---
For those drawn to the intricate and deeply personal field of women's health, a career as an Obstetrics and Gynecology (OB-GYN) Nurse Practitioner offers a rare combination of clinical autonomy, profound patient impact, and significant financial reward. You are not just a healthcare provider; you are a trusted confidante, an educator, and a steadfast advocate through some of the most pivotal moments in a person's life. But beyond the immense personal satisfaction, what is the tangible value of this expertise? What can you expect your OB-GYN Nurse Practitioner salary to be, and how can you maximize it?
This comprehensive guide is designed to answer those questions and more. We will delve into the granular details of compensation, exploring not just the national averages but the critical factors that can add tens of thousands of dollars to your annual earnings. We will dissect the robust job outlook for this profession, projected to be one of the fastest-growing in the nation, and provide a clear, step-by-step roadmap for aspiring professionals. I remember the profound sense of relief in my sister’s voice when she described her appointment with a Women’s Health Nurse Practitioner (WHNP). For the first time, she felt her concerns were not just clinically assessed but truly heard, a testament to the unique blend of medical expertise and compassionate care that defines this role. This is more than a job; it is a calling with the backing of a stable, lucrative, and deeply meaningful career trajectory.
---
### Table of Contents
- [What Does an OB-GYN Nurse Practitioner Do?](#what-does-an-ob-gyn-nurse-practitioner-do)
- [Average OB-GYN Nurse Practitioner Salary: A Deep Dive](#average-ob-gyn-nurse-practitioner-salary-a-deep-dive)
- [Key Factors That Influence Your Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Become an OB-GYN Nurse Practitioner](#how-to-get-started-in-this-career)
- [Is This Career Your Calling?](#conclusion)
---
What Does an OB-GYN Nurse Practitioner Do?

An OB-GYN Nurse Practitioner, more formally known as a Women's Health Nurse Practitioner (WHNP), is an Advanced Practice Registered Nurse (APRN) who specializes in the comprehensive care of women across their lifespan. While they often work in collaboration with obstetricians and gynecologists, in many states, they have the authority to operate their own practices, diagnose conditions, and prescribe medications independently. Their scope is vast, encompassing everything from adolescent health to post-menopausal care.
The WHNP's role is a unique fusion of advanced medical knowledge, hands-on clinical skills, and profound patient education. They are primary care providers for many women, managing both wellness and illness with a specialized focus.
Core Responsibilities and Daily Tasks:
A WHNP's duties are diverse and patient-centered. On any given day, they might:
- Provide Gynecological Care: Conduct annual well-woman exams, including Pap tests, breast exams, and screenings for sexually transmitted infections (STIs).
- Manage Contraception: Counsel patients on various birth control methods, prescribe contraceptives, and perform procedures like IUD and contraceptive implant insertions and removals.
- Offer Obstetric Care: Manage low-risk pregnancies, provide prenatal check-ups, order and interpret diagnostic tests (like ultrasounds), and offer postpartum care. While they don't typically deliver babies in a hospital setting (a role reserved for Certified Nurse-Midwives or physicians), they are integral to the entire prenatal and postnatal journey.
- Diagnose and Treat Conditions: Evaluate, diagnose, and manage common gynecological issues such as polycystic ovary syndrome (PCOS), endometriosis, uterine fibroids, vaginal infections, and menstrual disorders.
- Educate Patients: Spend significant time educating patients on topics like reproductive health, sexual wellness, preconception health, menopause management, and disease prevention.
- Perform In-Office Procedures: Conduct procedures such as colposcopies (examining the cervix after an abnormal Pap test), endometrial biopsies, and vulvar biopsies.
- Promote Health and Wellness: Provide counseling on nutrition, exercise, and lifestyle modifications relevant to women's health, including managing symptoms of menopause.
### A Day in the Life of a WHNP
To make this tangible, let's follow a hypothetical WHNP named Dr. Anya Sharma, DNP, WHNP-BC, working in a busy urban clinic.
- 8:00 AM: Anya arrives, reviews her patient schedule for the day, and checks lab results and patient messages that came in overnight. She flags a few results for immediate follow-up calls.
- 8:30 AM: Her first patient is a 22-year-old for her first-ever well-woman exam. Anya spends extra time building rapport, explaining every step of the exam to ease her anxiety, and providing comprehensive contraceptive counseling.
