Introduction

Have you ever felt the calling to do more in your nursing career? To move beyond the bedside and into a role with greater autonomy, deeper patient relationships, and the authority to diagnose, treat, and prescribe? For many ambitious Registered Nurses, the path leads to becoming a Nurse Practitioner (NP)—a career that is not only profoundly rewarding but also financially lucrative. With a national median salary well into the six figures, the NP role represents a pinnacle of clinical practice and professional achievement. The demand for these advanced practice providers is skyrocketing, creating a landscape of unprecedented opportunity.
As a career analyst who has guided countless healthcare professionals through their career transitions, I've seen firsthand the transformative power of this path. I once worked with a seasoned RN who, despite loving her work, felt she had hit a professional and financial ceiling. She took the leap, invested in her education, and became a Family Nurse Practitioner. Within two years, she was not only earning nearly double her previous salary but was also running her own panel of patients, describing her work as "the reason I went into nursing in the first place." Her story is not an exception; it's increasingly the norm in this dynamic field.
This guide is designed to be your definitive resource for understanding every facet of a Nurse Practitioner's salary and career. We will dissect national averages, explore the key factors that can dramatically increase your earning potential, and lay out a clear, step-by-step roadmap to get you there. Whether you are a nursing student, a practicing RN, or simply exploring high-impact careers in healthcare, this article will provide the data-driven insights and expert advice you need to make an informed decision.
### Table of Contents
- [What Does a Nurse Practitioner Do?](#what-is-an-np)
- [Average Nurse Practitioner Salary: A Deep Dive](#salary-deep-dive)
- [Key Factors That Influence Your Salary](#key-factors)
- [Job Outlook and Career Growth](#job-outlook)
- [How to Get Started in This Career](#how-to-start)
- [Conclusion](#conclusion)
---
What Does a Nurse Practitioner Do?
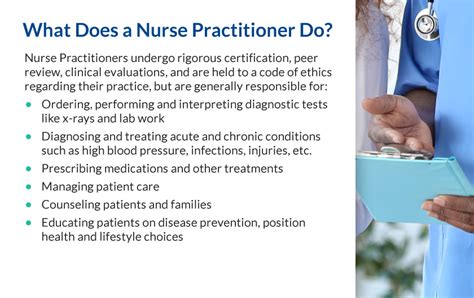
A Nurse Practitioner is an Advanced Practice Registered Nurse (APRN) who has completed graduate-level education (either a Master of Science in Nursing or a Doctor of Nursing Practice) and obtained national board certification in a specific patient population specialty. They are trained, licensed, and equipped to provide a significant level of patient care, often serving as a primary or specialty care provider.
Unlike an RN, whose practice is focused on carrying out patient care plans, an NP is responsible for *creating* those plans. They blend the clinical expertise of a physician with the patient-centered, holistic approach of nursing. This unique combination allows them to manage a patient's overall health, focusing on wellness and disease prevention just as much as treating acute and chronic illnesses.
The scope of practice for NPs varies by state, which is a critical concept to understand. States fall into one of three categories:
1. Full Practice Authority: In these states (like Washington, Oregon, and Arizona), NPs can evaluate patients, diagnose, order and interpret tests, initiate and manage treatments, and prescribe medications without physician oversight. They can also establish their own independent practices.
2. Reduced Practice: In these states, NPs are limited in at least one area of their practice. They may need a career-long collaborative agreement with a physician to provide patient care or have limits on their prescriptive authority.
3. Restricted Practice: In these states, NPs require direct physician supervision, delegation, or team management to provide patient care. This is the most restrictive environment.
Core Responsibilities and Daily Tasks
Regardless of the state, the core duties of an NP are comprehensive. Their daily workflow is a dynamic mix of clinical, administrative, and educational tasks.
- Patient Assessment: Performing comprehensive health histories and detailed physical examinations.
- Diagnosis: Diagnosing and treating acute health problems (e.g., infections, injuries) and chronic diseases (e.g., diabetes, hypertension).
- Ordering & Interpreting Tests: Ordering diagnostic tests like lab work, X-rays, and MRIs, and then interpreting the results to inform treatment.
