In the intricate and ever-evolving world of healthcare, a landscape governed by complex laws and life-or-death decisions, a specialized legal expert is not just valuable—they are indispensable. This is the world of the healthcare attorney. If you are drawn to a career that merges the intellectual rigor of law with the profound human impact of medicine, and you're curious about its financial rewards, you've arrived at the definitive resource. This guide will not only demystify the healthcare attorney salary but will illuminate the entire career path, from law school to the partner's desk.
The potential in this field is immense. The U.S. healthcare industry is a multi-trillion-dollar behemoth, and every transaction, policy, and patient interaction is underpinned by a dense web of regulations. Consequently, the demand for legal professionals who can navigate this complexity is robust, with average salaries often ranging from $130,000 to over $250,000 annually, and top earners pushing well beyond that. I once had the privilege of working alongside a team of healthcare lawyers advising a hospital during a complex merger. Watching them deftly handle everything from physician contracts to intricate Stark Law compliance, I realized their work wasn't just about protecting an institution; it was about ensuring that thousands of patients would continue to receive seamless, high-quality care. They were the silent architects of the system's stability.
This article is designed to be your comprehensive roadmap. Whether you're a pre-law student, a current law student, or a practicing attorney considering a specialization, we will explore every facet of this rewarding career.
### Table of Contents
- [What Does a Healthcare Attorney Do?](#what-does-a-healthcare-attorney-do)
- [Average Healthcare Attorney Salary: A Deep Dive](#average-healthcare-attorney-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion: Is a Career as a Healthcare Attorney Right for You?](#conclusion)
What Does a Healthcare Attorney Do?

A healthcare attorney is far more than a courtroom litigator. They are strategic advisors, compliance experts, and transactional facilitators who operate at the intersection of law, business, and medicine. Their primary role is to guide clients—which can include hospitals, physician groups, insurance companies, pharmaceutical corporations, and even individual practitioners—through the labyrinthine legal requirements of the healthcare industry. Their work is multifaceted, touching upon nearly every operational aspect of a healthcare organization.
The core responsibilities of a healthcare attorney can be broadly categorized into three main areas: regulatory compliance, transactional work, and litigation.
1. Regulatory and Compliance: This is the bedrock of healthcare law. Attorneys in this area help clients understand and adhere to a vast array of federal and state laws. Key statutes they work with daily include:
- The Health Insurance Portability and Accountability Act (HIPAA): Ensuring the privacy and security of patient health information.
- The Stark Law and Anti-Kickback Statute (AKS): Preventing illegal patient referrals and financial arrangements between physicians and other healthcare entities.
- The Emergency Medical Treatment and Labor Act (EMTALA): Governing how hospitals must treat patients in emergency situations.
- Medicare and Medicaid Regulations: Advising on billing, reimbursement, and enrollment requirements.
A compliance-focused attorney spends their time developing internal policies, conducting risk assessments, training staff, and responding to government audits or investigations.
2. Transactional Work: These attorneys are the deal-makers. They structure, negotiate, and execute the business deals that allow the healthcare industry to function and grow. This includes:
- Mergers and Acquisitions (M&A): Facilitating the consolidation of hospitals, clinics, and physician practices.
- Contract Drafting and Negotiation: Creating employment agreements for physicians, service agreements with vendors, and managed care contracts with insurance payers.
- Joint Ventures: Establishing legal structures for partnerships between different healthcare organizations, such as a hospital and a specialized imaging center.
3. Litigation and Risk Management: When disputes arise, litigators step in. This can involve:
- Medical Malpractice Defense: Representing doctors, nurses, and hospitals accused of negligence.
- Fraud and Abuse Defense: Defending clients against allegations of false claims or improper billing from government bodies like the Department of Justice (DOJ) or the Office of Inspector General (OIG).
- Staff Privileging Disputes: Representing either physicians or hospitals in conflicts over a doctor's right to practice at a facility.
### A Day in the Life of a Mid-Career Healthcare Attorney
To make this tangible, let's imagine a day for "Sarah," a 7th-year associate at a mid-sized law firm specializing in healthcare.
- 8:30 AM - 9:30 AM: Sarah starts her day reviewing overnight emails. The general counsel of a regional hospital client has an urgent question about a new telehealth policy and its compliance with cross-state licensing laws. Sarah quickly researches the latest state-specific guidance and drafts a preliminary advisory email.
- 9:30 AM - 11:00 AM: She joins a conference call with a team handling the acquisition of a small cardiology practice by a larger health system. Her role is to review the due diligence documents related to the practice's existing insurance contracts and identify any potential liabilities under the Anti-Kickback Statute.
- 11:00 AM - 1:00 PM: Sarah focuses on a major drafting project: a professional services agreement for a new hospitalist group. She carefully words the compensation clauses to ensure they fit within a "commercially reasonable" safe harbor under the Stark Law. She meticulously records her 2.0 billable hours for this task.
- 1:00 PM - 1:30 PM: A quick lunch while she skims industry news from publications like *Modern Healthcare* and *Fierce Healthcare* to stay abreast of regulatory changes.
- 1:30 PM - 4:00 PM: Sarah shifts gears to a litigation matter. She prepares a key physician witness for an upcoming deposition in a medical malpractice defense case, reviewing the medical chart with him and anticipating the plaintiff's attorney's line of questioning.
- 4:00 PM - 6:00 PM: She attends an internal department meeting to discuss new guidance from the Centers for Medicare & Medicaid Services (CMS). The partners lead a discussion on how this will impact their clients' billing practices and what proactive advice they need to provide.
- 6:00 PM onwards: Sarah returns to the telehealth inquiry from the morning, conducting deeper research to provide a comprehensive formal memo. She finalizes her time entries for the day before heading home, knowing tomorrow will bring a new set of complex and critical challenges.
This snapshot illustrates the dynamic and intellectually stimulating nature of the work. It requires a lawyer who can pivot quickly between being a meticulous rule-follower, a savvy business negotiator, and a fierce advocate.
Average Healthcare Attorney Salary: A Deep Dive
The financial compensation for a healthcare attorney is a significant draw, reflecting the high stakes of their work and the specialized knowledge required. While salaries can vary dramatically, the overall picture is one of robust and lucrative earning potential.
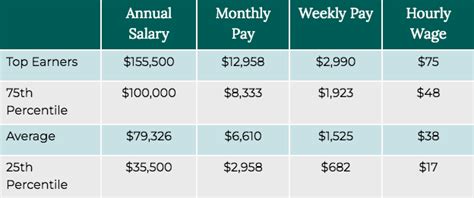
According to a comprehensive analysis of data from sources like Salary.com, Payscale, and Glassdoor, the national average base salary for a healthcare attorney in the United States falls between $155,000 and $175,000 per year as of early 2024. However, this single figure only tells part of the story. The realistic salary range is incredibly wide, stretching from approximately $90,000 for an entry-level position in a non-profit or state government role to well over $400,000 for a partner at a major law firm ("BigLaw") or a Chief Legal Officer at a large hospital system.
To provide a clearer picture, let's break down the compensation structure by experience level.
### Healthcare Attorney Salary by Experience Level
The career path of an attorney is marked by a steep and consistent increase in earning potential as they accumulate expertise and a proven track record. The salary brackets generally align with titles like Associate, Senior Associate/Counsel, and Partner/General Counsel.
| Experience Level | Typical Title(s) | Typical Base Salary Range | Key Responsibilities & Value |
| :--- | :--- | :--- | :--- |
| Entry-Level | Junior Associate, Staff Attorney | $90,000 - $140,000 | Primarily focused on research, document review, and drafting initial versions of contracts and memos. They support senior attorneys and learn the foundational laws. |
| Mid-Career | Associate, Senior Associate | $140,000 - $225,000 | Manages significant portions of transactions or cases, has direct client contact, and begins to develop a niche specialization. They operate with greater autonomy. |
| Senior-Level | Senior Associate, Counsel, Junior Partner, Senior Counsel (In-House) | $200,000 - $350,000 | Leads complex transactions, manages teams of junior lawyers, serves as the primary relationship manager for key clients, and may begin to develop their own book of business. |
| Executive/Partner | Equity Partner, General Counsel, Chief Legal Officer | $350,000 - $750,000+ | Drives firm or department strategy, originates significant new business, provides high-level strategic advice to C-suite executives, and has ultimate responsibility for legal outcomes. |
*Source: Aggregated data analysis from Salary.com, Payscale, and reports from legal recruiting firms like Major, Lindsey & Africa, updated for 2024 projections. Note that BigLaw starting salaries often follow a separate, higher "Cravath Scale," which can start closer to $225,000 for first-year associates in major markets.*
### Beyond the Base Salary: Understanding Total Compensation
A healthcare attorney's income is rarely limited to their base salary. A significant portion of their earnings comes from variable compensation and benefits, which differ based on the type of employer.
