For those with a passion for intricate problem-solving, a desire to profoundly impact patient quality of life, and an ambition for a rewarding, high-earning career, the field of gastroenterology represents a pinnacle of medical practice. As a career analyst who has guided countless professionals, I've seen many aspiring doctors weigh their options, and the role of a gastroenterologist consistently emerges as one of the most compelling. It’s a specialty that combines deep intellectual knowledge with hands-on procedural skill, offering a dynamic and financially prosperous path. But what does that prosperity actually look like? The average gastroenterologist salary is one of the highest among all medical specialties, typically ranging from $400,000 to over $650,000 annually, with top earners exceeding $1,000,000.
I recall a conversation with a close friend who struggled for years with a debilitating, undiagnosed digestive condition. It impacted his work, his social life, and his mental health. The turning point was finding a skilled gastroenterologist who didn't just prescribe medication, but meticulously performed diagnostic procedures, identified the root cause—a complex form of Inflammatory Bowel Disease—and crafted a long-term management plan. Seeing my friend regain his life underscored for me that these specialists don't just treat diseases; they restore hope and functionality.
This comprehensive guide will illuminate every facet of a gastroenterologist's career, with a deep, data-driven focus on salary and the factors that shape it. We will move beyond simple averages to provide an expert analysis of the financial landscape, the long-term outlook, and the rigorous yet achievable path to entering this esteemed profession.
### Table of Contents
- [What Does a Gastroenterologist Do?](#what-does-a-gastroenterologist-do)
- [Average Gastroenterologist Salary: A Deep Dive](#average-gastroenterologist-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Become a Gastroenterologist](#how-to-become-a-gastroenterologist)
- [Conclusion: Is a Career in Gastroenterology Right for You?](#conclusion)
What Does a Gastroenterologist Do?

A gastroenterologist, often referred to as a "GI doctor," is an internal medicine physician who has undergone extensive, specialized training in the management of diseases concerning the gastrointestinal (GI) tract and liver. This complex system includes the esophagus, stomach, small intestine, large intestine (colon), rectum, pancreas, gallbladder, bile ducts, and liver. They are the ultimate experts on how the body digests food, absorbs nutrients, and removes waste.
Their role is a fascinating blend of cognitive medicine and technical, hands-on procedures. Unlike some specialists who may spend their days primarily in an office or an operating room, a gastroenterologist’s work is remarkably varied.
Core Roles and Responsibilities:
- Diagnosis and Treatment of a Wide Spectrum of Conditions: GI doctors manage an incredible range of health issues, from common ailments to life-threatening diseases. This includes:
- Gastroesophageal Reflux Disease (GERD): Chronic acid reflux and heartburn.
- Peptic Ulcer Disease: Sores in the lining of the stomach or small intestine.
- Inflammatory Bowel Disease (IBD): Chronic inflammation of the digestive tract, primarily Crohn's disease and ulcerative colitis.
- Irritable Bowel Syndrome (IBS): A common disorder affecting the large intestine, causing cramping, abdominal pain, and bloating.
- Hepatitis: Inflammation of the liver (A, B, C, autoimmune).
- Cirrhosis and Liver Failure: Advanced scarring and dysfunction of the liver.
- Gallbladder and Biliary Tract Disease: Including gallstones and blockages.
- Pancreatitis: Inflammation of the pancreas.
- Celiac Disease: An immune reaction to eating gluten.
- Gastrointestinal Cancers: Including colorectal, stomach, esophageal, and pancreatic cancer.
- Performing Endoscopic Procedures: This is a cornerstone of the specialty and a major reason for the high compensation. Gastroenterologists are highly skilled in using endoscopes—thin, flexible tubes with a light and camera—to visualize, diagnose, and treat conditions inside the GI tract. Key procedures include:
- Upper Endoscopy (EGD): To examine the esophagus, stomach, and first part of the small intestine.
- Colonoscopy: To examine the entire colon and rectum, crucial for colorectal cancer screening and polyp removal.
- Flexible Sigmoidoscopy: To examine the lower part of the colon.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): A specialized procedure to diagnose and treat problems in the liver, gallbladder, bile ducts, and pancreas.
- Endoscopic Ultrasound (EUS): Combines endoscopy with ultrasound to obtain detailed images and tissue samples of the digestive tract and surrounding organs.