- Developing Treatment Plans: Creating evidence-based plans of care that may include medication, therapy, lifestyle changes, and referrals to other specialists.
- Prescribing Medications: Prescribing pharmaceuticals and other treatments within their scope of practice.
- Patient Education: Counseling and educating patients and their families on disease prevention, health maintenance, and positive lifestyle choices.
- Procedures: Performing common procedures relevant to their specialty, such as suturing, biopsies, and joint injections.
- Collaboration: Working closely with physicians, nurses, social workers, and other healthcare professionals to ensure coordinated patient care.
### A Day in the Life: Dr. Marcus Chen, DNP, FNP-BC
To make this tangible, let's follow a hypothetical "day in the life" of a Family Nurse Practitioner (FNP) working in a busy outpatient primary care clinic.
- 8:00 AM: Marcus arrives at the clinic, reviews his schedule for the day, and checks lab results and specialist reports that came in overnight. He flags a few for follow-up calls.
- 8:30 AM - 12:00 PM: Patient appointments begin. He sees a 45-year-old for hypertension management, adjusting his medication. Next, he diagnoses a child with strep throat and prescribes antibiotics. He then conducts a "Welcome to Medicare" wellness visit for a new 65-year-old patient, discussing preventative screenings and health goals. He also sutures a small laceration for a walk-in patient.
- 12:00 PM - 1:00 PM: Lunch break, during which he quickly catches up on charting and returns a few patient phone calls regarding prescription refills.
- 1:00 PM - 4:30 PM: The afternoon is filled with more appointments, including a well-woman exam, a follow-up for a patient with recently diagnosed Type 2 diabetes, and a teenager with sports-related knee pain. Between patients, he consults with the on-site cardiologist about a complex patient case.
- 4:30 PM - 5:30 PM: Marcus finishes his patient notes in the Electronic Health Record (EHR), signs off on prescription refill requests, and responds to patient messages in the online portal. He prepares a referral for the patient with knee pain to see an orthopedic specialist. He leaves the clinic having managed the health and wellness of nearly 20 individuals, acting as their trusted primary provider.
---
Average Nurse Practitioner Salary: A Deep Dive

The financial compensation for a Nurse Practitioner is a significant draw, reflecting the high level of education, responsibility, and demand for the role. Salary figures consistently place NPs among the top earners in healthcare and across all professions.
According to the most recent data from the U.S. Bureau of Labor Statistics (BLS) Occupational Outlook Handbook, the median annual wage for Nurse Practitioners was $128,490 as of May 2023. This is the midpoint, meaning half of all NPs earned more than this, and half earned less.
However, the full picture is much wider. The BLS also reports the salary range:
- Lowest 10% earned: Less than $94,930
- Highest 10% earned: More than $174,990
Professional organizations and salary aggregators provide further granularity, often showing even higher potential earnings when bonuses and other compensation are included.
- The American Association of Nurse Practitioners (AANP) 2020 National NP Sample Survey reported a median total income of $117,000 for full-time NPs (including salary and bonuses). This number has undoubtedly grown since.
- Salary.com, as of late 2024, reports the median NP salary in the U.S. to be $126,280, with a typical range falling between $117,190 and $137,110.
- Glassdoor places the average total pay for an NP at $144,233 per year, combining a base salary of around $124,000 with additional pay (bonuses, profit sharing) of approximately $20,000.
### Salary by Years of Experience
Like any profession, experience is a primary driver of salary growth. As an NP gains clinical confidence, efficiency, and a reputation for excellent patient outcomes, their value to an employer increases substantially.
Here is a typical salary progression based on synthesized data from Payscale and Salary.com:
| Experience Level | Typical Years of Experience | Estimated Annual Salary Range | Description |
| :--- | :--- | :--- | :--- |
| Entry-Level Nurse Practitioner | 0-1 years | $100,000 - $118,000 | A new graduate, often working with mentorship. Focus is on building clinical skills and patient management efficiency. |
| Mid-Career Nurse Practitioner | 2-5 years | $115,000 - $135,000 | An established provider comfortable with a full patient load. May begin to take on extra responsibilities like precepting new NPs. |
| Experienced Nurse Practitioner | 6-10 years | $125,000 - $150,000 | A seasoned NP with deep expertise. Can handle highly complex cases and may be a clinical lead or department resource. |
| Senior/Lead Nurse Practitioner| 10+ years | $140,000 - $175,000+ | Often in leadership, administrative, or highly specialized roles. May manage a team of NPs or run their own practice. |
### Beyond the Base Salary: Understanding Total Compensation
Your annual salary is only one part of the financial equation. A comprehensive compensation package for a Nurse Practitioner often includes several other valuable components that can significantly boost total earnings and overall financial well-being. When evaluating a job offer, it's crucial to look beyond the base number and consider the full package.
- Sign-On Bonuses: Increasingly common, especially in high-demand areas or for hard-to-fill specialties. These can range from $5,000 to $25,000 or more, paid out as a lump sum or over the first year of employment.
- Performance Bonuses: Many large healthcare systems and private practices offer annual or quarterly bonuses tied to specific metrics. These can be based on patient volume (RVUs - Relative Value Units), patient satisfaction scores, or quality-of-care measures. These bonuses can add 5-15% to your base salary.
- Profit Sharing: In private practice settings, some NPs may be eligible for a share of the clinic's profits, directly tying their hard work to the financial success of the practice.
- Retirement Benefits: This is a huge factor. Strong packages include a 401(k) or 403(b) with a generous employer match. A 5% match on a $130,000 salary is an extra $6,500 per year in tax-advantaged savings.
- Continuing Medical Education (CME) Allowance: NPs are required to complete a certain number of continuing education hours to maintain their certification and licensure. Most employers provide an annual allowance for this, typically ranging from $1,500 to $3,000, along with paid time off to attend conferences.
- Paid Time Off (PTO): A generous PTO package (including vacation, sick leave, and holidays) is a significant quality-of-life benefit.
- Health and Wellness Benefits: Comprehensive health, dental, and vision insurance for you and your family is a standard and valuable part of the package.
- Malpractice Insurance: Employers almost always provide professional liability (malpractice) insurance. It's important to understand the type (claims-made vs. occurrence) and coverage limits.
- Loan Repayment Programs: Some employers, particularly non-profits, Federally Qualified Health Centers (FQHCs), and facilities in underserved areas, offer loan repayment assistance, which can be worth tens of thousands of dollars.
---
Key Factors That Influence Your Salary
While the national averages provide a solid baseline, a Nurse Practitioner's actual salary is influenced by a complex interplay of factors. Understanding these variables is the key to maximizing your earning potential throughout your career. This is where you can move from earning an average salary to becoming a top-tier earner in the field.
### 1. Area of Specialization
Perhaps the single most significant factor after location is your chosen specialty. The demand and compensation for different NP populations vary widely, driven by patient needs, the complexity of care, and shortages of providers in certain fields.
- Psychiatric-Mental Health Nurse Practitioner (PMHNP): Consistently the highest-paid specialty. With a nationwide mental health crisis and a severe shortage of psychiatrists, PMHNPs are in extremely high demand to manage conditions like depression, anxiety, bipolar disorder, and ADHD. Their ability to provide therapy and prescribe psychotropic medications makes them invaluable.
- *Estimated Salary Range:* $135,000 - $180,000+
- Adult-Gerontology Acute Care Nurse Practitioner (AG-ACNP): These NPs work in high-acuity settings like intensive care units (ICUs), emergency departments, and specialty hospital floors. They manage complex, critically ill adult patients. The high-stakes environment and advanced procedural skills required command a premium salary.
- *Estimated Salary Range:* $125,000 - $165,000+
- Neonatal Nurse Practitioner (NNP): NNPs care for critically ill and premature infants in the Neonatal Intensive Care Unit (NICU). This is a highly specialized, high-stress field that requires immense skill and precision.
- *Estimated Salary Range:* $120,000 - $160,000+
- Family Nurse Practitioner (FNP): The most common specialization. FNPs provide primary care to patients of all ages, from infants to the elderly. While the base salary may be slightly lower than acute care specialties, the sheer number of job opportunities across every conceivable setting (urban, rural, outpatient, hospital) is a major advantage.
