To practice medicine in New York City is to place yourself at the very heart of global ambition, relentless energy, and unparalleled human diversity. It’s a calling that demands the highest levels of skill, resilience, and compassion, practiced against the backdrop of an iconic skyline and within some of the world's most advanced medical institutions. For those who dream of this path, the questions are often as practical as they are profound: What does it truly mean to be a doctor here? And, given the city's notorious cost of living and the immense investment required, what is the reality of a doctor's salary in New York City?
This guide is designed to be your definitive resource, pulling back the curtain on the complex and often opaque world of physician compensation in the five boroughs. We will move beyond simple averages to dissect the nuanced factors that shape a doctor's earnings, from the crucial choice of specialty to the type of practice you join. The financial rewards can be substantial, with many physicians earning well into the six-figure range and top specialists exceeding half a million dollars annually. However, this journey is not for the faint of heart. I once spoke with an emergency room physician from Brooklyn who, after a grueling 12-hour shift that included treating a multi-car pile-up on the BQE, simply said, "You don't choose this life for the money, but the money allows you to survive this life." Her words capture the essence of this career: a profound commitment supported by the necessity of a commensurate income.
This article will provide you with a data-driven, comprehensive roadmap. We will explore not only the numbers but also the career trajectory, the job outlook in a post-pandemic world, and a step-by-step guide to embarking on this demanding and extraordinary career path.
### Table of Contents
- [What Does a Doctor in New York City Do?](#what-does-a-doctor-in-new-york-city-do)
- [Average Doctor Salary in New York City: A Deep Dive](#average-doctor-salary-in-new-york-city-a-deep-dive)
- [Key Factors That Influence a Doctor's Salary in NYC](#key-factors-that-influence-a-doctors-salary-in-nyc)
- [Job Outlook and Career Growth for NYC Doctors](#job-outlook-and-career-growth-for-nyc-doctors)
- [How to Become a Doctor in New York City](#how-to-become-a-doctor-in-new-york-city)
- [Conclusion: Is a Medical Career in NYC Right for You?](#conclusion-is-a-medical-career-in-nyc-right-for-you)
What Does a Doctor in New York City Do?
At its core, the role of a physician, whether in a quiet town or a bustling metropolis, is to diagnose, treat, and prevent human illness and injury. They are scientists, investigators, counselors, and healers. However, practicing medicine in New York City adds unique layers of complexity and opportunity to this fundamental mission.
The general responsibilities of a physician (M.D. or D.O.) remain constant. They include:
- Patient Examination and Diagnosis: Conducting thorough physical exams, taking detailed medical histories, and listening intently to patient concerns to identify health issues.
- Developing Treatment Plans: Ordering, performing, and interpreting diagnostic tests (like lab work, X-rays, and MRIs) to inform a comprehensive treatment strategy.
- Prescribing Medication and Therapies: Determining the appropriate medications, dosages, and therapeutic regimens for patients.
- Performing Procedures: Depending on their specialty, this can range from simple in-office procedures like suturing a wound to highly complex surgeries lasting many hours.
- Patient Counseling: Advising patients on diet, hygiene, and preventative healthcare measures to promote long-term wellness.
- Record Keeping: Meticulously documenting patient visits, diagnoses, treatments, and follow-ups in Electronic Health Records (EHRs).
- Collaboration: Working as part of a multidisciplinary team with other doctors, nurses, physician assistants, and healthcare professionals to ensure coordinated patient care.
In the context of New York City, these duties are amplified by the environment. An NYC doctor might treat patients from dozens of different countries in a single day, requiring cultural competency and, often, the use of translation services. They work within vast, high-volume hospital systems like Northwell Health or NYU Langone, navigating complex bureaucracies and managing incredibly high patient loads. The pressure is immense, but the access to cutting-edge research, technology, and a network of world-leading experts is unparalleled.
### A Day in the Life: Dr. Elena Ramirez, Internist at a Manhattan Academic Medical Center
To make this tangible, let's imagine a typical day for an internal medicine physician working in a large hospital-affiliated practice.