- Patient Consultation and Management: A significant portion of their time is spent in a clinical setting, meeting with patients to discuss symptoms, review medical history, order tests, and develop comprehensive, long-term treatment plans. This requires exceptional communication skills and empathy.
- Hospital Care: Gastroenterologists are often called to the hospital to consult on patients with acute GI issues, such as gastrointestinal bleeding, severe pancreatitis, or acute liver failure.
---
### A Day in the Life of a Gastroenterologist
To make this tangible, consider a typical "split day" for a GI doctor in a private practice or hospital setting:
Morning (7:30 AM - 12:00 PM): Procedure Block
- 7:30 AM: Arrive at the endoscopy suite. Review the day's schedule of procedures with the nursing and anesthesia team.
- 7:45 AM: Meet the first patient, a 52-year-old for a screening colonoscopy. Explain the procedure, answer last-minute questions, and ensure informed consent is obtained.
- 8:00 AM - 11:45 AM: Perform a series of procedures. This could include three screening colonoscopies (removing several polyps in one), one upper endoscopy for a patient with chronic reflux, and another colonoscopy for a patient with known Crohn's disease to assess disease activity.
- 11:45 AM: Speak with the family members of the patients, explaining the findings and next steps. Dictate procedure notes into the electronic health record (EHR).
Afternoon (1:00 PM - 5:00 PM): Clinic Block
- 1:00 PM: Arrive at the office. Quickly review the afternoon's patient list with their medical assistant.
- 1:15 PM: See a new patient, a 35-year-old with symptoms suggestive of IBS. Take a detailed history, perform a physical exam, and discuss a diagnostic and management plan.
- 1:45 PM: Follow-up appointment with a 65-year-old patient being treated for Hepatitis C. Review recent lab work, which shows the virus is now undetectable. Share the good news and discuss long-term liver monitoring.
- 2:15 PM - 4:30 PM: Continue seeing a mix of new and follow-up patients with various conditions like GERD, celiac disease, and post-polypectomy surveillance.
- 4:30 PM - 5:30 PM (or later): "Clean up" time. Finalize patient notes, review lab and pathology reports that came in during the day, respond to patient messages, and handle prescription refills. This administrative time is a significant part of the job.
This schedule highlights the dynamic nature of the work—a balance between highly technical, focused procedures and the interpersonal, analytical work of clinical consultations.
---
Average Gastroenterologist Salary: A Deep Dive
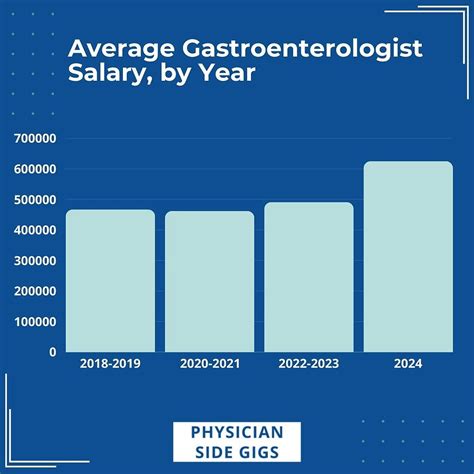
Gastroenterology consistently ranks among the top-earning medical specialties, surpassed only by a few surgical subspecialties like orthopedics and plastic surgery. The high compensation is a direct reflection of the extensive training required, the high demand for their services, and the procedural nature of the work, which generates significant revenue for hospitals and practices.
It's important to note that salary data can vary slightly based on the source, the year of the survey, and the components included (e.g., salary vs. total compensation). We will synthesize data from the most reputable sources to provide a clear and accurate picture.
National Average and Typical Range
According to the most recent and widely cited industry reports, the national average salary for a gastroenterologist in the United States falls into a lucrative bracket.
- Medscape's 2023 Physician Compensation Report, a leading authority, places the average gastroenterologist salary at $501,000 per year.
- Doximity's 2023 Physician Compensation Report reports a slightly higher average, at $512,542.
- Salary aggregators provide similar ranges. For instance, Salary.com (as of late 2023) shows a median salary of $435,996, with a typical range falling between $367,931 and $514,641. The discrepancy often lies in whether the data includes bonuses and productivity incentives, which are a huge part of a GI doctor's income.
Therefore, a realistic and comprehensive salary range for a full-time gastroenterologist is $375,000 to $650,000, with the median hovering around $500,000. Entry-level positions start strong, and experienced, high-producing physicians can easily surpass $750,000 and even approach or exceed the seven-figure mark.