- *Estimated Salary Range:* $110,000 - $140,000
- Pediatric Nurse Practitioner (PNP): Focusing on the care of children, PNPs can work in primary care (well-child visits, common illnesses) or acute care (hospital-based pediatrics). Primary care PNP salaries are similar to FNPs, while acute care PNP salaries are higher.
- *Estimated Salary Range:* $105,000 - $135,000
- Women's Health Nurse Practitioner (WHNP): Specializing in gynecological and obstetric care, WHNPs are vital providers of reproductive health services. Salaries are generally solid but can be slightly lower than other specialties unless combined with other skills or roles.
- *Estimated Salary Range:* $105,000 - $130,000
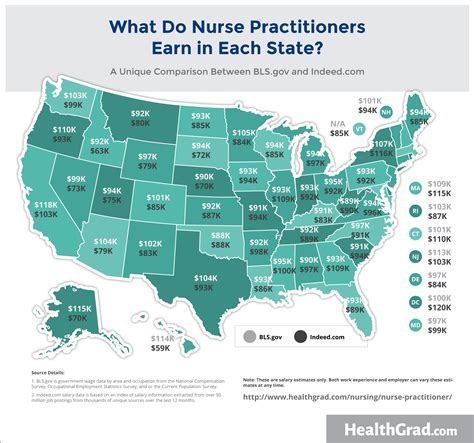
### 2. Geographic Location
"Location, location, location" is as true in healthcare careers as it is in real estate. NP salaries can vary by more than $50,000 per year depending on the state, city, and even whether the setting is urban or rural. This is driven by local market demand, cost of living, and, crucially, the state's scope of practice laws.
According to the BLS (May 2023), the top-paying states for Nurse Practitioners are:
1. California: Annual Mean Wage: $161,540
2. New Jersey: Annual Mean Wage: $151,160
3. Washington: Annual Mean Wage: $145,710
4. Oregon: Annual Mean Wage: $143,260
5. Nevada: Annual Mean Wage: $142,880
It's critical to balance these high salaries against the cost of living. A $160,000 salary in San Francisco, CA, may not go as far as a $130,000 salary in a lower-cost-of-living state like Texas.
Conversely, some of the lowest-paying states include:
- Tennessee: $106,120
- Alabama: $107,350
- South Carolina: $109,140
Metropolitan vs. Rural:
- High-Paying Metro Areas: The highest absolute salaries are often found in major metropolitan areas, especially on the West Coast. For example, San Jose-Sunnyvale-Santa Clara, CA, boasts an annual mean wage of $199,630.
- Rural and Underserved Areas: While the base salary in rural areas may be lower, these positions often come with significant financial incentives designed to attract providers. These can include substantial sign-on bonuses, student loan repayment programs (like the National Health Service Corps, which can provide up to $50,000 in loan forgiveness), and a much lower cost of living, making the "take-home" value very competitive.
### 3. Work Setting (Type of Employer)
Where you choose to work has a direct impact on your paycheck. Different practice environments have different funding models, patient populations, and operational demands, all of which are reflected in their compensation structures.
BLS data from May 2023 shows a clear hierarchy in pay by industry:
- Outpatient Care Centers: (e.g., urgent care centers, specialty clinics) - Median Salary: $138,980. These settings are often fast-paced and revenue-focused, leading to higher compensation.
- Hospitals (State, Local, and Private): - Median Salary: $136,130. Hospital-based NPs, especially in acute care roles, command high salaries due to the complexity and acuity of their patient populations.
- Offices of Physicians: - Median Salary: $125,120. This is the traditional primary care or specialty practice setting. While the median is lower than hospitals, high-performing private practices can offer significant bonus potential.
- Offices of Other Health Practitioners: (e.g., NP-owned practices) - Median Salary: $118,290.
- Educational Services (Colleges, Universities): While clinically practicing faculty may earn more, full-time academic roles typically pay less than clinical roles but offer different benefits like tuition remission and a better work-life balance.
Additionally, locum tenens (temporary or traveling NP) work offers some of the highest pay rates, often exceeding $100 per hour. These roles fill temporary staffing gaps and pay a premium for flexibility and expertise, though they may not include traditional benefits like retirement plans.
