Introduction

For generations, the decision to pursue a career in medicine has been driven by a profound desire to help others, a fascination with the complexities of the human body, and the intellectual challenge of diagnosis and treatment. It is a true vocation, demanding immense dedication, resilience, and compassion. But alongside this calling is a practical reality: a medical career in England is a significant investment of time, effort, and finances. Therefore, understanding the financial rewards—the England doctor salary—is not just a matter of curiosity, but a crucial component of career planning. The path is long, but the destination offers not only immense personal satisfaction but also significant financial stability and a well-defined structure for growth. The salary of a doctor in England is not a single figure but a complex, multi-layered system that evolves dramatically from the first day as a newly qualified junior to the pinnacle of the profession as a senior consultant.
I once had the privilege of shadowing a senior consultant in a busy London hospital. In the space of a single morning, she calmed a terrified patient, deftly explained a complex diagnosis to a family, mentored a junior doctor through a difficult procedure, and chaired a departmental meeting. It was a masterclass in expertise, empathy, and leadership. That experience crystallized for me that a doctor's salary isn't just compensation for tasks performed; it's a reflection of a decade or more of rigorous training, immense responsibility, and a lifelong commitment to learning and care. It's the tangible value society places on the people we trust with our lives.
This comprehensive guide will demystify the salary structure for doctors in England. We will dissect the official NHS pay scales, explore the myriad factors that influence earnings, from specialization to private practice, and provide a clear roadmap for anyone aspiring to this esteemed profession.
### Table of Contents
- [What Does a Doctor in England Do?](#what-does-a-doctor-do)
- [Average Doctor Salary in England: A Deep Dive](#salary-deep-dive)
- [Key Factors That Influence a Doctor's Salary](#key-factors)
- [Job Outlook and Career Growth for Doctors in England](#job-outlook)
- [How to Become a Doctor in England: A Step-by-Step Guide](#how-to-get-started)
- [Conclusion: Is a Career in Medicine Right for You?](#conclusion)
---
What Does a Doctor in England Do?
To understand a doctor's salary, one must first appreciate the sheer breadth and depth of their responsibilities. The title "doctor" encompasses a vast range of roles and specialties, but all are united by a core mission: to maintain and restore human health through the practice of medicine. The vast majority of doctors in England are employed by the National Health Service (NHS), the country's publicly funded healthcare system, which shapes the structure of their careers and daily work.
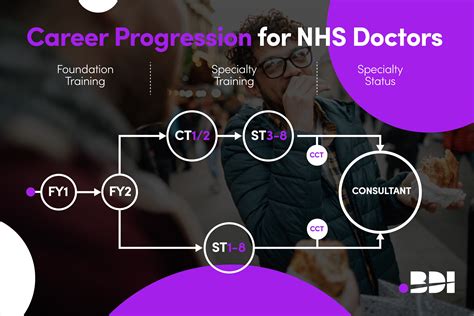
The medical career path in England is highly structured. After graduating from medical school, all doctors enter a two-year Foundation Programme. These "junior doctors" (Foundation Year 1 and 2) rotate through various medical and surgical specialties, gaining broad, hands-on experience under senior supervision. Their work is the bedrock of hospital care, involving clerking new patient admissions, performing initial assessments, ordering tests, prescribing medications, and carrying out essential ward-based tasks.
Following the Foundation Programme, doctors choose a path of specialization. This can be broadly divided into two streams:
1. General Practice (GP): These doctors undergo at least three years of specialty training to become the first point of contact for patients in the community. They diagnose and treat a wide spectrum of common illnesses, manage chronic conditions like diabetes and hypertension, provide preventative care and health education, and refer patients to hospital specialists when necessary.
2. Hospital-Based Specialties: This path is longer, typically taking five to eight years of specialty training after the Foundation Programme. Doctors train to become specialists in fields like Cardiology, Oncology, Paediatrics, General Surgery, Psychiatry, or Anaesthetics. As they progress, they are known as Specialty Registrars (StRs), taking on increasing responsibility for patient care, performing complex procedures, and contributing to the training of more junior doctors. The ultimate goal for most hospital doctors is to become a Consultant, the most senior grade of hospital doctor responsible for a team and the overall management of patients under their care.
### A "Day in the Life" of a Medical Specialty Registrar (StR)
To make this tangible, let's imagine a day for "Dr. Evans," a fourth-year trainee in Cardiology:
- 8:00 AM - 9:00 AM (Handover): The day begins with a handover meeting from the night team. Dr. Evans receives updates on all patients on the cardiology ward, noting any overnight events, urgent test results, or sick patients requiring immediate attention.