1. Bonuses:
- Law Firms: Bonuses are a major component of compensation. They are typically tied to two factors: the firm's overall profitability for the year and the individual attorney's performance, measured primarily in billable hours. A mid-career associate at a large firm might bill between 1,900 and 2,100 hours per year. Meeting or exceeding this target can result in a year-end bonus ranging from 15% to 50% (or more) of their base salary. For partners, bonuses are replaced by a share of the firm's profits.
- In-House (Hospitals, Corporations): In-house counsel bonuses are more often tied to the overall performance of the company and the achievement of specific departmental or individual goals (Key Performance Indicators, or KPIs). These are typically smaller and more predictable than law firm bonuses, often in the 10-25% range of base salary.
2. Profit Sharing and Equity:
- Law Firm Partners: The ultimate financial goal for many law firm attorneys is making equity partner. This means they are no longer a salaried employee but a part-owner of the firm. Their compensation is a direct share of the firm's profits, which can lead to annual earnings in the high six or even seven figures.
- In-House Counsel: For senior in-house roles at for-profit healthcare companies (like large hospital chains or pharmaceutical companies), compensation can include stock options or Long-Term Incentive Plans (LTIPs). This gives them an ownership stake in the company, aligning their financial success with the company's growth.
3. Benefits and Perks:
- Health and Retirement: Comprehensive health insurance and robust 401(k) or 403(b) retirement plans with generous employer matching are standard.
- Professional Development: Employers typically cover the costs of state bar association fees, continuing legal education (CLE) credits, and attendance at major industry conferences.
- Work-Life Balance (Relative Term): While the legal profession is demanding, in-house roles often offer a more predictable schedule than law firm life, which is a valuable non-monetary benefit for many. Government roles are renowned for offering the best work-life balance and excellent job security.
Understanding this complete compensation picture is crucial. A law firm offer of $200,000 base + a potential $50,000 bonus might be financially superior to a $220,000 in-house salary with a $20,000 bonus, but it will likely come with significantly higher demands on time and energy.
Key Factors That Influence a Healthcare Attorney Salary
The wide salary ranges discussed above are not arbitrary. They are the result of a complex interplay of factors that determine an attorney's market value. For anyone looking to maximize their earning potential in this field, understanding these levers is paramount. This section provides an exhaustive breakdown of the six primary drivers of a healthcare attorney's salary.
### 1. Level of Education and Credentials
While a Juris Doctor (J.D.) degree is the non-negotiable entry ticket, additional education and certifications can significantly enhance a candidate's profile and, consequently, their salary.
- The J.D. and Law School Prestige: The reputation of the law school from which you graduate has the most substantial impact at the very beginning of your career. Graduates from "T14" (top 14) law schools are heavily recruited by the highest-paying BigLaw firms and are often able to command a starting salary premium. These firms pay a lockstep salary (the "Cravath Scale") to all first-year associates regardless of their law school, but getting the interview and the offer is far easier from a top-tier school. While this effect diminishes over time as experience becomes more important, it provides a powerful initial launchpad.
- Advanced Degrees (LL.M., M.P.H., M.H.A.):
- Master of Laws (LL.M.) in Health Law: For attorneys who did not specialize during their J.D. or are transitioning from another practice area, a one-year LL.M. program from a university with a top-ranked health law program (like the University of Houston, Saint Louis University, or Loyola University Chicago) can be a powerful credential. It demonstrates a deep commitment to the field and provides an intensive dose of specialized knowledge, making a candidate more attractive to employers and potentially justifying a higher salary.
