the vast difference in living expenses.
### 2. Work Setting and Employer Type
The type of facility where a CNM works has a profound impact on their daily responsibilities, patient population, and compensation structure.
- Hospitals (Academic vs. Community): Hospitals are the largest employers of CNMs. Large, university-affiliated academic medical centers often offer competitive salaries and excellent benefits but may come with higher patient loads and more bureaucratic structures. Community hospitals may offer slightly lower base salaries but can provide a better work-life balance and a strong sense of community. Hospital-employed CNMs typically receive a stable salary with comprehensive benefits packages.
- Private Physician/Midwifery Practices: Working in a private practice can be highly rewarding. As an employee, the salary may be comparable to a hospital, but there might be more opportunities for performance-based bonuses tied to the practice's success. For CNMs who become partners or owners of a practice, the earning potential is theoretically unlimited but also comes with the risks and responsibilities of running a small business.
- Freestanding Birth Centers: These centers offer a unique, low-intervention environment. Salaries may be slightly lower than in large hospital systems, as they often operate on tighter margins and serve a clientele that may include a higher percentage of self-pay or Medicaid patients. However, the work environment is a major draw for midwives passionate about the midwifery model of care.
- Public Health Clinics and Federally Qualified Health Centers (FQHCs): These non-profit organizations serve vulnerable and underserved populations. While base salaries are often lower than in the private sector, the compensation packages can be excellent. They frequently include generous benefits, regular hours (fewer on-call demands), and, most importantly, eligibility for federal loan forgiveness programs like the National Health Service Corps (NHSC) Loan Repayment Program, which can be worth tens of thousands of dollars.
- Government and Military: CNMs working for the Department of Veterans Affairs (VA), the Indian Health Service (IHS), or as commissioned officers in the U.S. military receive salaries based on government pay scales (like the GS scale) or military rank. These roles offer exceptional job security, federal benefits, and unique practice opportunities.
### 3. Level of Education
The minimum educational requirement to become a CNM is a Master of Science in Nursing (MSN). However, the terminal degree for practice-focused nursing is increasingly becoming the Doctor of Nursing Practice (DNP).
- MSN vs. DNP: A CNM with a DNP may not see a dramatically higher starting salary for a purely clinical role compared to an MSN-prepared peer. However, the DNP opens doors to higher-paying positions in leadership, administration, policy, and academia. A DNP-prepared CNM who becomes the Director of Midwifery Services for a hospital system will earn significantly more than a staff CNM. The DNP curriculum's focus on systems leadership, quality improvement, and evidence-based practice implementation makes graduates prime candidates for these advanced roles. Over the course of a career, a DNP is likely to lead to higher lifetime earnings.
### 4. Years of Experience and Career Trajectory
As detailed in the previous section, experience is a primary driver of salary growth. This progression isn't just about time served; it's about the accumulation of skills and expertise.
- Clinical Acumen: An experienced CNM can confidently manage more complex clinical scenarios, requires less supervision, and can serve as a mentor and preceptor for new graduates. This expertise is highly valued.
- Leadership and Administration: With 5-10 years of experience, a CNM can transition into leadership roles. A Lead Midwife or Chief of Midwifery is responsible for scheduling, budgeting, staff management, and strategic planning for their department. These management positions come with a significant salary premium.
- Practice Ownership: The most experienced and entrepreneurial CNMs may choose to open their own private practice. While this carries the greatest financial risk, it also offers the highest potential reward.
### 5. Area of Specialization and Additional Certifications
While "Certified Nurse-Midwife" is itself a specialization, CNMs can acquire further sub-specialty skills and certifications that enhance their practice and increase their salary.
- Surgical First Assisting (RNFA): CNMs who obtain certification as a Registered Nurse First Assistant can surgically assist collaborating OB/GYN physicians during cesarean sections and other procedures. This added skill makes them more versatile and valuable to a hospital or surgical practice, often commanding a higher salary or additional stipends.
- Lactation Consulting (IBCLC): While all CNMs have training in lactation, becoming an International Board Certified Lactation Consultant (IBCLC) demonstrates a higher level of expertise. This can lead to specialized roles or make a candidate more attractive to practices that want to market comprehensive lactation support.
- Ultrasound Skills: Proficiency in limited obstetric ultrasound for tasks like confirming fetal viability, position, and fluid levels is a highly marketable skill that can increase efficiency and autonomy within a practice.
- Academic Roles: CNMs with a DNP or Ph.D. can work as faculty in nursing schools. While a full-time academic salary might be lower than a top clinical salary, it can be combined with part-time clinical practice for a very high total income.
### 6. In-Demand Skills
Beyond formal certifications, certain practical skills can make a CNM a more competitive candidate and justify a higher salary offer.
- Bilingualism: Fluency in a second language, particularly Spanish, is extremely valuable in many parts of the country. It improves patient care, safety, and satisfaction, and employers will often pay a premium for this skill.
- EHR/Technology Proficiency: Deep experience with major Electronic Health Record systems (like Epic or Cerner) reduces training time and improves workflow efficiency, making a candidate more attractive.
- Business and Management Acumen: Skills in billing, coding, and practice management are crucial for CNMs in private practice or those aspiring to leadership roles.
- Advocacy and Policy Work: Experience in professional advocacy, working with state legislatures on scope-of-practice issues, or serving on professional committees demonstrates leadership and a commitment to advancing the profession.
By strategically developing these areas—choosing a favorable location, pursuing advanced education, gaining diverse experience, and acquiring specialized skills—a Certified Nurse-Midwife can actively shape their career and significantly increase their earning potential over time.
---
Job Outlook and Career Growth for CNMs
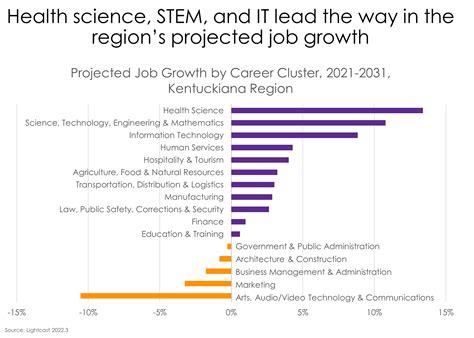
For those investing the significant time, effort, and financial resources required to become a Certified Nurse-Midwife, the long-term career outlook is a critical consideration. The forecast for CNMs is not just positive; it is exceptionally bright, driven by a confluence of healthcare trends, demographic shifts, and a growing recognition of the value of the midwifery model of care.
### An Unprecedented Demand for Services
The U.S. Bureau of Labor Statistics (BLS) provides the most authoritative projection for the profession. In its 2022-2032 forecast, the BLS projects that employment for Nurse Anesthetists, Nurse Midwives, and Nurse Practitioners will grow by a staggering 38 percent. This is more than ten times the average growth rate for all occupations in the U.S. economy.
This translates to approximately 11,800 new job openings for this group of APRNs each year over the decade, arising from both new job creation and the need to replace professionals who retire or transition to different occupations. While this statistic is for the combined group, the underlying factors fuel strong demand specifically for CNMs.
### Key Trends Driving Job Growth
Several powerful trends are converging to create this robust job market: