Are you driven by a desire to make a tangible impact on people's lives, but feel your talents lie more in leadership, strategy, and operations than in direct clinical care? Do you envision yourself at the helm of a hospital, a thriving clinic, or a cutting-edge healthcare system, steering it toward efficiency, quality, and financial stability? If so, a career in Health Administration, supercharged by a Master of Health Administration (MHA), might be your calling. This path isn't just about leadership; it's about becoming the crucial backbone of the healthcare industry, a field that is both profoundly meaningful and financially rewarding, with median salaries comfortably exceeding $100,000 annually for experienced professionals.
I once spent time shadowing a hospital administrator during a particularly chaotic winter surge. Amid the controlled frenzy of the emergency department, she wasn't treating patients, but she was orchestrating the entire response—rerouting staff, securing extra beds from other units, and communicating with department heads to ensure the flow of patients was managed safely. It was a masterclass in leadership, and it cemented my understanding that for every great clinician saving a life, there's a great administrator behind the scenes making it all possible.
This guide is designed to be your definitive resource, a comprehensive map to navigate the landscape of a career in Health Administration. We will dissect every facet of the masters in health administration salary, explore the factors that can elevate your earnings, and lay out a clear, actionable plan for you to launch your own successful career.
### Table of Contents
- [What Does a Health Administrator Do?](#what-does-a-health-administrator-do)
- [Average masters in health administration salary Salary: A Deep Dive](#average-salary-a-deep-dive)
- [Key Factors That Influence Your Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth in Health Administration](#job-outlook-and-career-growth)
- [How to Become a Health Administrator: Your Step-by-Step Guide](#how-to-get-started)
- [Is a Career in Health Administration Right for You?](#conclusion)
What Does a Health Administrator Do?
At its core, a Health Administrator, often titled a Medical and Health Services Manager, is the strategic leader and operational manager of a healthcare organization or a specific department within it. Think of them as the CEO, COO, or general manager of their domain. While physicians, nurses, and technicians focus on patient care, the health administrator focuses on creating the optimal environment for that care to be delivered effectively, efficiently, and sustainably.
Their work is a complex blend of business acumen, leadership, and a deep understanding of the healthcare ecosystem. They are the conductors of a complex orchestra, ensuring that all sections—from finance and human resources to clinical departments and technology—play in harmony to achieve the organization's mission.
Core Responsibilities and Daily Tasks:
A health administrator's duties are vast and varied, but they generally fall into several key categories:
- Strategic Planning and Development: Setting goals and objectives for the department or organization. They analyze industry trends, competitor activities, and patient demographics to plot a course for future growth and service improvement.
- Financial Management: This is a cornerstone of the role. Administrators are responsible for preparing and managing budgets, monitoring financial performance, optimizing revenue cycles (billing and collections), and ensuring the organization's financial health.
- Operational Oversight: Managing the day-to-day functions of their facility or department. This includes everything from staff scheduling and supply chain management to ensuring patient flow is smooth and wait times are minimized.
- Human Resources Management: Hiring, training, and evaluating staff. They work to create a positive work environment, manage employee relations, and ensure adequate staffing levels to meet patient demand.
- Regulatory Compliance and Quality Assurance: Healthcare is one of the most heavily regulated industries. Administrators must ensure their organization complies with all laws and regulations (e.g., HIPAA, Joint Commission standards). They also lead initiatives to improve patient safety and the quality of care.
- Technology Integration: Overseeing the implementation and use of health information technology, such as Electronic Health Records (EHRs), to improve efficiency and patient outcomes.
---
### A Day in the Life: Director of Operations, Mid-Sized Community Hospital
To make this tangible, let's follow "Alex," a Health Administrator with an MHA who serves as the Director of Operations.
- 7:30 AM: Alex arrives and reviews the overnight hospital census report and any incident reports. He notes a spike in admissions in the orthopedic unit and a staffing call-out in the ICU.
- 8:00 AM: Morning leadership "huddle" with the Chief Nursing Officer, Chief Financial Officer, and other key directors. They discuss the census, staffing issues, and any pressing patient safety concerns. Alex is tasked with finding a solution for the orthopedic bed shortage.
- 9:00 AM: Meeting with the manager of the orthopedic unit and the discharge planning team. They strategize on how to safely expedite the discharge of patients ready to go home, freeing up beds for new admissions.
- 11:00 AM: Budget review session with the finance department. They analyze the Q3 budget variance for surgical services, identifying areas of overspending in supply costs. Alex commits to working with surgeons to evaluate lower-cost, clinically equivalent supplies.
- 1:00 PM: Lunch while reviewing proposals for a new patient scheduling software. He's looking for a system that can reduce wait times and integrate with their current EHR.
- 2:30 PM: Sits in on the hospital's Quality Improvement Committee meeting. Today's topic is reducing hospital-acquired infections. Alex contributes from an operational perspective, discussing workflow changes that could improve sterile procedures.
- 4:00 PM: Walks the floors. Alex believes in "management by walking around." He checks in with staff in the emergency department, listens to their concerns, and observes patient flow firsthand.
- 5:30 PM: Back at his desk, Alex responds to emails, signs off on purchase orders, and drafts a memo outlining the new discharge protocol for the orthopedic unit. He reviews his calendar for the next day before heading home.
This example illustrates the dynamic, problem-solving nature of the role. It requires a seamless shift between high-level strategy and granular, on-the-ground operational detail.
Average masters in health administration salary Salary: A Deep Dive
Now for the central question: What can you expect to earn with a Master's in Health Administration? The financial outlook is exceptionally strong, reflecting the high level of responsibility and specialized knowledge required for the role. An MHA is a significant investment, but the return on that investment, in terms of salary potential, is substantial and well-documented.
It's crucial to understand that "salary" is more than just a base number; it's a total compensation package. However, let's start with the foundational data from the most reliable sources.
National Average and Salary Range
The most authoritative source for this data is the U.S. Bureau of Labor Statistics (BLS), which classifies these professionals under "Medical and Health Services Managers."
- Median Annual Salary: According to the BLS's May 2022 data (the most recent comprehensive report), the median annual wage for medical and health services managers was $104,830. This means half of all managers earned more than this amount, and half earned less.
- Salary Range: The BLS also provides a range to show the full spectrum of earning potential:
- The lowest 10 percent earned less than $64,100. These are typically entry-level positions or roles in smaller, less-funded facilities.
- The highest 10 percent earned more than $209,990. These are the senior executive roles (e.g., C-suite executives like CEO, COO) in large, complex health systems.
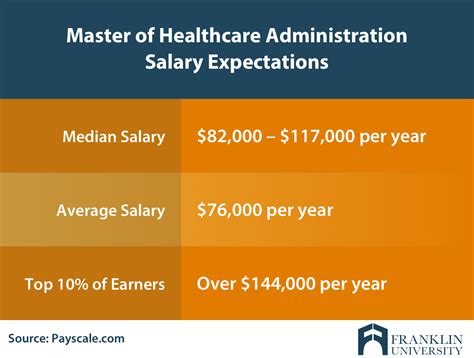
Reputable salary aggregation websites provide similar, often more granular, real-time data based on user-submitted profiles. As of late 2023/early 2024:
- Salary.com: Reports the median salary for a Healthcare Administration Manager in the United States to be around $120,550, with a typical range falling between $105,270 and $137,360.
- Payscale.com: Shows the average salary for a professional with a Master of Health Administration (MHA) degree is approximately $98,000 per year. This figure often includes professionals with varying levels of experience, which can pull the average down slightly compared to manager-specific roles.
- Glassdoor: Lists the average base pay for a "Healthcare Administrator" at $84,047 per year, but this title can be broad. For a more senior "Hospital Administrator," the average climbs to $121,911.
What does this tell us? A six-figure salary is not just an aspiration but a very realistic median benchmark for professionals in this field, particularly a few years after earning an MHA.
---
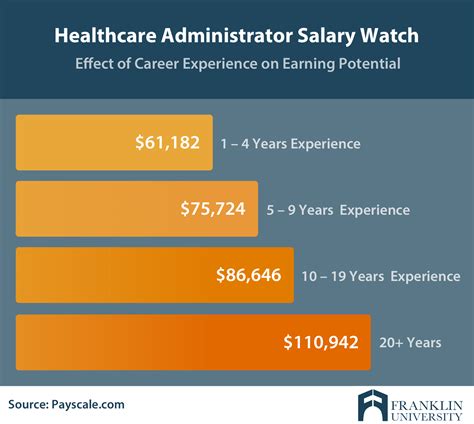
### Salary by Experience Level
Your salary will grow significantly as you accumulate experience and take on greater responsibility. An MHA degree provides the educational foundation, but your hands-on experience is what translates that knowledge into tangible value for an employer, who in turn compensates you for it.