- Dual Degrees (J.D./M.P.H. or J.D./M.H.A.): Pursuing a dual degree in law and Public Health (M.P.H.) or Health Administration (M.H.A.) is a strategic move that pays long-term dividends. It equips the attorney with the language and perspective of their clients. They don't just understand the law; they understand the operational, financial, and clinical challenges of the healthcare system. This dual expertise is highly sought after for senior in-house roles, such as General Counsel of a hospital, where strategic business advice is just as important as legal counsel. This can translate to a 10-15% salary premium over time.
- Professional Certifications:
- Certified in Healthcare Compliance (CHC): Offered by the Compliance Certification Board (CCB), the CHC is the gold standard for compliance professionals. For attorneys focused on the regulatory side of healthcare law, having this certification is a clear signal of expertise in designing and managing effective compliance programs. It is often a preferred or even required credential for in-house compliance counsel roles and can be a significant factor in salary negotiations.
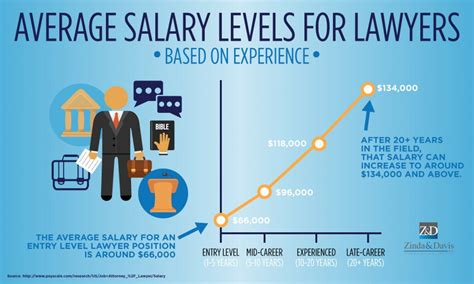
### 2. Years of Experience: The Climb to Mastery
As with most professions, experience is arguably the single most powerful determinant of salary. The legal field, in particular, rewards a demonstrated history of successful outcomes and deep-seated knowledge that can only be gained over time.
- Associate Years (1-8): This is the training and growth phase.
- Junior Associates (Years 1-3): Salary: $90,000 - $160,000. The primary focus is on learning the ropes. They perform foundational legal tasks and their value is in their ability to learn quickly and support senior lawyers efficiently. In BigLaw, this starts much higher, around $225,000 in 2024.
- Mid-Level Associates (Years 4-6): Salary: $160,000 - $240,000. These attorneys have developed a solid knowledge base. They are trusted to manage significant aspects of a case or transaction with less supervision. They begin to have more direct client interaction and are seen as reliable workhorses. Their salary increases reflect their growing autonomy and efficiency.
- Senior Associates (Years 7-8): Salary: $220,000 - $290,000+. On the cusp of making partner or moving to a senior in-house role, these attorneys are highly skilled specialists. They manage junior associates, take the lead on complex matters, and may start to build relationships that could turn into future business. Their compensation reflects their near-mastery of their niche.
- Counsel and Partner Years (9+): This is the leadership and business-generation phase.
- Counsel / Senior Counsel (Years 9-15): Salary: $250,000 - $350,000. This title is often used for highly experienced attorneys who are valuable experts but are not on the equity partner track. In an in-house setting, it denotes a senior legal advisor. Their value is in their deep subject matter expertise.
- Partner (Equity and Non-Equity): Salary: $350,000 - $1,000,000+. This is the pinnacle of the law firm model. Non-equity partners are salaried but have a partner title and higher bonus potential. Equity partners are owners of the firm, and their compensation is a share of profits. Their value is not just in their legal skill, but in their ability to bring in millions of dollars of business (their "book of business"). This is where salaries become astronomical.
### 3. Geographic Location: Where You Work Matters
The adage "location, location, location" holds as true for legal salaries as it does for real estate. The cost of living and the concentration of major healthcare corporations and top law firms create significant geographic disparities in pay.
- Top-Tier Metropolitan Areas: Major legal and business hubs offer the highest salaries, often 20-40% above the national average. These cities are home to the headquarters of large health systems, pharmaceutical companies, and the most profitable law firms.