- 9:15 AM: Next is a 35-year-old patient at 28 weeks gestation for a routine prenatal check-up. Anya measures fetal growth, checks the fetal heart rate, reviews her blood pressure and glucose screening results, and answers questions about creating a birth plan.
- 10:00 AM: A 48-year-old patient comes in to discuss perimenopausal symptoms, including hot flashes and sleep disturbances. Anya discusses the risks and benefits of hormone replacement therapy (HRT) versus non-hormonal options and collaborates with the patient to create a personalized symptom management plan.
- 11:00 AM: Anya performs an IUD insertion for a 28-year-old patient seeking long-acting reversible contraception.
- 12:00 PM: Lunch break, during which she catches up on charting, returns non-urgent patient calls, and consults with a collaborating physician about a complex patient case.
- 1:00 PM: A follow-up appointment with a 31-year-old patient diagnosed with PCOS. They review the effectiveness of her current medication regimen, discuss lifestyle modifications, and set new health goals.
- 1:45 PM: Anya sees a 19-year-old for STI testing and counseling on safe sex practices in a non-judgmental, confidential environment.
- 2:30 PM: Time for a scheduled in-office colposcopy for a patient with an abnormal Pap test. Anya carefully performs the procedure and takes biopsies, explaining the process and what to expect next.
- 3:30 PM - 5:00 PM: The afternoon is reserved for administrative time. Anya finishes her patient charts, signs off on prescription refills, reviews new lab reports, and participates in a weekly clinic meeting to discuss quality improvement initiatives.
This snapshot reveals a career that is anything but monotonous. It demands a high level of clinical skill, emotional intelligence, and a genuine passion for advocating for women's health.
---
Average OB-GYN Nurse Practitioner Salary: A Deep Dive
Now, let's address the central question: what does this demanding and rewarding career pay? The compensation for OB-GYN Nurse Practitioners is highly competitive, reflecting their advanced education, specialized skills, and the critical demand for their services.
It's important to start with a broad benchmark. The U.S. Bureau of Labor Statistics (BLS), the gold standard for employment data, groups all Nurse Practitioners together. As of its May 2023 report (the most recent available data), the median annual salary for Nurse Practitioners was $128,490. The salary range is wide, with the lowest 10 percent earning around $94,990 and the top 10 percent earning more than $174,990.
However, specialty plays a significant role. To get a more precise figure for OB-GYN NPs, we turn to reputable salary aggregators that provide specialty-specific data.
- Salary.com, as of late 2023, reports the median annual salary for a Women's Health Nurse Practitioner in the United States to be $124,194, with a typical range falling between $115,221 and $134,845.
- Payscale.com provides a similar figure, with an average base salary for a WHNP reported at approximately $105,081 per year. Payscale's data often includes a higher proportion of early-career professionals, which can influence the average. Their reported range spans from $84,000 to $130,000.
- Glassdoor reports a total pay average of $136,743 per year for OB/GYN Nurse Practitioners, with a likely range between $117,000 and $160,000. This figure includes base salary as well as additional compensation like bonuses.
Taking a composite view of these authoritative sources, a realistic national average salary for an OB-GYN Nurse Practitioner falls squarely in the $120,000 to $135,000 per year range. However, this is just the midpoint. As we will explore, factors like experience, location, and work setting can dramatically shift this number.
### Salary by Experience Level
Your earning potential grows significantly as you accumulate experience, develop clinical confidence, and increase your efficiency. An experienced WHNP who can manage a full patient panel with complex needs is far more valuable to an employer than a new graduate.
Here is a typical salary progression, synthesized from data provided by Payscale and Salary.com:
| Career Stage | Years of Experience | Typical Annual Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-2 Years | $95,000 - $110,000 | New graduate, developing procedural skills, often working with more direct supervision. Focus is on building a patient base and gaining confidence. |
| Mid-Career | 3-9 Years | $110,000 - $130,000 | Proficient in a wide range of procedures and managing complex patient cases. Works with greater autonomy. May begin to mentor new NPs. |
| Experienced | 10-19 Years | $125,000 - $145,000 | Highly autonomous, efficient, and often seen as a clinical expert. May take on leadership roles (e.g., Lead NP) or specialize in a niche area. |
| Senior/Late-Career| 20+ Years | $135,000 - $160,000+ | Top clinical expert, potential for roles in administration, education, or research. Commands the highest salaries due to a wealth of knowledge and experience. |
### Beyond the Base Salary: Understanding Total Compensation
Your annual salary is only one piece of the compensation puzzle. Total compensation includes a variety of benefits and bonuses that can add significant value. When evaluating a job offer, it's crucial to look at the entire package:
- Bonuses: Many employers, particularly in private practice and large hospital systems, offer performance-based or annual bonuses. These can range from a few thousand dollars to 10% or more of your base salary, often tied to productivity metrics (like the number of patients seen) or quality of care outcomes.