### 4. Level of Education: MSN vs. DNP
The standard entry-level degree for a Nurse Practitioner is the Master of Science in Nursing (MSN). However, the Doctor of Nursing Practice (DNP) is increasingly promoted as the terminal degree for clinical practice. The question many aspiring NPs have is: does a DNP translate to a higher salary?
The answer is nuanced.
- For direct clinical roles: Currently, the salary difference between an MSN-prepared NP and a DNP-prepared NP in the *same clinical role* is often minimal to non-existent, perhaps a few thousand dollars per year. Most employers hire for the NP certification (e.g., FNP-BC), not the degree itself.
- For leadership and advanced roles: The DNP provides a significant advantage. The degree focuses on systems leadership, quality improvement, evidence-based practice implementation, and healthcare policy. This makes DNP-prepared NPs prime candidates for roles like:
- Director of Advanced Practice
- Clinical Department Head
- Healthcare Administrator
- University Faculty
- Policy Advocate
These leadership positions command much higher salaries, often in the $150,000 to $200,000+ range. Therefore, while a DNP might not give you an immediate 20% bump in your first clinical job, it opens doors to higher-paying career trajectories down the line.
### 5. Years of Experience
As detailed in the "Salary Deep Dive" section, experience is a linear driver of income. A new graduate NP is, understandably, less efficient and requires more support than a provider with a decade of experience. Experienced NPs can manage more complex patients, work more efficiently, and often generate more revenue for their practice (measured in RVUs).
The salary curve tends to be steepest in the first 5-7 years of practice. After the 10-year mark, significant salary increases often come from moving into leadership, changing work settings, or developing a highly specialized niche practice.
### 6. In-Demand Skills and Certifications
Beyond your primary population focus, acquiring specific procedural skills, sub-specialty certifications, and unique competencies can make you a more attractive candidate and justify a higher salary.
- Procedural Skills: In specialties like dermatology, orthopedics, or emergency medicine, proficiency in procedures is highly valued. Examples include:
- Advanced suturing and wound care
- Joint injections
- Skin biopsies and cryotherapy
- Intubation or central line placement (in acute care)
- First-Assist Certification (RNFA): For NPs working in surgical specialties, being a certified Registered Nurse First Assistant allows them to directly assist in the operating room, a skill that commands a significant pay increase.
- Bilingualism: In diverse communities, being fluent in a second language (especially Spanish) is a massive asset. It improves patient care and safety and can lead to a pay differential or a hiring preference.
- Telehealth Proficiency: Since 2020, telehealth has become a standard mode of care delivery. NPs who are adept at virtual consultations and comfortable with the associated technology are highly sought after.
- Business Acumen: For those interested in private practice, skills in medical billing, coding, and practice management are invaluable and can lead to partnership or ownership opportunities.
- Sub-specializations: An FNP who obtains additional certification in diabetes education (CDCES) or an AG-ACNP who specializes in cardiology can command a higher salary within their respective fields.
---
Job Outlook and Career Growth

The career outlook for Nurse Practitioners is not just bright; it's explosive. This is one of the fastest-growing professions in the entire United States economy, driven by a convergence of powerful healthcare trends.
The U.S. Bureau of Labor Statistics projects that employment for Nurse Practitioners will grow by a staggering 45% from 2022 to 2032. This is more than ten times the average growth rate for all occupations. This translates to about 118,600 new job openings for NPs expected each year, on average, over the decade.
So, what is fueling this incredible demand?
1. An Aging Population: The large baby boomer generation is aging, increasing the demand for healthcare services, particularly for the management of chronic diseases that are common in older adults. NPs are perfectly positioned to provide this type of long-term, comprehensive care.
2. Physician Shortages: The Association of American Medical Colleges (AAMC) projects a significant shortfall of physicians, particularly in primary care, in the coming years. NPs are essential to filling this gap and ensuring patients have access to care, especially in rural and underserved communities.
3. A Focus on Preventative Care: The healthcare system is increasingly shifting its focus from reactive treatment to proactive prevention and wellness management. The holistic, patient-centered training of NPs makes them ideal leaders in this area.
4. Expanding Scope of Practice: A growing number of states are moving toward Full Practice Authority for NPs. This allows them to work more independently, open their own clinics, and provide a wider range of services,