### Salary by Experience Level
Like any profession, compensation grows significantly with experience, efficiency, and reputation. In medicine, this is often tied to how quickly and effectively a physician can see patients and perform procedures (measured in work Relative Value Units, or wRVUs).
Here is a typical salary progression, combining data from industry reports and compensation consultants:
| Experience Level | Years in Practice | Typical Annual Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level/Early Career | 0-3 Years | $350,000 - $450,000 | Just finished fellowship. Often starts with a guaranteed salary for the first 1-2 years before transitioning to a productivity-based model. Focus is on building a patient base and becoming efficient. |
| Mid-Career | 4-10 Years | $450,000 - $600,000 | Highly efficient in the clinic and endoscopy suite. Has an established reputation and a strong referral base. May be on a partnership track in a private practice. |
| Senior/Experienced | 11-20+ Years | $550,000 - $750,000+ | At peak earning potential. May have taken on leadership roles (e.g., department chief, managing partner). In private practice, partners at this stage are earning a share of the group's overall profits. |
*(Note: These are general estimates. Top performers in high-paying regions or practice types can exceed these ranges at every level.)*
### A Deeper Look at Compensation Components
A gastroenterologist's paycheck is rarely just a flat salary. The total compensation package is a complex structure designed to incentivize productivity.
- Base Salary: This is the guaranteed portion of the income. In hospital-employed models, this may be the largest component. In private practice, it might be a more modest "draw" against future earnings.
- Productivity Bonus (wRVU-based): This is the most significant variable. The wRVU (work Relative Value Unit) is a metric used by Medicare and commercial payers to value the work involved in a physician's service. Every patient visit and procedure is assigned a wRVU value. For example, a complex office visit might be worth 2.0 wRVUs, while a colonoscopy might be worth 4.5 wRVUs. Physicians are often paid a certain dollar amount per wRVU they generate above a set threshold. A productive GI doctor can generate a substantial bonus through this model, often adding $100,000 to $300,000+ to their base salary.
- Profit Sharing / Partnership Income: For those who become partners in a private practice, this is a game-changer. They receive a share of the practice's net profits after all expenses are paid. This can include revenue from the practice's own endoscopy center, pathology services, and infusion center, significantly boosting total income.
- Sign-On Bonus: To attract top talent, especially in underserved areas, health systems and practices often offer substantial sign-on bonuses. These can range from $25,000 to over $100,000.
- Call Pay: Gastroenterologists are part of an on-call rotation for hospital emergencies. Many employment models include a per-diem rate for being on call and additional compensation for any procedures performed after hours.
- Benefits and Perks: The value of the complete benefits package should not be underestimated. It almost always includes:
- Comprehensive Health, Dental, and Vision Insurance
- Generous Retirement Plans: Such as 401(k) or 403(b) with significant employer matching contributions.
- Malpractice Insurance: A crucial and expensive necessity, almost always fully covered by the employer.
- Continuing Medical Education (CME) Allowance: An annual stipend (e.g., $5,000 - $15,000) to cover the costs of attending conferences and staying current in the field.
- Paid Time Off (PTO): Typically 4-6 weeks per year.
- Relocation Assistance: For physicians moving to a new area for the job.
Understanding this complete picture is essential. A job offer with a slightly lower base salary but a more favorable productivity model and profit-sharing potential can be far more lucrative in the long run.
---
Key Factors That Influence Salary

While the national averages provide a useful benchmark, a gastroenterologist's actual earnings are determined by a complex interplay of several key factors. Aspiring and practicing GI doctors who understand these variables can strategically position themselves to maximize their earning potential throughout their careers.
###
1. Geographic Location
Where a gastroenterologist chooses to practice is one of the single most powerful determinants of their salary. The dynamic is often counterintuitive; practicing in a major, desirable coastal city like New York or Los Angeles does not always translate to the highest pay. This is due to market saturation (more GIs competing for patients) and higher overhead costs.
Conversely, states in the Southeast and Midwest often offer the highest compensation to attract physicians to areas with greater need and less competition.
Highest-Paying States for Gastroenterologists (in no particular order, based on multiple 2023 reports):
- Kentucky: Often cited as a top-paying state due to high demand.
- Tennessee: Strong demand and favorable practice environments.