- Profit Sharing: Some private OB-GYN practices offer a profit-sharing plan, allowing you to benefit directly from the financial success of the clinic. This can be a powerful incentive and a substantial addition to your income.
- Continuing Medical Education (CME) Allowance: To maintain licensure and certification, WHNPs must complete ongoing education. Most employers provide an annual allowance, typically ranging from $1,500 to $3,000, along with paid time off to attend conferences or workshops. This is a critical, tax-free benefit.
- Retirement Plans: Look for strong retirement packages, such as a 401(k) or 403(b) with a generous employer match. A 5% match on a $125,000 salary is an extra $6,250 of free money per year toward your retirement.
- Health and Wellness Benefits: Comprehensive health, dental, and vision insurance are standard. Also, look for life insurance, disability insurance (both short-term and long-term), and paid time off (vacation, sick leave, and holidays).
- Licensure and Certification Reimbursement: Many employers will cover the costs of renewing your RN license, APRN license, DEA license, and your WHNP-BC certification, saving you hundreds of dollars each year.
- Sign-On Bonuses: In competitive markets or for hard-to-fill positions, employers may offer a substantial sign-on bonus, which can range from $5,000 to $20,000 or more, to attract top talent.
When comparing job offers, calculate the full value of the compensation package. A job with a slightly lower base salary but an excellent retirement match, a generous CME allowance, and a performance bonus structure could be more lucrative in the long run.
---
Key Factors That Influence Salary

While the national average provides a useful benchmark, your individual OB-GYN Nurse Practitioner salary will be determined by a confluence of six key factors. Understanding these variables is the most powerful tool you have for negotiating your worth and maximizing your lifetime earnings.
### 1. Level of Education: MSN vs. DNP
The foundational educational requirement to become a WHNP is a Master of Science in Nursing (MSN). However, the Doctor of Nursing Practice (DNP) is increasingly becoming a popular and valuable credential.
- Master of Science in Nursing (MSN): This is the standard degree for entry into advanced practice. It provides the essential clinical training, diagnostic reasoning, and pharmacology knowledge required for the role. The majority of practicing WHNPs today hold an MSN.
- Doctor of Nursing Practice (DNP): The DNP is a terminal degree focused on clinical practice rather than academic research (which is the focus of a Ph.D. in Nursing). The curriculum emphasizes leadership, evidence-based practice implementation, quality improvement, healthcare policy, and systems thinking.
Does a DNP increase your salary? Yes, but the impact varies. Research from the AANP and other industry surveys suggests that DNP-prepared NPs earn, on average, $5,000 to $10,000 more per year than their MSN-prepared counterparts in similar clinical roles. The real financial benefit of a DNP often comes from the types of jobs it unlocks. DNP graduates are highly sought after for leadership positions such as:
- Clinical Director or Department Head
- Nurse Practitioner Manager
- Healthcare Executive
- University Faculty
- Clinical Research Coordinator
These leadership roles naturally command higher salaries. Therefore, while a DNP provides a modest boost in a purely clinical role, its primary financial value lies in opening doors to higher-paying administrative, academic, and leadership career paths.
### 2. Years of Experience
As highlighted in the previous section, experience is arguably the single most significant driver of salary growth in a clinical setting. This is not simply about time served; it's about the accumulation of expertise.
- Early Career (0-2 years): In this phase, you are consolidating your academic knowledge with real-world practice. Your focus is on efficiency and mastering core competencies. Salaries are at the lower end of the spectrum.
