In the chaotic, high-stakes world of emergency medicine, where every second counts and decisions carry immense weight, a new kind of clinical leader has emerged as indispensable: the Emergency Room Nurse Practitioner (ER NP). For nurses seeking the pinnacle of autonomy, challenge, and clinical responsibility, this career path represents a compelling summit. It's a role that demands a unique blend of sharp intellect, unshakable composure, and profound compassion. But beyond the immense personal and professional satisfaction, the financial rewards are substantial, with the potential for an emergency room nurse practitioner salary to reach well into the six-figure range, reflecting the advanced skills and critical importance of the position.
The journey to becoming an ER NP is demanding, but the destination is a career at the forefront of patient care. I once spoke with a seasoned ER NP who, in a single shift, managed the care of a multi-car pileup victim, stabilized a child in anaphylactic shock, and diagnosed a subtle stroke in an elderly patient who others had initially dismissed as merely confused. Her ability to rapidly assess, diagnose, and treat across such a wide spectrum of acute conditions underscored the immense value and expertise this role commands. It’s this level of impact that draws so many to the field, and it’s this level of expertise that justifies the impressive compensation package.
This guide is designed to be your definitive resource, whether you're an experienced RN considering your next step, a nursing student charting your future, or a healthcare administrator seeking to understand the value of this role. We will dissect every facet of an emergency room nurse practitioner salary, explore the factors that drive it, and lay out the precise roadmap to achieving this elite professional designation.
### Table of Contents
- [What Does an Emergency Room Nurse Practitioner Do?](#what-er-np-does)
- [Average Emergency Room Nurse Practitioner Salary: A Deep Dive](#salary-deep-dive)
- [Key Factors That Influence an ER NP's Salary](#key-factors)
- [Job Outlook and Career Growth for ER NPs](#job-outlook)
- [How to Become an Emergency Room Nurse Practitioner: A Step-by-Step Guide](#how-to-become)
- [Conclusion: Is a Career as an ER NP Right for You?](#conclusion)
What Does an Emergency Room Nurse Practitioner Do?

An Emergency Room Nurse Practitioner is an advanced practice registered nurse (APRN) who provides comprehensive care to patients of all ages in the emergency department (ED) and other urgent care settings. Functioning with a high degree of autonomy, often in collaboration with emergency physicians, they are responsible for assessing, diagnosing, and treating a vast range of acute illnesses and injuries. Their scope of practice bridges the gap between nursing and medicine, allowing them to manage a significant portion of the patient load in a busy ER.
The core of the ER NP's role is clinical decision-making under pressure. They are the frontline providers for patients presenting with everything from minor complaints like coughs and sprains to life-threatening emergencies such as heart attacks, strokes, severe trauma, and septic shock. They must possess the knowledge to differentiate between the benign and the critical, often with incomplete information and in a time-sensitive environment.
Core Responsibilities and Daily Tasks:
- Patient Triage and Assessment: Performing rapid and focused patient histories and physical examinations to determine the urgency and nature of the medical issue.
- Diagnostic Interpretation: Ordering and interpreting a wide array of diagnostic tests, including X-rays, CT scans, ultrasounds, EKGs, and laboratory work.
- Diagnosis and Treatment Planning: Formulating differential diagnoses and creating evidence-based treatment plans for acute conditions.
- Prescribing Medications: Prescribing medications, including analgesics, antibiotics, antiemetics, and other drugs necessary to manage acute symptoms and illnesses.
- Performing Procedures: Executing a variety of medical procedures, such as suturing lacerations, draining abscesses, reducing simple fractures and dislocations, performing lumbar punctures, and in some settings, inserting central lines or assisting with intubation.
- Patient and Family Education: Communicating diagnoses, treatment plans, and follow-up instructions clearly and compassionately to patients and their families.
- Collaboration and Consultation: Working as a key member of the interdisciplinary healthcare team, collaborating with ER physicians, specialists, nurses, technicians, and social workers to ensure seamless patient care.
- Disposition Planning: Determining the appropriate patient disposition, whether it be admission to the hospital, transfer to a specialty center, or discharge home with a safe follow-up plan.
> A Day in the Life of an ER NP
>
> 7:00 AM - Shift Handoff: The day begins with a detailed report from the night shift NP and physicians. You learn about the patients currently in the department, any pending lab results, and potential incoming traumas. You grab your coffee and log into the electronic health record (EHR) system.