Here is a typical salary progression you can expect throughout your career, compiled from sources like Payscale and Salary.com.
| Experience Level | Typical Timeframe | Common Job Titles | Typical Salary Range (Annual) |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-2 Years | Administrative Fellow, Project Coordinator, Department Supervisor, Practice Manager (Small Clinic) | $65,000 - $85,000 |
| Mid-Career | 3-8 Years | Department Manager, Director of Operations, Service Line Director, Practice Administrator (Large Group) | $85,000 - $130,000 |
| Senior-Level | 9-15 Years | Vice President (VP) of Operations, Associate Administrator, Senior Director, Chief Operating Officer (Small Hospital) | $130,000 - $180,000+ |
| Executive-Level| 15+ Years | Chief Operating Officer (COO), Chief Executive Officer (CEO), Chief Strategy Officer (CSO) in large hospitals or health systems | $180,000 - $300,000+ |
*Note: These are national averages. Your specific salary will be heavily influenced by the factors discussed in the next section.*
### Beyond the Base Salary: Understanding Total Compensation
Your annual salary is only one part of the equation. Health administration roles, especially at the manager level and above, often come with robust compensation packages that significantly increase your overall earnings.
- Annual Bonuses: These are extremely common and are typically tied to performance metrics. Bonuses can be based on your individual performance (meeting budget goals), your department's performance (improving patient satisfaction scores), and the organization's overall performance (achieving profitability targets). A bonus can range from 5% to 25% or more of your base salary.
- Profit Sharing: In for-profit healthcare systems (e.g., HCA Healthcare, Tenet Healthcare), managers and executives may be eligible for a share of the company's profits, providing a direct incentive to improve the organization's financial health.
- Retirement Plans: This is a critical component of long-term wealth building. Most non-profit healthcare organizations offer a 403(b) plan, while for-profits offer a 401(k). The key is the employer match. A typical match might be 50% of your contributions up to 6% of your salary, which is essentially an instant, guaranteed return on your investment.
- Health and Wellness Benefits: As you would expect from a healthcare employer, these benefits are usually excellent. This includes comprehensive medical, dental, and vision insurance with relatively low premiums and deductibles.
- Paid Time Off (PTO): Leadership roles generally come with generous vacation, sick, and personal day allowances, often starting at 4 weeks per year and increasing with seniority.
- Tuition Reimbursement & Professional Development: Many healthcare organizations invest in their leaders by providing funds for ongoing education, attending industry conferences (like the ACHE Congress), or pursuing advanced certifications.
- Relocation Assistance: For senior-level roles, it's common for organizations to offer a relocation package to attract top talent from other regions.
When evaluating a job offer, it's essential to look at this total compensation picture. A role with a slightly lower base salary but an exceptional bonus structure and a generous 401(k) match could be more lucrative in the long run.
Key Factors That Influence Your masters in health administration salary
While the national averages provide a great starting point, your individual salary is determined by a confluence of factors. Understanding these variables is the key to maximizing your earning potential. An MHA is your ticket to the game, but how you play the game—leveraging your background, skills, and choices—determines your score.
### 1. Level and Quality of Your Education
While this article is centered on the MHA, the specifics of your education matter.
- MHA vs. MBA vs. MPH:
- MHA (Master of Health Administration): The most direct and specialized degree. Its curriculum is tailored specifically to the business of healthcare.
- MBA with a Healthcare Concentration: An excellent alternative, particularly for those who want to blend deep business principles (finance, marketing, strategy) with healthcare applications. This can be highly valuable for roles in large corporate health systems, consulting, or the pharmaceutical industry.
- MPH (Master of Public Health): This degree focuses more on population health, epidemiology, and policy. It's ideal for roles in government (CDC, local health departments) or non-profits focused on community health, and salaries may be slightly lower than in a traditional hospital administration track.
- Program Accreditation (CAHME): The gold standard for MHA programs is accreditation from the Commission on Accreditation of Healthcare Management Education (CAHME). Graduating from a CAHME-accredited program signals to employers that you have received a rigorous, high-quality education that meets industry standards. This can be a significant advantage, particularly for prestigious administrative fellowships and your first job post-graduation.
- Advanced Certifications: Post-MHA, pursuing board certification is a powerful way to increase your authority and salary. The most prestigious is the FACHE (Fellow of the American College of Healthcare Executives). To become a Fellow, you must have a master's degree, healthcare management experience, pass a comprehensive exam, and demonstrate a commitment to professional development. Earning the FACHE credential is a clear marker of expertise and is often a prerequisite for C-suite roles, commanding a significant salary premium.
### 2. Years and Type of Experience
As shown in the salary progression table, experience is arguably the single most significant factor in your salary growth.
- The Administrative Fellowship: Many top MHA graduates complete a one-to-two-year administrative fellowship. This is a highly competitive, post-graduate residency where you rotate through various departments of a hospital or health system, working directly with senior executives. While the fellowship salary itself is modest (typically $60,000 - $75,000), it is an unparalleled career accelerator. Fellows often land manager-level positions immediately upon completion, bypassing several years of entry-level work.