- Mid-Career (3-9 years): You now operate with significant autonomy. You can handle a higher volume of patients, manage more complex cases without frequent consultation, and perform advanced procedures with confidence. This increased productivity and expertise directly translate to higher value for your employer and, consequently, a higher salary, often in the $110,000 to $130,000 range.
- Senior Career (10+ years): At this stage, you are a clinical authority. You are the go-to person for difficult cases, a mentor for new NPs, and a leader in implementing new clinical protocols. Your vast experience is a major asset, justifying a salary at the top end of the scale, often exceeding $140,000 or $150,000, especially in high-paying locations or settings.
### 3. Geographic Location
Where you choose to practice will have a dramatic impact on your salary. Compensation for NPs varies widely by state, region, and even between urban and rural areas within the same state. This variation is driven by demand, cost of living, and state-specific scope of practice laws.
According to the BLS May 2023 data for all Nurse Practitioners, the top-paying states are:
1. California: Annual Mean Wage: $161,540
2. New Jersey: Annual Mean Wage: $147,140
3. Massachusetts: Annual Mean Wage: $146,160
4. Oregon: Annual Mean Wage: $144,790
5. Nevada: Annual Mean Wage: $141,360
Conversely, states in the Southeast and parts of the Midwest tend to have lower average salaries, though this is often offset by a significantly lower cost of living.
Metropolitan Areas: High-paying metro areas often exist even outside the top-paying states. Cities in California (San Jose-Sunnyvale-Santa Clara, San Francisco-Oakland-Hayward) consistently top the list with salaries approaching or exceeding $180,000.
Rural vs. Urban: The dynamic here is complex. While major metropolitan areas often have the highest absolute salaries due to high cost of living and large hospital systems, rural and underserved areas can also be surprisingly lucrative. To attract talent, these areas may offer:
- Higher-than-average base salaries.
- Significant sign-on bonuses.
- Student loan repayment programs through federal or state initiatives (like the National Health Service Corps Loan Repayment Program, which can be worth $50,000 or more).
### 4. Work Setting (Company Type & Size)
The type of facility you work in is another major determinant of your compensation structure.
- Private Physician's Office: This is a very common setting for WHNPs. Salaries are generally competitive. Smaller practices may offer lower base salaries but compensate with a more intimate work environment and potential for profit-sharing. Larger group practices can offer higher base pay and more robust benefits.
- Hospital Systems (Inpatient or Outpatient Clinics): Hospitals are often the highest-paying employers. They have structured salary scales, excellent benefits, and union representation in many cases, which can lead to higher wages and guaranteed annual raises. A WHNP working in a hospital-owned outpatient OB-GYN clinic can expect to earn at the higher end of the salary spectrum.
- Community Health Centers & Federally Qualified Health Centers (FQHCs): These non-profit clinics serve medically underserved populations. While their base salaries may be slightly lower than those at large hospitals, they often provide exceptional benefits, a strong sense of mission, and eligibility for significant federal loan forgiveness programs.
- Academia/University Health Centers: Working at a university student health center or as faculty in a nursing program offers a different lifestyle, often with better work-life balance and excellent benefits. Clinical salaries may be slightly less than in a high-volume private practice, but the total package is often very attractive.
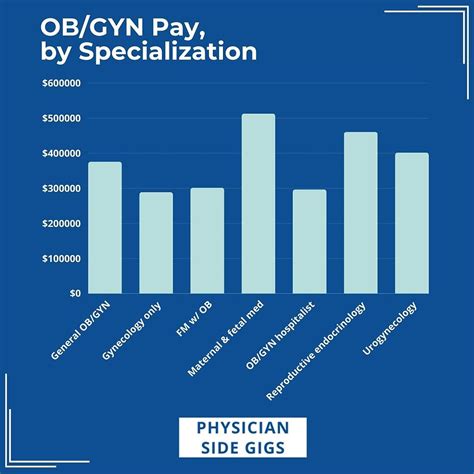
### 5. Area of Sub-Specialization
While "OB-GYN" or "Women's Health" is the primary specialty, you can develop further sub-specialty expertise that can significantly boost your earning potential. These roles often require additional on-the-job training or post-graduate certification.
- Reproductive Endocrinology and Infertility (REI): WHNPs in this field work at fertility clinics, assisting with in-vitro fertilization (IVF) cycles, managing fertility medications, and performing procedures like intrauterine insemination (IUI). This is a highly specialized and lucrative niche.