- 9:00 AM - 1:00 PM (Ward Round): Dr. Evans joins the Consultant-led ward round. They move from bed to bed, reviewing each patient. For each one, Dr. Evans presents the case history, recent progress, and investigation results. They discuss the management plan with the consultant, write in the patient notes, update prescription charts, and request necessary scans or procedures.
- 1:00 PM - 2:00 PM (Lunch & Admin): A quick lunch, often combined with "jobs." This means following up on the plans made during the ward round: chasing blood test results, liaising with radiologists to schedule an urgent echocardiogram, and speaking with a patient's family to provide an update.
- 2:00 PM - 4:00 PM (Cardiology Clinic): Dr. Evans runs an outpatient clinic under the supervision of a consultant. They see patients with a variety of conditions, from post-heart attack follow-ups to new referrals for chest pain. This involves taking detailed histories, performing examinations, and making decisions about medication and further investigations.
- 4:00 PM - 5:30 PM (Referrals & Discharges): The final part of the day is spent seeing new patient referrals from the A&E department and preparing discharge summaries for patients going home. This documentation is vital for ensuring continuity of care with the patient's GP.
- 5:30 PM (Evening Handover): Dr. Evans hands over care of the ward patients to the on-call evening team, highlighting any particularly unwell patients or outstanding tasks before heading home—unless, of course, they are the one on call, in which case their shift continues into the night.
This snapshot reveals a role that is intellectually demanding, physically draining, and carries immense responsibility. The salary structure is designed to reflect the progression through these increasingly challenging stages.
---
Average Doctor Salary in England: A Deep Dive

The salary of a doctor in England is almost entirely governed by nationally agreed-upon pay scales, primarily for those working in the NHS. This creates a transparent, predictable, but also relatively rigid system. Unlike professions where salary is highly negotiable from the outset, a doctor's pay is determined by their grade (stage of training or seniority) and years of experience within that grade.
The primary sources for this data are NHS Employers, the organisation representing the NHS in workforce matters, and the British Medical Association (BMA), the main trade union and professional body for doctors. The figures cited here are based on the pay scales for 2023/2024.
It's important to note that the "average" salary for a doctor in England can be misleading, as the range is incredibly wide. A newly qualified doctor earns a fraction of a senior consultant. Therefore, it's more accurate to break down the salary by career stage.
| Career Stage / Grade | Typical Years of Experience Post-Graduation | Basic Salary Range (2023/2024) | Notes |
| :--- | :--- | :--- | :--- |
| Foundation Doctor Year 1 (FY1) | 0-1 years | £32,398 | First job after medical school. Provisional GMC registration. |
| Foundation Doctor Year 2 (FY2) | 1-2 years | £37,303 | Full GMC registration. Increased responsibility. |
| Specialty Registrar / Core Trainee (StR/CT) | 2-10 years | £43,923 - £63,152 | Longest training period. Salary increases annually at set 'nodal pay points'. |
| Specialty & Associate Specialist (SAS) Doctors | Varies (often 10+ years) | £52,542 - £99,592 | Senior, non-consultant grade. Multiple contract types and pay scales exist. |
| Consultant | Typically 8-10+ years | £93,666 - £126,281 | Senior grade. Salary increases with years of experience as a consultant. |
| General Practitioner (GP) | Typically 5+ years | ~£70,000 - £120,000+ | Varies significantly. Most are independent contractors or partners in a practice. |
*Source: NHS Employers and the British Medical Association (BMA) Pay Scales for 2023/2024.*
### Breakdown of Compensation Components
A doctor's payslip is more than just their basic salary. Several other components significantly impact their total take-home pay, particularly for doctors in training.
- Basic Pay: This is the core salary determined by the national pay scales as detailed in the table above. It reflects the doctor's grade and years of service.
- Pay for Additional Hours: Doctors in training are contracted for a standard 40-hour week. Any hours worked above this are paid at an enhanced rate.
- Enhanced Pay for Unsocial Hours: The most significant addition for junior doctors. A percentage enhancement is paid for any work scheduled at night (between 9 PM and 7 AM), on weekends, or on public holidays. This is often referred to as "banding" in older contract terminology. For a trainee on a rota with many nights and weekends, this can increase their basic salary by 30-50%.