- 7:00 AM - 9:00 AM: Hospital Rounds. Dr. Ramirez begins her day at the hospital, not her clinic. She visits the handful of her primary care patients who have been admitted overnight or are recovering from procedures. She reviews their charts, speaks with the on-call residents and nurses, examines each patient, and adjusts their care plans before they are discharged.
- 9:00 AM - 9:30 AM: Chart Review and Prep. She travels to her outpatient clinic a few blocks away. She grabs a quick coffee and spends 30 minutes reviewing the charts for her morning patients, noting recent lab results, specialist reports, and reasons for their visits.
- 9:30 AM - 1:00 PM: Morning Clinic. Dr. Ramirez sees patients every 15-20 minutes. Her schedule includes a 65-year-old with newly diagnosed diabetes needing education on glucose monitoring, a 30-year-old finance professional with stress-induced hypertension, a tourist from Brazil with a severe respiratory infection, and a long-time patient for a routine annual physical. Each interaction requires a rapid-yet-thorough assessment and clear communication.
- 1:00 PM - 2:00 PM: Lunch and Administrative Tasks. Lunch is often eaten at her desk while she responds to a flood of emails, signs prescription refills, and returns urgent calls to patients and pharmacies. She also reviews and signs off on notes written by the medical residents she supervises.
- 2:00 PM - 5:00 PM: Afternoon Clinic & Telehealth. The afternoon brings another slate of patients. Two of these appointments are conducted via telehealth video calls, a now-permanent feature of her practice. She diagnoses a case of shingles, refers a patient with a suspicious mole to a dermatologist, and manages the complex medication regimen of an elderly patient with multiple chronic conditions.
- 5:00 PM - 6:30 PM: Charting and Follow-Up. The last patient has left, but the day is far from over. Dr. Ramirez spends the next 90 minutes completing her detailed notes in the EHR for every patient she saw. Failing to do so can delay billing and compromise patient care. She also sends referrals, reviews the day's lab results, and creates a task list for her medical assistant for the following day. This "pajama time" work, as it's often called, is a significant and often uncompensated part of a modern doctor's job.
This schedule highlights the intense blend of clinical work, administrative duty, and relentless time pressure that defines the life of many doctors in New York City.
Average Doctor Salary in New York City: A Deep Dive
Determining a single "average" salary for a doctor in New York City is challenging because the title "doctor" encompasses hundreds of specialties with vastly different earning potentials. However, by consulting authoritative sources, we can establish a reliable baseline and explore the ranges you can expect.
It's crucial to understand the data sources. The U.S. Bureau of Labor Statistics (BLS) provides robust, employer-reported data, often for broad metropolitan areas. Industry-specific reports, like the Doximity Physician Compensation Report, offer granular detail on specific specialties and cities, based on surveys of physicians themselves. Salary aggregators like Salary.com and Glassdoor provide real-time, user-reported data that can be very current but may have a smaller sample size.
### National vs. New York City Averages
First, let's set a national benchmark. According to the most recent BLS Occupational Employment and Wage Statistics data (May 2023), the national mean annual wage for key physician roles includes:
- Family Medicine Physicians: $235,930
- Internists, General: $242,190
- Pediatricians, General: $203,240
- Surgeons (All Other): $347,870
- Anesthesiologists: $339,420
Now, let's zoom in on New York City. The BLS groups its data into the "New York-Newark-Jersey City, NY-NJ-PA" metropolitan area, which is a very strong proxy for the city's market. For this metro area, the mean annual wages are:
- Family Medicine Physicians: $200,410
- Internists, General: $211,730
- Pediatricians, General: $207,170
- Surgeons (All Other): $373,260
- Anesthesiologists: >$239,200 (The BLS often caps the highest salaries at this "top of range" figure)
You might notice that primary care salaries in the NYC metro area appear *lower* than the national average according to the BLS. This can be misleading and is often attributed to a higher concentration of physicians in lower-paid residency programs and academic centers in the metro area data pool.