>
> 7:30 AM - First Patient: You pick up your first chart: a 45-year-old male with crushing chest pain. You immediately perform a focused assessment, order an EKG and cardiac enzymes, and administer aspirin and nitroglycerin based on standing protocols, all while calmly reassuring the anxious patient. The EKG shows an ST-elevation myocardial infarction (STEMI). You activate the cath lab team and brief the cardiologist.
>
> 9:00 AM - The Rush Begins: The waiting room is filling up. Over the next three hours, you see a child with a febrile seizure, a college student with acute appendicitis, and an elderly woman who fell and may have a hip fracture. You suture a deep laceration on a chef's hand, order a CT scan for a patient with a head injury, and prescribe antibiotics for a patient with pneumonia.
>
> 1:00 PM - Trauma Alert: A "Level 1 Trauma" is announced overhead—a high-speed motor vehicle collision. You join the trauma team at the patient's bedside, assisting the physician with the primary and secondary surveys, helping to secure the airway, and ordering the necessary imaging and blood products.
>
> 3:00 PM - Charting and Follow-up: There's a brief lull. You use this time to meticulously document your patient encounters, follow up on lab results, and check in on the patients you’re planning to discharge.
>
> 5:00 PM - Winding Down: You manage a few more patients with less acute issues—a urinary tract infection, a sprained ankle, a bout of food poisoning. You begin preparing your sign-out report for the incoming evening shift NP, ensuring all critical information is clearly communicated.
>
> 7:00 PM - Shift End: After giving a thorough handoff, you finally sign out. You've managed over a dozen complex cases, performed multiple procedures, and made countless critical decisions. It was a physically and mentally exhausting day, but one filled with purpose and impact.
Average Emergency Room Nurse Practitioner Salary: A Deep Dive
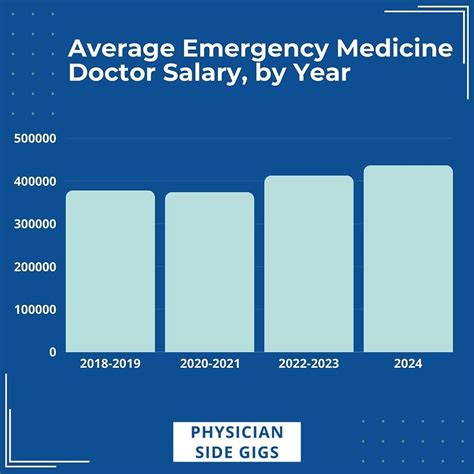
The compensation for an Emergency Room Nurse Practitioner is a direct reflection of their advanced education, specialized skills, and the high-stakes environment in which they work. While salary data for all Nurse Practitioners is robust, pinpointing the specific premium for ER specialization requires looking at more granular data from industry-specific sources.
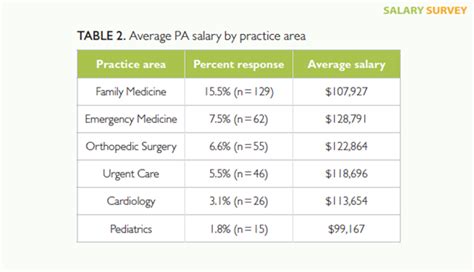
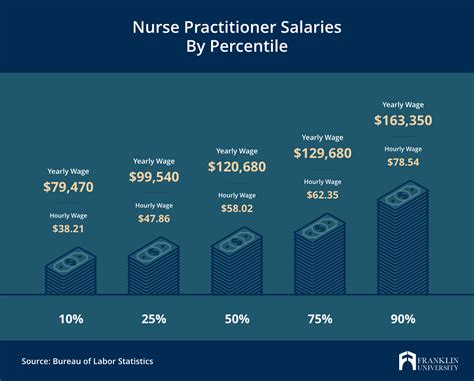
The U.S. Bureau of Labor Statistics (BLS) provides a broad overview for all Nurse Practitioners. As of May 2023, the median annual wage for Nurse Practitioners was $128,490. The lowest 10 percent earned less than $94,970, and the highest 10 percent earned more than $174,930. While this is an excellent baseline, ER NPs typically earn on the higher end of this spectrum due to the intensity and specialization of their role.
More specialized salary aggregators provide a clearer picture:
- Salary.com reports that as of May 2024, the average Emergency Room Nurse Practitioner salary in the United States is $135,165, with a typical salary range falling between $125,721 and $146,289.
- Payscale.com indicates a similar average base salary of approximately $120,417 per year, but this figure often increases significantly when accounting for bonuses and overtime, which are common in the ER setting.