- Washington, D.C.: The epicenter of federal regulation. Home to the Department of Health and Human Services (HHS), CMS, and the FDA, D.C. has an enormous concentration of regulatory healthcare lawyers. Salaries here are among the highest in the nation. (Average: ~$195,000)
- New York, NY: A hub for finance and major corporate transactions, leading to high-paying work in healthcare M&A and private equity deals. (Average: ~$190,000)
- San Francisco / Silicon Valley, CA: The nexus of technology and healthcare (HealthTech), with a high demand for lawyers specializing in data privacy (HIPAA), digital health, and venture capital financing. (Average: ~$205,000)
- Boston, MA & Chicago, IL: Major centers for biotechnology, academic medical centers, and large insurance companies. (Average: ~$180,000)
- Mid-Tier and Lower-Paying Areas: Salaries in smaller cities and rural areas are typically lower, reflecting a lower cost of living and a different client base (e.g., community hospitals instead of multinational corporations). States in the Southeast and Midwest (excluding major hubs like Chicago) often fall below the national average. However, the purchasing power of a $130,000 salary in a city like Omaha, Nebraska, may be equivalent to or greater than a $180,000 salary in New York City.
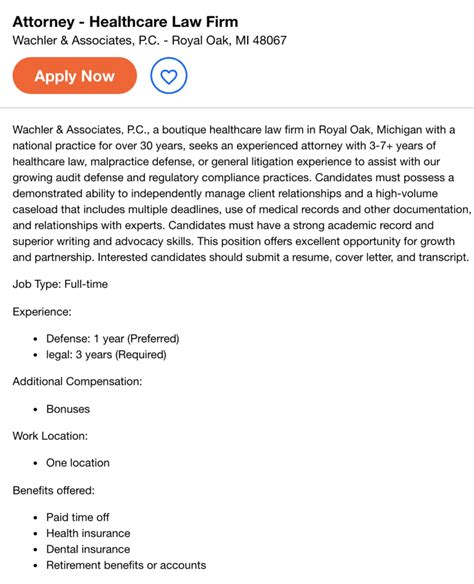
### 4. Company Type & Size: Who You Work For
The nature of your employer is a massive factor in your compensation structure and ceiling.
- Large Law Firms ("BigLaw"): These firms (typically 500+ attorneys) represent the largest and most sophisticated clients and, as a result, offer the highest salaries and bonuses, especially for associates. The trade-off is intense pressure, extremely high billable hour requirements, and an "up or out" culture.
- Boutique Health Law Firms: Smaller firms that exclusively practice health law can also be very lucrative. While their starting salaries might not match BigLaw, successful partners in top boutique firms can earn just as much, often with a better lifestyle and more hands-on experience early in one's career.
- In-House Counsel (Healthcare System/Corporation): Working directly for a hospital, pharmaceutical company, or insurer offers a different compensation model. Base salaries are strong and competitive with mid-to-large firms. While bonuses are smaller, the overall package often includes better work-life balance, greater job stability, and, for senior roles, the potential for stock options or long-term incentive plans. The salary ceiling is typically the General Counsel or Chief Legal Officer role, which can be extremely well-compensated at large organizations.
- Government: Attorneys working for federal agencies like HHS or state attorneys general offices will have the lowest starting salaries. The government's pay scales are public and rigid. For example, a new attorney might start on the GS-11 or GS-12 scale, earning around $75,000 - $90,000. However, the trade-off is significant: unparalleled work-life balance, excellent job security, federal benefits, and often, eligibility for Public Service Loan Forgiveness (PSLF). The experience gained is also highly valuable and can lead to a lucrative private sector job later.
- Non-Profit/Academic Medical Centers: These roles offer salaries that typically fall between government and in-house corporate positions. The work is mission-driven, and the benefits can be excellent, but the salary ceiling is generally lower than in the for-profit sector.
### 5. Area of Specialization: Your Niche Dictates Your Value
Within the broad field of "health law," certain sub-specialties are more complex, in higher demand, and thus, more lucrative.
- High-Paying Specializations:
- Healthcare M&A and Private Equity: Transactional attorneys who facilitate multi-billion dollar deals for health systems and private equity funds are at the top of the pay scale. Their work directly generates massive revenue and requires sophisticated financial and legal expertise.
- Government Investigations & White-Collar Defense: Defending healthcare companies against fraud and abuse allegations from the DOJ can involve massive financial stakes. Expert litigators in this area command premium rates for their ability to navigate these high-risk investigations.