- On-Call Allowance: Doctors on a non-resident on-call rota receive an allowance for the availability they provide. Currently, this is set at 8% of their basic salary.
- London Weighting: A supplemental payment for doctors working in London and the surrounding fringe zones to compensate for the significantly higher cost of living. This can add several thousand pounds to the annual salary. For example, the inner London weighting is £2,162 per year.
- Recruitment and Retention Premia (RRPs): For certain "hard-to-fill" specialties, such as Emergency Medicine or Psychiatry, the NHS may offer additional payments to attract and retain doctors in those fields.
- Clinical Excellence Awards (CEAs) / National Clinical Impact Awards (NCIAs): For consultants, this is a prestigious and highly competitive award scheme that recognizes individuals who contribute most to the NHS over and above their standard job expectations. These awards can add a substantial amount to a consultant's salary, ranging from £20,000 to £40,000 per year, though the system has been reformed in recent years.
- Pension: Doctors are eligible for the NHS Pension Scheme, which is one of the most comprehensive public sector pension schemes in the UK. Both the employee and the NHS (as the employer) make significant contributions. While this reduces take-home pay, it is an extremely valuable long-term benefit.
For General Practitioners, the model is different. Most GPs are not directly salaried employees of the NHS. Instead, they are partners or salaried employees of a GP practice, which operates as an independent business contracted by the NHS to provide services. GP partners' income is derived from the practice's profits, which depend on the number of patients, the services they provide, and how efficiently the practice is run. This introduces a level of business management and financial risk not present for hospital doctors, but also offers higher earning potential for successful practice partners.
---
Key Factors That Influence a Doctor's Salary

While the NHS pay scales provide a clear framework, several key variables determine a doctor's precise salary and overall earning potential. Understanding these factors is crucial for any medical professional looking to plan their financial future.
### 1. Stage of Training and Seniority (Level of Education)
This is the single most dominant factor in the NHS system. In medicine, "education" is a continuous process that directly corresponds to seniority and pay.
- Medical School (Undergraduate): This is the prerequisite, typically a 5 or 6-year degree. There is no salary during this time; in fact, it represents a significant financial investment.
- Foundation Programme (FY1/FY2): Upon graduation, you enter the workforce at the lowest rung of the ladder. An FY1 doctor starts at a basic salary of £32,398. This increases to £37,303 in the second year. This period is effectively a mandatory, supervised apprenticeship.
- Specialty Training (Core/Registrar Level): This is the long middle phase of a doctor's career development. The pay scale for doctors in training (StRs) is a ladder with specific "nodal points." A doctor entering specialty training starts at the bottom of this scale (£43,923) and moves up annually. For example, a registrar in their final year of training (perhaps 8 years post-graduation) would be at the top of the scale, earning a basic salary of £63,152.
- Consultant Grade: Achieving a Certificate of Completion of Training (CCT) and being appointed as a consultant represents a monumental jump in both responsibility and salary. The starting basic salary for a new consultant is £93,666. This scale is based on years of experience *as a consultant*. The salary rises through eight "pay thresholds," typically on an annual basis, up to a maximum basic pay of £126,281 for a consultant with over 8 years of experience. This progression is automatic, provided performance is satisfactory.
### 2. Years of Experience
As illustrated above, experience is codified directly into the NHS pay structure. You do not negotiate a raise based on a successful project; you progress through pre-determined pay points based on time served in a particular grade.
- Within Training: A doctor's pay automatically increases each year they successfully complete within the training programme. This predictable growth provides financial stability during a long and demanding period.
- As a Consultant: The consultant contract is designed to reward long-term service. A consultant who has worked for the NHS for 20 years will have a significantly higher basic salary than one who is newly appointed, purely due to this structured progression. According to BMA data, a consultant on Threshold 1 earns £93,666, while one on Threshold 8 earns £126,281—a difference of over £32,000 based on experience alone.
- SAS Doctors: The Specialty and Associate Specialist (SAS) grade also has its own multi-year pay scale, allowing for significant salary growth over a long career for doctors who choose this non-consultant senior path.
### 3. Geographic Location
Unlike some professions where salaries vary dramatically by region, the core NHS basic pay is national. A consultant in Liverpool has the same basic pay scale as a consultant in Bristol. However, location still has a major impact on total compensation and disposable income.
- London Weighting: This is the most formal geographic salary influence. To offset the high cost of living in the capital, the NHS applies a "High Cost Area Supplement." According to NHS Employers, this is currently £2,162 per year for those in inner London. While helpful, many argue it does not fully compensate for the difference in housing and transport costs.