- ZipRecruiter places the national average even higher, at $149,150 per year as of June 2024, with top earners reaching $188,500 annually.
The variance in these numbers highlights the influence of factors we will explore in the next section, such as location, experience, and work setting. A conservative and realistic salary expectation for a new ER NP would be in the $115,000 to $125,000 range, while an experienced, certified ER NP in a high-demand urban area could easily command a salary exceeding $160,000 or more.
### Salary by Experience Level
Like most professions, compensation for ER NPs grows substantially with experience. A seasoned NP who can manage high-acuity patients with minimal supervision is far more valuable than a recent graduate still mastering complex procedures and differential diagnoses.
| Experience Level | Typical Years of Experience | Typical Annual Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-2 Years | $110,000 - $128,000 | Recent graduate, often FNP-certified. Requires mentorship and supervision. Focus on lower-acuity "Fast Track" patients. |
| Mid-Career | 3-9 Years | $129,000 - $150,000 | Gained confidence and autonomy. Manages a wider range of patient acuities. May be pursuing ENP certification. |
| Senior/Experienced| 10+ Years | $151,000 - $175,000+ | Often ENP-certified. Acts as a clinical leader, preceptor, and mentor. Manages the most complex cases. May hold administrative roles (Lead NP). |
*Source: Data synthesized from Salary.com, Payscale, and AANP Salary Reports.*
### Beyond the Base Salary: A Look at Total Compensation
An ER NP's base salary is only one part of their total compensation package. The 24/7 nature of emergency medicine creates numerous opportunities for additional earnings and valuable benefits.
- Shift Differentials: This is a significant income booster. NPs working evenings, nights, weekends, and holidays receive a premium on their hourly rate, which can add thousands of dollars to their annual income. A night shift differential can range from 10% to 25% of the base hourly rate.
- Overtime Pay: While many NPs are salaried, those paid hourly can earn substantial overtime (time-and-a-half) for picking up extra shifts, which are frequently available in understaffed departments.
- Bonuses:
- Sign-On Bonuses: To attract talent in competitive markets, hospitals often offer sign-on bonuses ranging from $5,000 to $20,000 or more.
- Performance Bonuses: Some hospital systems tie bonuses to metrics like patient satisfaction scores (HCAHPS), door-to-provider time, or productivity (patients seen per hour).
- Retention Bonuses: Offered to experienced NPs to encourage them to stay with the organization long-term.
- Continuing Medical Education (CME) Allowance: Virtually all employers provide an annual allowance (typically $1,500 - $3,000) and paid time off to attend conferences and workshops to maintain licensure and stay current with medical advancements.
- Retirement Benefits: Most hospitals offer robust retirement plans, such as a 401(k) or 403(b), often with a generous employer match (e.g., matching 50% or 100% of employee contributions up to a certain percentage of salary).
- Health and Wellness Benefits: Comprehensive health, dental, and vision insurance is standard. Many institutions also offer life insurance, disability insurance, and wellness programs.
- Tuition Reimbursement: For NPs looking to advance their education to a Doctor of Nursing Practice (DNP), many hospital systems offer significant tuition assistance.
- Malpractice Insurance: Employers provide comprehensive professional liability (malpractice) insurance, a critical and expensive necessity in this high-risk specialty.
When all these components are combined, the total compensation for an experienced ER NP can easily be 15-25% higher than their base salary alone.
Key Factors That Influence an Emergency Room Nurse Practitioner Salary
While national averages provide a useful benchmark, an individual ER NP's salary is determined by a complex interplay of several key factors. Understanding these variables is crucial for both aspiring NPs planning their careers and current NPs aiming to maximize their earning potential. This section breaks down the most significant salary drivers in detail.
### 1. Level of Education and Certification
This is arguably the most powerful lever an NP can pull to influence their salary, especially in a specialized field like emergency medicine.
- Master of Science in Nursing (MSN) vs. Doctor of Nursing Practice (DNP): While the MSN is the current standard for entry-level practice, the DNP is a terminal degree focused on clinical leadership, evidence-based practice, and systems improvement. According to the 2020 AANP Salary Survey, NPs with a DNP degree earned a median of $7,000 more per year than those with an MSN. In a competitive ER environment, a DNP can provide an edge for leadership positions (e.g., Director of Advanced Practice Providers) which come with a significant pay increase.
- The Power of Specialty Certification: This is the single most important factor within education. Many NPs enter the ER with a Family Nurse Practitioner (FNP-C/BC) certification, which provides a broad, lifespan-focused knowledge base. While perfectly acceptable, they are often competing for jobs and salary with NPs who hold more specialized, acute-care-focused certifications.