- Indiana: Consistently ranks among the top-paying states.
- Alabama: High need for specialists drives up compensation.
- Florida: A large, aging population creates constant demand for GI services.
- Oklahoma: Favorable market dynamics for physicians.
Lower-Paying (but still high-income) States:
- Maryland: Proximity to numerous academic centers and high physician density.
- Massachusetts: Similar dynamics to Maryland, with high market saturation in Boston.
- Colorado: A desirable location that attracts many physicians, increasing competition.
- District of Columbia: Very high physician density for its size.
The Urban vs. Rural Dynamic:
Generally, physicians in rural or smaller metropolitan areas earn more than their counterparts in large, saturated urban centers. A hospital system in rural Wisconsin might offer a starting salary of $550,000 plus a large sign-on bonus to attract a GI doctor, whereas a similar position at a major academic center in Chicago might start closer to $400,000. This premium is paid to compensate for the location and to fill a critical community need.
###
2. Type of Practice
The setting in which a gastroenterologist works dramatically impacts their compensation structure and earning ceiling.
- Private Practice (Partner): This model offers the highest earning potential. After an initial period as an employee (typically 2-3 years), a physician can be offered partnership. As a partner, they not only earn from their own clinical work but also share in the overall profits of the practice. If the practice owns its endoscopy center, infusion suite, or pathology lab, the ancillary revenue can be immense. The trade-off is significant: partners share in the business risks, administrative responsibilities, and management headaches. Top-earning partners in successful private practices can earn well over $800,000 to $1,000,000+.
- Private Practice (Employee): This is a common starting point. The physician is an employee of the group, receiving a salary and/or productivity bonus. This offers a stable income without the risks of ownership. The salary is excellent but capped below what a partner makes. It serves as the "partnership track" in many groups.
- Hospital or Health System Employed: This is an increasingly common model. The physician is a direct employee of a hospital or large multi-specialty group. This provides maximum stability, predictable hours (in theory), and excellent benefits. The hospital handles all administrative tasks, billing, and overhead. Compensation is typically a base salary plus a wRVU-based productivity bonus. While the income is very strong (often in the $450,000 - $650,000 range), it generally has a lower ceiling than private practice partnership because the physician does not share in the facility fees from procedures.
- Academic Medicine: Gastroenterologists at university hospitals and academic medical centers are faculty members. Their role is a "three-legged stool": clinical care, teaching (medical students, residents, fellows), and research. Salaries in academia are consistently lower than in private practice or hospital-employed settings, often ranging from $300,000 to $450,000. The lower salary is offset by other benefits: intellectual stimulation, the prestige of a university affiliation, dedicated time for research, and often a better lifestyle with less pressure for high-volume procedural work.
###
3. Level of Education and Sub-specialization
The educational path to becoming a gastroenterologist is fixed and extensive, and is the fundamental justification for the high salary.
- The Foundational Path: 4 years of undergraduate + 4 years of medical school (MD or DO) + 3 years of Internal Medicine residency + 3 years of Gastroenterology fellowship = 14 years of post-high school education and training.
This rigorous, non-negotiable path creates a high barrier to entry. Board certification from the American Board of Internal Medicine (ABIM) in both Internal Medicine and Gastroenterology is the standard and is required by virtually all employers and insurance panels.
Within gastroenterology, further sub-specialization can significantly impact earning potential, primarily by enabling the physician to perform more complex, higher-reimbursing procedures.
- General Gastroenterology: The backbone of the specialty, focusing on common GI issues, EGD, and colonoscopy.
- Hepatology: A focus on liver diseases. A one-year Transplant Hepatology fellowship can be completed after the standard GI fellowship, leading to roles in liver transplant centers. This can command a higher salary in specific academic or large hospital settings.
- Advanced/Therapeutic Endoscopy: This is a key area for increased income. An additional fourth year of fellowship is dedicated to mastering complex procedures like ERCP and EUS. Physicians with this training are in high demand as they can manage more complex biliary and pancreatic diseases, and these procedures have high wRVU values. An advanced endoscopist can often earn a 10-20% premium over a general gastroenterologist.
- Inflammatory Bowel Disease (IBD): While not always leading to a direct salary increase, becoming a recognized IBD expert can lead to a high volume of complex patient referrals, indirectly boosting productivity and income.