- Private Practice Opportunities: This is the most significant, albeit informal, geographic factor. The concentration of wealth, private hospitals, and insured patients is much higher in London and the South East. A consultant in a specialty with high private demand (e.g., Orthopaedics, Cardiology, Dermatology) can potentially double their NHS salary through private work in London. These opportunities may be far more limited in other parts of the country, making the effective earning potential much lower, even if the basic NHS salary is the same.
- Regional Demand: Certain rural or less popular areas may have difficulty recruiting, sometimes leading to more readily available consultant posts or locum opportunities, which can be lucrative.
### 4. Employer Type: NHS vs. Private Sector
The vast majority of doctors in England will spend all or most of their careers working for the NHS. However, the private sector presents a significant and often very lucrative alternative or supplement.
- National Health Service (NHS): The UK's largest employer.
- Pros: Unparalleled job security, a world-class pension scheme, predictable and transparent pay progression, extensive training and development opportunities.
- Cons: Pay is relatively rigid and not subject to individual negotiation. It can be a highly bureaucratic environment, and workload pressures are immense.
- Private Hospitals and Clinics: (e.g., Bupa, Nuffield Health, HCA Healthcare)
- How it Works: Consultants working in the NHS can typically use their non-NHS time to see private patients. They are granted "practising privileges" at private hospitals and function as independent practitioners, setting their own fees (though often guided by insurance company rates).
- Salary Impact: This is the single biggest factor that separates high-earning doctors from the rest. Earnings are fee-for-service. A private surgical procedure can earn a surgeon several thousand pounds. A private consultation can be £200-£400. Top consultants in high-demand fields in London can earn an additional £100,000 to £300,000+ per year on top of their NHS salary. Salary aggregators like Glassdoor often reflect this blended income, showing average consultant salaries far higher than the NHS baseline, with some top-end figures reaching £250,000-£300,000.
- Locum Work: Doctors can work as locums (temporary staff) through agencies, either in the NHS or private sector. Locum rates are typically much higher than salaried pay to compensate for the lack of job security, pension, and sick pay. A locum consultant can earn £80-£120 per hour, making it a very high-income option, albeit a less stable one.
### 5. Area of Specialization
While the NHS training and consultant pay scales are largely the same regardless of specialty, the choice of specialization has a profound impact on long-term earning potential, primarily through the availability of private work.
- High Private Practice Potential:
- Orthopaedics: Joint replacements, sports injuries.
- Cardiology: Angiograms, private consultations.
- Ophthalmology: Cataract surgery, laser eye surgery.
- Dermatology: Cosmetic procedures, private skin checks.
- Gastroenterology: Private endoscopies and colonoscopies.
- Plastic Surgery: A mix of reconstructive (NHS) and cosmetic (private) work.
- Moderate to Low Private Practice Potential:
- Emergency Medicine: Almost exclusively NHS-based.
- Palliative Care: Primarily based in the NHS and hospice sector.
- General Paediatrics: While some private paediatric work exists, it's a smaller market.
- Public Health: A salaried role within public health bodies.
- General Practice: As discussed, GPs operate as independent businesses. Their income depends on practice management, list size, and offering additional services (e.g., minor surgery, travel clinics), making it a specialty with high variance in earnings.
### 6. High-Value Skills and Additional Responsibilities
Within the NHS structure, there are ways to increase income and career progression beyond standard clinical work. These roles recognise leadership, academic, and management skills.
- Management & Leadership Roles: Consultants can take on additional paid responsibilities. A Clinical Lead might receive one or two additional paid sessions (PAs) for their work. A Clinical Director or Medical Director, with responsibility for a whole directorate or hospital trust, receives a significant salary supplement, often pushing their total NHS earnings to £150,000-£200,000+.
- National Clinical Impact Awards (NCIAs): As mentioned, these awards are a direct financial reward for consultants who demonstrate outstanding contributions in areas like research, innovation, teaching, and leadership that have a national impact.
- Academic Work: Many consultants hold joint appointments with a university. This involves teaching medical students, conducting research, and publishing papers. This can sometimes come with a salary supplement or separate remuneration from the university.
- Medico-legal Work: Providing expert witness reports for legal cases is a highly specialized and lucrative side activity for experienced consultants. It is paid for privately by law firms and can be a significant source of additional income.