For a more realistic picture, we turn to industry-specific sources. The 2023 Doximity Physician Compensation Report, a gold standard in the industry, ranks New York City as #14 among the top 50 metro areas for physician compensation. It reports an average annual salary of $433,524 for physicians across all specialties in the NYC metro area. This figure is significantly higher because it focuses on post-residency attending physicians and more accurately reflects the earning power in this competitive market.
Salary.com, which analyzes employer-reported compensation data, provides the following ranges for New York, NY as of late 2023/early 2024:
- Physician - Family Practice: Median salary of $231,684, with a typical range between $204,115 and $265,309.
- Physician - Internal Medicine: Median salary of $253,391, with a typical range between $228,349 and $288,579.
- Surgeon - Orthopedic: Median salary of $559,623, with a typical range between $440,024 and $718,290.
### Salary by Experience Level in NYC
A physician's salary follows a distinct, sharp trajectory based on their career stage.
| Career Stage | Typical Years of Experience | Estimated Annual Compensation (NYC) | Notes |
| :--- | :--- | :--- | :--- |
| Resident/Fellow | 0-7 years (post-medical school) | $70,000 - $95,000 | This is a training stipend, not a full salary. Varies by program and post-graduate year (PGY). |
| Early Career Attending| 1-5 years (post-residency) | $200,000 - $350,000 | This is the major salary jump. Primary care is at the lower end, surgical specialties at the higher end. |
| Mid-Career Physician | 6-15 years | $250,000 - $500,000+ | Salary increases with experience, reputation, and patient volume. Production bonuses (RVUs) become significant. |
| Senior/Late Career | 16+ years | $300,000 - $700,000+ | Top earners in high-paying specialties with established practices or leadership roles can far exceed this. |
*Sources: Data compiled and estimated from GME residency program websites (e.g., Mount Sinai, NYU), Doximity, and Salary.com.*
### Beyond the Base Salary: Understanding Total Compensation
A physician's base salary is only one part of their financial picture. In a competitive market like New York City, the total compensation package is a critical negotiation point.
- Production Bonuses (RVU-based): This is one of the most common forms of incentive pay. Physicians are often given a base salary and then earn additional bonuses for productivity, measured in Relative Value Units (RVUs). An RVU is a measure of value used by Medicare that factors in the time, skill, and intensity required for a patient service. A physician who sees more patients or performs more complex procedures will generate more RVUs and thus a larger bonus.
- Sign-On and Relocation Bonuses: To attract top talent, especially in high-need specialties, NYC hospital systems frequently offer substantial sign-on bonuses. These can range from $15,000 to $50,000 or more, sometimes structured to be paid out over the first couple of years.
- Malpractice Insurance: This is a huge expense in New York, which is known for being a litigious state. Most hospital-employed physicians will have their malpractice insurance ("tail coverage" included) paid for by their employer. This benefit is worth tens of thousands of dollars per year.
- Health and Retirement Benefits: Comprehensive health, dental, and vision insurance are standard. Retirement plans typically include a 401(k) or, for non-profit hospitals, a 403(b), often with an employer match.
- Continuing Medical Education (CME) Allowance: Physicians are required to complete a certain number of hours of continuing education each year to maintain their license. Employers typically provide an annual allowance ($2,000 - $5,000) and paid time off to attend conferences or complete courses.
- Loan Repayment Programs: Some non-profit organizations and hospitals in underserved areas of NYC may offer student loan repayment assistance as a powerful recruitment tool, given that many physicians graduate with over $200,000 in debt.
Key Factors That Influence a Doctor's Salary in NYC

While averages provide a starting point, a doctor's actual take-home pay in New York City is determined by a confluence of critical factors. Understanding these variables is key to forecasting your own potential earnings and navigating your career choices.