- Pharmaceutical and Medical Device Law: Advising on the full lifecycle of a drug or device—from FDA approval to patent litigation and marketing compliance—is a highly specialized and well-compensated field.
- Standard to High-Paying Specializations:
- Regulatory Compliance (Stark Law, AKS, HIPAA): This is the core of health law. While perhaps less glamorous than M&A, deep expertise here is always in demand and essential for any healthcare organization. Top compliance advisors are very well-paid.
- Telehealth and Digital Health Law: An emerging and rapidly growing field. Attorneys who can advise on the complex web of state licensing, privacy, and reimbursement rules for virtual care are becoming increasingly valuable.
- Standard Paying Specializations:
- Medical Malpractice Defense: While essential, this litigation practice is often handled by insurance defense firms where billing rates and, consequently, salaries are more constrained compared to corporate-focused practices.
- General Hospital Operations: Advising on day-to-day issues like patient consent, bioethics, and staff privileging is critical but may not command the same premium as high-stakes transactional or investigative work.
### 6. In-Demand Skills: The Value-Adds
Beyond your formal title and specialization, certain cross-cutting skills can make you a more valuable asset and justify higher pay.
- Data Privacy and Cybersecurity Expertise: With the rise of electronic health records and digital health, understanding the nuances of HIPAA, GDPR (if applicable), and state data breach laws is no longer optional. Attorneys who can lead an organization through a data breach response are invaluable.
- Project Management: The ability to manage a complex transaction or litigation from start to finish, coordinating with multiple stakeholders and keeping everything on budget and on time, is a skill that separates top performers from the rest.
- Business Acumen: The best lawyers don't just spot legal issues; they understand the business implications of their advice. Being able to speak the language of finance and strategy with C-suite executives makes you a true partner to the business, not just a legal gatekeeper.
- Client Development: In a law firm setting, the ability to bring in new clients is the single most important skill for long-term, high-level financial success. This involves networking, marketing, and building a reputation as a thought leader in the industry.
Job Outlook and Career Growth

For those investing the significant time and resources required to become a healthcare attorney, the long-term career prospects are a critical consideration. The outlook is exceptionally positive, driven by powerful and sustained macro-level trends in the U.S. healthcare landscape.
The U.S. Bureau of Labor Statistics (BLS), in its Occupational Outlook Handbook, projects that employment for all lawyers will grow by 8 percent from 2022 to 2032, which is much faster than the average for all occupations. However, this general statistic likely understates the specific demand for healthcare attorneys. The healthcare sector is one of the fastest-growing segments of the U.S. economy, and legal services are an integral part of that expansion. As the industry grows in size and complexity, the need for specialized legal guidance grows in lockstep.
Several key trends are fueling this robust demand and shaping the future of the profession:
1. An Aging Population and Chronic Disease: The demographic shift of the baby boomer generation entering retirement age is placing unprecedented demand on the healthcare system. This translates to more hospitals, more long-term care facilities, more medical services, and consequently, more legal work related to Medicare, facility licensing, M&A, and patient care regulations.
2. The Explosion of Telehealth and Digital Health: The COVID-19 pandemic acted as a massive accelerator for virtual care. This has created a new frontier of legal questions. Healthcare attorneys are now essential for advising on:
- State-by-State Licensing: Navigating the patchwork of laws governing whether a physician in one state can treat a patient in another.
- Reimbursement Policies: Understanding and lobbying for favorable payment policies for virtual services from Medicare, Medicaid, and private insurers.
- Data Privacy and Security: Ensuring that telehealth platforms are HIPAA-compliant and secure from cyber threats.
- Standard of Care: Defining the legal standards for care delivered virtually versus in person.
This is a high-growth niche that will require legal expertise for decades to come.
3. Continued Regulatory Complexity and Enforcement: The government shows no signs of simplifying healthcare regulation. On the contrary, areas like price transparency, data interoperability, and fraud and abuse enforcement are becoming more complex. The Office of Inspector General (OIG) and the Department of Justice (DOJ) are increasingly using sophisticated data analytics to identify potential fraud, leading to more investigations and a greater need for defense counsel. Companies need savvy lawyers to create proactive compliance programs to stay out of trouble and to defend them when they are targeted.
**4. Industry