- Clinical Background: While not required, having a prior clinical background (e.g., as a nurse, physical therapist, or technician) before pursuing an MHA can be a major asset. You bring an intrinsic understanding of clinical workflows and a credibility with clinical staff that is hard to replicate. This can lead to specialized leadership roles (e.g., Director of Nursing, Director of Rehabilitative Services) that command higher salaries.
- Trajectory and Scope of Responsibility: Your salary isn't just about years worked; it's about the scope of responsibility you've earned. An administrator who has spent 10 years successfully managing a 15-person department will earn less than one who has spent 10 years progressively moving up to oversee a 200-person service line with a $50 million budget. Proactively seeking projects, leading initiatives, and demonstrating quantifiable results (e.g., "reduced operating costs by 12%") is how you build the case for promotion and higher pay.
### 3. Geographic Location
Where you work has a massive impact on your paycheck, largely due to variations in the cost of living and the concentration of large, high-paying healthcare employers.
Top-Paying Metropolitan Areas for Medical and Health Services Managers (Source: BLS, May 2022):
1. San Jose-Sunnyvale-Santa Clara, CA: Annual Mean Wage: $184,330
2. Vallejo-Fairfield, CA: Annual Mean Wage: $174,050
3. San Francisco-Oakland-Hayward, CA: Annual Mean Wage: $173,080
4. Trenton, NJ: Annual Mean Wage: $165,830
5. New York-Newark-Jersey City, NY-NJ-PA: Annual Mean Wage: $164,570
Top-Paying States:
1. New York: $155,590
2. District of Columbia: $151,190
3. California: $148,840
4. Massachusetts: $145,550
5. New Jersey: $143,240
Conversely, states and rural areas with a lower cost of living and smaller healthcare markets will typically offer lower salaries. For example, states like Mississippi, Alabama, and Arkansas tend to have median salaries closer to or below the national median.
The Strategy: While it's tempting to chase the highest absolute salary, you must weigh it against the cost of living. A $140,000 salary in San Francisco may leave you with less disposable income than a $110,000 salary in a city like Charlotte, NC, or Columbus, OH.
### 4. Work Setting and Organization Type
The type and size of the organization you work for is another critical salary determinant.
| Work Setting | Description | Typical Salary Range (Median) | Why? |
| :--- | :--- | :--- | :--- |
| Hospitals (State, Local, & Private) | The largest employer of health administrators. Roles range from department manager to CEO. | $119,450 (BLS Median) | Large, complex operations with significant budgets and revenue. Pay is commensurate with the high level of responsibility. |
| Ambulatory Healthcare Services | Outpatient centers, physician group practices, surgery centers. | $99,540 (BLS Median) | Operations are typically smaller in scale than hospitals, but large, multi-site physician practices can be very lucrative. |
| Government | Federal (e.g., VA Hospitals, Dept. of Health), state, and local health departments. | Varies Greatly | Federal roles, particularly within the VA system, are often competitive with private sector pay and have excellent benefits. State/local jobs may pay less but offer great stability. |
| Nursing & Residential Care Facilities | Skilled nursing facilities (SNFs), assisted living communities. | $94,480 (BLS Median) | These facilities often operate on thinner margins than hospitals, which can be reflected in salaries, though top administrators of large chains are well-compensated. |
| Corporate/Consulting/Insurance | Roles within large health insurance companies, pharmaceutical/biotech firms, or healthcare consulting firms. | Often $150,000+ | These for-profit entities highly value business acumen. Roles in strategy, business development, and consulting can be among the highest paying in the industry. |
Size Matters: Working for a massive, nationally recognized health system like Mayo Clinic, Cleveland Clinic, or HCA Healthcare will generally offer higher salary potential and more room for advancement than a small, independent critical access hospital in a rural area.
### 5. Area of Specialization
Within health administration, you can specialize in functions that are in particularly high demand, leading to higher earning potential.
- Health Informatics / Data Analytics: This is arguably the hottest specialization today. Administrators who can manage EHR systems, leverage clinical and financial data to drive decisions, and understand healthcare IT are invaluable. They command a premium salary because they help organizations unlock efficiency and improve quality through technology.
- Finance / Revenue Cycle Management: Experts who can optimize the complex process of billing, coding, and collections are always in demand. A Director of Revenue Cycle with a proven track record of increasing collections can have a direct, positive impact on the bottom line, and they are compensated accordingly.
- Strategy and Business Development: These professionals work on mergers and acquisitions, service line expansion, and forging partnerships. Their work directly contributes to the organization's growth and market position, making it a high-stakes, high-reward field.