### ### Specialty: The Single Biggest Differentiator
Without question, your chosen medical specialty is the most significant factor influencing your salary. The gap between primary care and procedural or surgical specialties is substantial across the country, and New York City is no exception. Proceduralists (those who perform procedures like surgeries or colonoscopies) are reimbursed at a much higher rate than physicians who primarily provide cognitive services (consultation and management).
Here is a comparison of average annual compensation for various specialties in the NYC metro area, illustrating the vast range.
| Specialty Group | Example Specialties | Estimated NYC Metro Area Salary Range |
| :--- | :--- | :--- |
| Top Tier (Surgical/Procedural) | Neurosurgery, Thoracic Surgery, Orthopedic Surgery | $700,000 - $1,000,000+ |
| High Tier (Surgical/Procedural) | Plastic Surgery, Cardiology (Invasive), Gastroenterology | $550,000 - $750,000 |
| Upper-Mid Tier (Procedural/Diagnostic)| Urology, Otolaryngology (ENT), Radiology, Anesthesiology | $450,000 - $600,000 |
| Mid Tier (Medical/Hospitalist) | Oncology, Emergency Medicine, Critical Care, Hospitalist | $350,000 - $450,000 |
| Lower Tier (Primary Care/Cognitive) | Internal Medicine, Family Medicine, Psychiatry, Pediatrics | $220,000 - $320,000 |
*Sources: Data compiled and estimated from the Doximity 2023 Physician Compensation Report, Medscape Physician Compensation Report 2023, and Merritt Hawkins reports.*
Why this massive gap? It's driven by the fee-for-service reimbursement system. A single complex spinal surgery can be reimbursed by insurance for an amount that would take a primary care physician hundreds of patient visits to equal. Furthermore, the training for top-tier specialties is longer and more competitive, and the personal risk (malpractice) is higher, all of which drive up compensation.
### ### Years of Experience & Career Progression
As detailed in the salary table above, a physician's career is marked by distinct financial stages.
1. Medical Student: This is a period of *negative* income. Students pay hefty tuition fees and accrue significant debt. The average medical school debt for the class of 2023 was $202,453, not including undergraduate loans.
2. Residency/Fellowship (PGY 1-7+): This is the apprenticeship phase. Residents work notoriously long hours for a stipend, not a market-rate salary. For the 2023-2024 academic year, resident stipends at major NYC institutions like Mount Sinai started around $74,000 for a PGY-1 (first-year resident) and increased to around $92,000 for a PGY-7 (senior fellow). While this seems low for a doctor, it is the necessary step toward full licensure and attending-level pay.
3. Attending Physician: Upon completing residency and board certification, a physician becomes an attending. This is when their salary jumps dramatically into the six-figure range appropriate for their specialty. In the first five years, physicians build their skills, patient base, and efficiency. Salary growth may be modest, based on contractual annual increases.
4. Established Physician (5+ years): After the initial years, compensation becomes more heavily tied to productivity (RVUs) or, in a private practice, partnership. This is where a doctor's reputation, referral network, and efficiency really begin to pay off, leading to significant salary growth throughout their mid-career. Senior partners in successful private practices often have the highest earning potential.
### ### Practice Setting: Hospital vs. Private Practice
Where a doctor works is nearly as important as what they do. The choice between being an employee of a large health system or running your own business has profound implications for both salary and lifestyle.
- Large Hospital System/Academic Medical Center (e.g., Northwell, NYU Langone, Mount Sinai, Montefiore):
- Pros: Stable, predictable salary. Excellent benefits package (health, retirement, paid malpractice). No administrative or business overhead. Access to world-class resources and colleagues.
- Cons: Lower ceiling on income potential compared to private practice. Less autonomy over schedule, practice style, and administrative decisions. Compensation is often tied to rigid institutional formulas and RVU targets.
- Salary Impact: Generally offers strong, competitive salaries, especially for early-career physicians who value stability. Academic positions may pay slightly less than community hospital positions but offer teaching and research opportunities.
- Private Practice (Group or Solo):
- Pros: Highest long-term earning potential. Full autonomy over the business, patient care, and lifestyle. Potential for partnership and equity in the practice.