- Emergency Nurse Practitioner (ENP-C): This board certification, offered by the American Academy of Nurse Practitioners Certification Board (AANPCB), is the gold standard for the specialty. It validates an NP's expertise specifically in emergency care. Obtaining the ENP-C can result in an immediate and significant salary increase, as it demonstrates a higher level of competence and reduces the training burden on an employer. Some institutions offer a direct salary differential for ENP-certified providers.
- Adult-Gerontology Acute Care Nurse Practitioner (AG-ACNP-BC): This certification focuses on the complex, acute, and critical care needs of adult patients. It is highly valued in the ER, particularly in Level I and II trauma centers that see a high volume of critically ill patients. An AG-ACNP may command a higher salary than an FNP in the same ER setting due to their specialized training in managing unstable patients.
### 2. Years of Experience
As highlighted in the previous section, experience is a primary driver of salary growth. The trajectory is not linear but occurs in stages.
- 0-2 Years (The Novice): During this phase, the NP is consolidating their academic knowledge with real-world clinical practice. They are developing procedural skills, learning departmental flow, and building confidence in their diagnostic abilities. Their salary reflects their status as a learner who requires more oversight.
- 3-5 Years (The Competent Practitioner): By this stage, the NP can handle a significant patient load with increased autonomy. They have seen a wide variety of cases and are comfortable managing moderately complex patients. Their value to the department increases, and so does their salary. This is often the period where NPs pursue the ENP certification.
- 5-10 Years (The Proficient Expert): These NPs are seasoned veterans. They can manage the highest acuity patients, perform advanced procedures, and act as a resource for junior NPs and even medical residents. They often take on roles as preceptors, mentors, or team leaders. Their salaries are in the upper quartile for the profession.
- 10+ Years (The Clinical Leader): With a decade or more of experience, these NPs are at the top of their clinical game. Many transition into formal leadership roles, such as Lead NP, APN Manager, or Director of the Emergency Department's advanced practice provider service. These administrative responsibilities come with top-tier salaries, often approaching or exceeding $200,000 in some markets.
### 3. Geographic Location
"Location, location, location" is as true in healthcare compensation as it is in real estate. Salaries for ER NPs vary dramatically by state, city, and even between urban and rural settings within the same state. This variation is driven by the cost of living, local market demand, and state-specific scope of practice laws.
High-Paying States: States in the Pacific West consistently offer the highest salaries for Nurse Practitioners. This is largely due to a high cost of living, strong union presence, and favorable practice environments.
- California: Average NP salaries are often the highest in the nation, with ER NPs in major metro areas like San Francisco and Los Angeles commanding salaries well above $170,000.
- Washington: Seattle and its surrounding areas are highly competitive markets with salaries often exceeding $150,000.
- Oregon: Similar to its neighbors, Oregon offers robust compensation, particularly in the Portland metro area.
- New York & New Jersey: High cost of living in the NYC metropolitan area drives salaries upward, frequently surpassing $150,000.
Lower-Paying States: States in the Southeast and parts of the Midwest tend to have lower average salaries, which is usually offset by a significantly lower cost of living.
- Alabama, Tennessee, South Carolina: These states often report median NP salaries closer to the national average or slightly below, typically in the $110,000 - $120,000 range. However, a $120,000 salary in Nashville can have more purchasing power than a $150,000 salary in San Jose.
Urban vs. Rural Divide:
- Urban Centers: Major metropolitan areas have a higher concentration of large hospitals, Level I trauma centers, and academic medical centers. While this means more job opportunities and higher nominal salaries, it also means a higher cost of living and more competition.
- Rural Areas: Rural and underserved areas can be a hidden gem for ER NPs. To attract providers to remote locations, these facilities often offer very competitive salaries, significant sign-on bonuses, and sometimes even loan repayment assistance through federal or state programs. An ER NP might be one of only a few providers in a critical access hospital, granting them immense responsibility and commensurate pay.
### 4. Work Setting & Employer Type
The type of facility an ER NP works in has a profound impact on their daily responsibilities, patient population, and compensation structure.
- Level I & II Trauma Centers (Academic or Large Urban Hospitals): These settings typically offer the highest salaries. They see the highest acuity patients and require NPs to be proficient in trauma and critical care. The work is intense, but the pay and learning opportunities are top-tier. These institutions are more likely to require or strongly prefer DNP degrees and ENP or ACNP certifications.