- Quality and Process Improvement: Administrators trained in methodologies like Lean Six Sigma who can lead initiatives to improve patient safety, reduce errors, and enhance efficiency are critical for meeting regulatory standards and succeeding in a value-based care environment.
### 6. In-Demand Skills
Beyond your formal title, the specific skills you cultivate can make you a more attractive and highly paid candidate.
- Hard Skills:
- Financial Acumen: The ability to read, analyze, and interpret financial statements, create budgets, and perform ROI analysis.
- Data Analysis: Proficiency with tools like Excel, SQL, and data visualization software (Tableau, Power BI). The ability to turn raw data into actionable insights is a superpower.
- Project Management: Formal knowledge of project management principles (PMP certification is a plus) to lead complex initiatives like a new building wing or an EHR implementation.
- Healthcare Law and Compliance: Deep knowledge of HIPAA, Stark Law, Anti-Kickback statutes, and payer regulations.
- Soft Skills (Power Skills):
- Leadership: The ability to inspire, motivate, and guide teams of diverse professionals, including strong-willed physicians.
- Communication: Exceptional written and verbal communication skills are non-negotiable. You must be able to present complex information clearly to everyone from the board of directors to frontline staff.
- Strategic Thinking: The ability to see the big picture, anticipate future trends, and position your organization for long-term success.
- Negotiation and Conflict Resolution: Whether negotiating with a vendor for a better price or mediating a dispute between two department heads, these skills are used daily.
Job Outlook and Career Growth in Health Administration

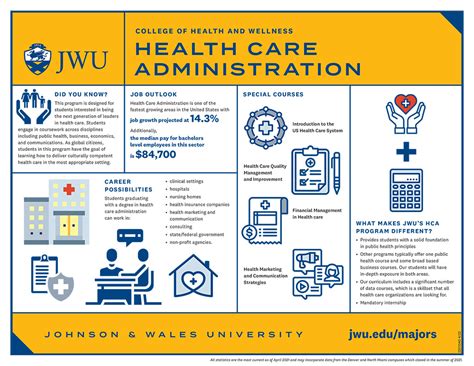
If you're investing the time and money into an MHA, you want to be sure you're entering a growing field. The data on this is unequivocally positive. The career outlook for health administrators is not just good; it's one of the strongest in the entire U.S. economy.
Explosive Job Growth Projections
According to the U.S. Bureau of Labor Statistics' Occupational Outlook Handbook, employment of medical and health services managers is projected to grow 28 percent from 2022 to 2032.
To put that in perspective, this is much faster than the average for all occupations, which is just 3 percent.
The BLS projects that this will result in about 54,700 openings for medical and health services managers each year, on average, over the decade. These openings are expected to result from both the creation of new jobs and the need to replace workers who transfer to different occupations or exit the labor force, such as to retire.
Why is the Demand So High?
Several powerful, long-term trends are fueling this remarkable growth:
1. The Aging Population: The massive Baby Boomer generation is aging and will require significantly more medical services. This increases demand across the entire healthcare spectrum—from hospitals and physician offices to nursing homes and home healthcare services. All of these expanding services require skilled administrators to manage them.
2. The Shift to Value-Based Care: The healthcare industry is slowly moving away from a fee-for-service model (where providers are paid for the quantity of services) to a value-based care model (where they are paid for quality and outcomes). This transition is incredibly complex and requires administrators who can analyze data, redesign care processes, and manage population health to improve outcomes while controlling costs.
3. Advances in Technology and Data: The proliferation of Electronic Health Records (EHRs) and other health IT has created a mountain of data. Healthcare organizations need leaders who are savvy enough to use this data to improve clinical and financial performance. This creates demand for administrators with skills in informatics and analytics.
4. Increasingly Complex Regulatory Environment: As mentioned, healthcare is heavily regulated. Keeping up with changes in healthcare law, insurance regulations, and compliance standards requires dedicated and knowledgeable managers.
Future Challenges and Staying Ahead of the Curve
While the outlook is bright, the field is not without its challenges. The successful administrator of tomorrow will need to be agile and forward-thinking.
- Rising Costs and Financial Pressures: The cost of healthcare continues to rise, and organizations face constant pressure to do more with less. Administrators are on the front lines of this battle, constantly seeking efficiencies without sacrificing quality.
- Workforce Shortages: Shortages of nurses, physicians, and other clinical staff are a persistent problem. Administrators must be creative in their recruitment, retention, and staff engagement strategies.
- Cybersecurity Threats: With all patient data now digitized, protecting it from