- Teaching and Training: Doctors who take on formal roles in postgraduate medical education, such as being a Training Programme Director, receive payment for this additional responsibility.
---
Job Outlook and Career Growth for Doctors in England
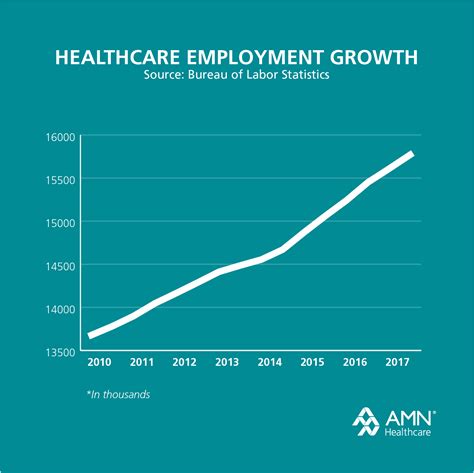
The career outlook for qualified doctors in England is exceptionally strong and stable. The demand for medical professionals consistently outstrips supply, a trend that is projected to continue for the foreseeable future. This creates a high degree of job security that is rare in many other professions.
### Demand and Workforce Projections
While the U.S. Bureau of Labor Statistics (BLS) is the standard for American job outlooks, the key sources for the UK are NHS England, the General Medical Council (GMC), and health-focused think tanks like The King's Fund and the Nuffield Trust.
The NHS Long Term Workforce Plan, published in June 2023, provides the most authoritative outlook. It highlights a critical and ongoing shortage of doctors and sets out ambitious targets to address this. Key takeaways include:
- High Demand: The plan acknowledges that without action, the NHS in England could face a shortfall of up to 360,000 staff by 2037, with doctors being a critical part of this gap.
- Drivers of Demand: An aging population with more complex, chronic health needs is the primary driver. Advances in medical technology and treatments also mean there is more that medicine can offer, further increasing demand.
- Planned Growth: To meet this demand, the government plans to significantly increase the number of medical school places, aiming to double the number of students entering training by 2031. This signals a clear, long-term commitment to expanding the medical workforce.
The GMC's annual "The state of medical education and practice in the UK" report consistently shows that while the number of doctors on the register is growing, so are the pressures. High rates of burnout and intentions to leave or reduce hours are significant challenges, but they also underscore the intense demand and the value placed on existing and future doctors. For an individual doctor, this environment means that once qualified, finding employment is virtually guaranteed.
### Emerging Trends and Future Challenges
The profession is not static. Several trends are shaping the future of medicine in England and the careers of doctors within it.
1. Portfolio Careers: Increasingly, doctors are moving away from the traditional single-role career. A "portfolio career" might involve working part-time in the NHS, doing some private practice, holding a teaching position, and engaging in medico-legal work. This allows for greater flexibility, work-life balance, and varied income streams.
2. Technological Integration: The role of technology is rapidly expanding. Telemedicine consultations have become mainstream. Artificial Intelligence (AI) is being developed to aid in diagnostics, particularly in radiology and pathology. Doctors of the future will need to be digitally literate and adaptable, working alongside technology to enhance patient care, not be replaced by it.
3. Shift to Community-Based Care: The NHS is actively trying to shift more care out of expensive hospitals and into the community. This will likely increase the demand and importance of General Practitioners and other community-based specialists.
4. Focus on Generalism: While specialization remains crucial, there is a growing recognition of the need for doctors with broad, generalist skills who can manage patients with multiple complex conditions, both in hospitals (e.g., Acute Medicine) and in General Practice.
5. Workforce Well-being and Burnout: This is perhaps the greatest challenge. The intense workload, administrative burden, and emotional toll of the job lead to high rates of burnout. The NHS and professional bodies are increasingly focused on improving working conditions, promoting flexibility, and supporting doctor well-being to ensure the sustainability of the workforce.
### How to Stay Relevant and Advance
Advancement in medicine is a marathon, not a sprint. The career path is well-defined, but proactivity is key to reaching the highest levels.
- Lifelong Learning: Medicine changes constantly. A commitment to Continuing Professional Development (CPD) is not just a requirement for revalidation by the GMC; it is essential for providing good care and remaining an expert in your field.
- Develop a Niche: Within your chosen specialty, develop a sub-specialist interest or expertise. This could be a particular procedure, a specific patient group, or a research area. This makes you a more valuable asset and can open doors to leadership and academic opportunities.
- Cultivate Soft Skills: Technical and diagnostic skills are