- Community Hospitals (Suburban/Mid-Sized Cities): These hospitals form the backbone of emergency care in the U.S. Salaries are very competitive, often just slightly below those at major trauma centers. The work-life balance may be more favorable, with a mix of high-acuity and lower-acuity patients.
- Urgent Care Centers: While distinct from ERs, many Urgent Care centers are owned by large health systems and staffed by ER-trained NPs. The pay structure can vary. Some offer lower base salaries but high productivity bonuses, while others offer competitive hourly rates. The work is generally lower acuity, which may be reflected in slightly lower overall compensation compared to a high-volume ER.
- Government/VA Hospitals: Working for the Department of Veterans Affairs (VA) or other government entities offers a unique package. Salaries are set on a transparent government pay scale and are often very competitive with the private sector. The true advantage lies in the unparalleled federal benefits package, which includes a generous pension plan (FERS), excellent health insurance, and extensive paid time off.
- Locum Tenens: This involves working as a temporary, independent contractor to fill short-term staffing needs. *Locum tenens* NPs command extremely high hourly rates—often 25-50% higher than their salaried counterparts. This path offers flexibility and high income but typically does not include benefits like health insurance, retirement plans, or paid time off, which the NP must fund themselves.
### 5. In-Demand Skills and Sub-Specialization
Beyond core competencies, certain advanced skills can make an NP a more valuable asset and a stronger salary negotiator.
- Advanced Procedural Skills: Proficiency in procedures beyond basic suturing is a major value-add. This includes ultrasound-guided line placement, lumbar punctures, chest tube insertion, and conscious sedation. NPs who can perform these skills independently increase departmental efficiency and can command a higher salary.
- Point-of-Care Ultrasound (POCUS): The ability to use ultrasound at the bedside to diagnose conditions like pneumothorax, deep vein thrombosis (DVT), or pericardial effusion is a rapidly growing and highly sought-after skill in emergency medicine. Formal POCUS certification or a robust portfolio can be a significant bargaining chip.
- Pediatric Emergency Experience: While many ERs see children, NPs with specialized experience or certification in pediatric emergency care (CPEN for nurses, though no direct NP equivalent exists, experience is key) are highly valued, especially in mixed-age ERs without a dedicated pediatric section.
- Leadership and Administrative Skills: Experience in scheduling, quality improvement projects, training new staff, or serving on hospital committees demonstrates value beyond clinical care. These skills are prerequisites for advancing to higher-paying leadership roles.
Job Outlook and Career Growth for ER NPs

For those investing the time, effort, and financial resources to become an Emergency Room Nurse Practitioner, the long-term career prospects are exceptionally bright. The demand for Nurse Practitioners, in general, is one of the fastest-growing in any profession, and the specialized skills of an ER NP place them in a particularly strong position within the healthcare landscape.
The U.S. Bureau of Labor Statistics (BLS) projects a phenomenal growth rate for nurse practitioners, nurse anesthetists, and nurse midwives. Employment in this group is projected to grow 45 percent from 2022 to 2032, which is astronomically faster than the average for all occupations. This translates to about 118,600 openings for these advanced practice nurses each year, on average, over the decade.
Several powerful, long-term trends are fueling this explosive demand:
1. An Aging Population: The baby boomer generation is aging, leading to a greater need for healthcare services to manage complex, chronic, and acute health conditions. Older adults are more frequent users of the emergency department.
2. Physician Shortages: The Association of American Medical Colleges (AAMC) continues to project significant shortages of physicians, particularly in primary and emergency care. ER NPs are perfectly positioned to fill this gap, providing high-quality, efficient care and ensuring patients have access to timely treatment.
3. Focus on Cost-Effective Care: Healthcare systems are under immense pressure to control costs without sacrificing quality. Nurse Practitioners are a proven, cost-effective solution. They can manage a large percentage of ER patients independently or in collaboration with physicians, at a lower salary point than their physician colleagues, which improves the financial viability of the department.
4. Increased NP Autonomy: A growing number of states are moving toward "Full Practice Authority," which allows NPs to practice to the full extent of their education and training without direct physician supervision. As of 2024, more than half of U.S. states have adopted these laws, expanding the roles and responsibilities—and thus the demand—for NPs.
### Emerging Trends and Future Challenges
The role of the ER NP is not static; it is continually evolving. Staying ahead of these trends is key to long-term career success.
- Telehealth Integration: The use of telehealth for emergency triage and follow-up is expanding. NPs who are comfortable with virtual platforms and can effectively