- Cons: Significant financial risk and responsibility. Doctors must cover all overhead: rent for prime NYC real estate, staff salaries, billing services, IT, and exorbitant malpractice insurance premiums. Income can be volatile.
- Salary Impact: In the initial years, a private practice physician might earn less than their hospital-employed counterpart as they build the business. However, a successful, established private practice surgeon or specialist in NYC can have one of the highest earning potentials in the country. Solo primary care, however, is increasingly difficult to sustain financially in the city.
- Urgent Care Centers & "Doc-in-a-Box" Clinics:
- This is a rapidly growing sector. These facilities, owned by large corporations or private equity, hire physicians (often in Emergency Medicine or Family Medicine) on an hourly or salaried basis. The pay is competitive, often with a focus on work-life balance (e.g., shift work with no on-call duties), but offers little of the autonomy or long-term patient relationships of traditional practice.
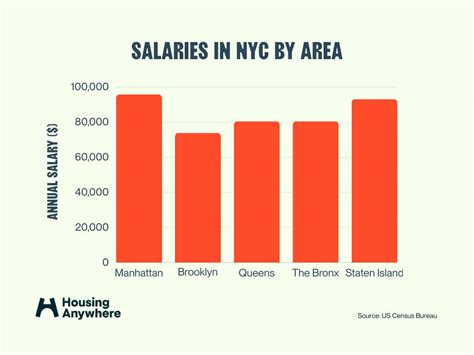
### ### Geographic Location within the NYC Metro Area
Even within the five boroughs and surrounding suburbs, salaries can vary.
- Manhattan: Tends to offer the highest nominal salaries, driven by the prestige of its institutions and the need to compensate for the astronomical cost of living and practice overhead. Top specialists with "Park Avenue" practices command the highest fees.
- The Other Boroughs (Brooklyn, Queens, The Bronx, Staten Island): Compensation is still very strong and highly competitive. Hospitals in these boroughs are aggressively recruiting to serve large, diverse populations. The cost of running a private practice can be significantly lower than in Manhattan, potentially leading to higher net income.
- Suburbs (Long Island, Westchester County, Northern New Jersey): These areas often have to offer salaries that are competitive with, or even exceed, city salaries to lure top talent away from the major academic hubs. A lower cost of living can make these compensation packages particularly attractive. Doximity's data often shows that some of the highest-paying jobs are located in affluent suburban communities.
### ### In-Demand Skills and Additional Qualifications
Beyond the basics, certain qualifications can add a premium to a doctor's salary.
- Fellowship Training: Completing a 1-3 year fellowship after residency to become a sub-specialist is the most common way to increase earnings. An orthopedic surgeon who completes a fellowship in spine surgery will earn significantly more than a general orthopedist.
- Leadership Roles: Taking on administrative responsibilities as a Medical Director, Chief of a department, or a member of a hospital's C-suite comes with a significant administrative stipend or a higher base salary.
- Bilingualism: In a city where hundreds of languages are spoken, fluency in a second language, particularly Spanish, Mandarin, Russian, or Bengali, can be a major asset, especially in community health settings or practices serving specific ethnic populations. While it might not always translate to a direct salary bump, it makes a candidate far more competitive for certain positions.
- Niche Procedural Skills: Mastering new, high-tech, or in-demand procedures (e.g., robotic surgery, minimally invasive techniques, specific interventional radiology procedures) can make a physician a highly sought-after and highly compensated asset for a hospital.
Job Outlook and Career Growth for NYC Doctors

For those investing more than a decade of their lives and hundreds of thousands of dollars in training, the long-term viability of their chosen career is paramount. Fortunately, the job outlook for physicians, both nationally and in New York City, remains exceptionally strong.
### National Job Growth Projections
The U.S. Bureau of Labor Statistics projects that overall employment for physicians and surgeons will grow by 3 percent from 2022 to 2032. While this is about the average for all occupations, it translates to approximately 24,00