###
4. In-Demand Skills (Clinical and Non-Clinical)
Beyond board certification, certain skills make a gastroenterologist more valuable and can lead to higher compensation.
- Procedural Efficiency and Safety: The ability to perform high-quality endoscopic procedures safely and efficiently is paramount. A physician who can maintain a low complication rate while managing a high volume of procedures will be a top earner in any productivity-based system.
- Expertise in ERCP/EUS: As mentioned, this is the most sought-after clinical skill set that directly translates to higher pay.
- Business Acumen: For physicians in private practice, understanding the business of medicine is crucial. Skills in financial management, contract negotiation, and operational efficiency can directly increase the profitability of the practice and, therefore, personal income.
- Leadership and Administrative Skills: Taking on roles like Medical Director of an Endoscopy Unit, Chief of Gastroenterology, or a managing partner in a private practice often comes with an additional administrative stipend and can increase overall compensation.
- Excellent Communication and "Bedside Manner": While a "soft skill," this has a hard financial impact. Patients who feel heard and respected are more likely to be compliant with treatment, refer friends and family, and leave positive online reviews, all of which help build a thriving and profitable practice.
---
Job Outlook and Career Growth

The career outlook for gastroenterologists is exceptionally strong and is projected to remain so for the foreseeable future. Several powerful demographic and healthcare trends are fueling a sustained, high demand for their specialized services.
Projected Job Growth
The U.S. Bureau of Labor Statistics (BLS) groups all physicians and surgeons together in its projections. For this broad category, the BLS projects a job growth of 3% between 2022 and 2032. While this number seems modest, it's crucial to understand the context for a specialty like gastroenterology. The demand within this specialty is expected to significantly outpace the average.
A 2021 workforce analysis from the American Medical Association (AMA) highlighted that gastroenterology is facing a potential shortage, with demand expected to exceed the supply of physicians in the coming years.
Key Drivers of Demand:
1. An Aging Population: The "baby boomer" generation is now well into the age range for increased GI health issues. Most importantly, the U.S. Preventive Services Task Force recommends screening colonoscopies for average-risk individuals beginning at age 45. With millions of Americans entering and moving through this age bracket, the demand for screening colonoscopies—a primary function of GIs—is immense and growing.
2. Increased Prevalence of GI Diseases: The incidence of many GI conditions is on the rise. This includes obesity-related liver disease (NAFLD/NASH), GERD, and inflammatory bowel diseases like Crohn's and colitis. These are chronic conditions that require long-term management by a specialist.
3. Advances in Diagnostic and Therapeutic Technology: The development of new endoscopic techniques, better imaging, and more effective treatments means that gastroenterologists can do more for their patients than ever before. This expands the scope of the specialty and the reasons for patients to seek their care.
4. Emphasis on Preventive Care: The success of colorectal cancer screening programs has cemented the value of preventive care in the public and medical consciousness. This public health priority ensures a steady and government-backed stream of patients for gastroenterologists.
Emerging Trends and Future Challenges
The field is not static. Staying relevant and advancing requires an awareness of future trends:
- Artificial Intelligence (AI) in Endoscopy: AI platforms are being developed and implemented to help physicians detect polyps during colonoscopy in real-time. GIs who adopt and become proficient with this technology may improve their detection rates, leading to better patient outcomes and potentially higher quality-of-care ratings.
- Rise of Private Equity in Healthcare: An increasing number of private gastroenterology practices are being acquired by private equity firms. This can lead to very high initial buyouts for practice partners but may change the practice's culture, compensation structures, and focus towards maximizing profit. This is a major, and often controversial, trend in the field.
- Telehealth Integration: While gastroenterology is a procedure-heavy specialty, telehealth has found a firm place for follow-up visits, management of chronic conditions, and initial consultations, increasing efficiency and patient access to care.
- Shift Towards Value-Based Care: The healthcare system is slowly moving from a fee-for-service model (where payment is based on volume) to a value-based model (where payment is tied to patient outcomes and cost-effectiveness). While wRVU productivity will likely remain dominant for years, GIs will need to increasingly demonstrate high-quality, efficient care to thrive.
Advice for Career Advancement:
- Never Stop Learning: Commit to lifelong learning through CME, reading journals, and attending major conferences like Digestive Disease Week (DDW).
- Consider a Sub-specialty: An extra year of training in advanced endoscopy can pay for itself many times over throughout a career.
- Develop a Niche: Become