- Gynecologic Oncology: Here, you would work with a team managing the care of patients with cancers of the reproductive organs. This role involves managing complex treatment side effects, providing survivorship care, and intensive patient education. The high-stakes nature of this field often commands a higher salary.
- Urogynecology: This sub-specialty focuses on female pelvic floor disorders, such as urinary incontinence and pelvic organ prolapse. WHNPs may perform advanced diagnostic testing (like urodynamics) and manage both surgical and non-surgical treatments.
- High-Risk Obstetrics (Maternal-Fetal Medicine): In this setting, WHNPs help manage pregnancies complicated by conditions like diabetes, hypertension, or multiple gestations. This requires an advanced level of knowledge and skill, which is compensated accordingly.
### 6. In-Demand Skills
Beyond your core education, specific clinical and professional skills can make you a more valuable candidate and give you leverage in salary negotiations.
High-Value Clinical Skills:
- Advanced Procedural Competence: Being proficient in procedures like colposcopy, endometrial biopsy, IUD/Nexplanon insertion, and basic obstetric ultrasonography makes you a huge asset to a practice, generating revenue and improving workflow.
- First-Assist in Surgery: Some WHNPs pursue training to become an RN First Assistant (RNFA), allowing them to assist surgeons in the operating room during procedures like C-sections or hysterectomies. This certification can add a significant premium to your salary.
- Prescribing and Medication Management: Expertise in complex medication regimens, such as those for hormone replacement therapy, fertility treatments, or managing chronic conditions in pregnancy, is highly valued.
Valuable Professional Skills:
- Leadership and Management: Experience in training new staff, leading quality improvement projects, or managing clinic schedules can position you for a Lead NP role with a corresponding pay increase.
- Billing and Coding Knowledge: Understanding the nuances of medical billing and coding (ICD-10, CPT codes) helps ensure the practice is properly reimbursed for your services, making you a more profitable employee.
- Telehealth Proficiency: In the modern healthcare landscape, being comfortable and effective at providing virtual care is a highly sought-after skill.
- Spanish Language Fluency: In many parts of the U.S., being a bilingual provider who can care for Spanish-speaking patients without an interpreter is a massive advantage that can and should be leveraged for higher pay.
---
Job Outlook and Career Growth

The professional future for OB-GYN Nurse Practitioners is exceptionally bright. The demand for their services is high and projected to grow rapidly over the next decade, ensuring a high degree of job security and opportunity.
The U.S. Bureau of Labor Statistics (BLS) projects that employment for Nurse Practitioners as a whole will grow by a staggering 45 percent from 2022 to 2032. This is one of the fastest growth rates of any occupation in the entire country. This translates to an average of about 12,600 job openings for NPs projected each year over the decade.
Several powerful trends are fueling this explosive growth:
- Increased Demand for Healthcare Services: As the general population ages and grows, the need for healthcare, including preventive and specialized care, will continue to rise.
- A Focus on Preventive Care: There is a growing emphasis in the U.S. healthcare system on prevention and wellness, which is a cornerstone of the NP model of care. WHNPs excel at patient education and preventive screenings.
- Physician Shortages: The nation is facing a projected shortage of physicians, particularly in primary care and specialized fields like OB-GYN. NPs are perfectly positioned to fill this gap, providing high-quality care and improving access for patients, especially in rural and underserved communities.
- Expanding Scope of Practice: A growing number of states are granting "Full Practice Authority" to Nurse Practitioners. This allows them to practice independently without the direct supervision of a physician, enabling them to open their own clinics and practice to the full extent of their education and training. This trend increases the attractiveness and autonomy of the profession.
- Cost-Effectiveness: NPs provide excellent patient outcomes at a lower cost than their physician counterparts, making them an attractive option for hospitals, clinics, and insurance companies focused on value-based care.
### Emerging Trends and Future Challenges
While the outlook is overwhelmingly positive, aspiring and current WHNPs should be aware of the evolving landscape.
Emerging Trends:
- Telehealth Integration: The use of telehealth for prenatal visits, contraceptive counseling, and follow-up care is here to stay. WHNPs who are adept at using virtual platforms will have a competitive edge.
- Holistic and Integrative Care: Patients are increasingly seeking a more holistic approach to their health. WHNPs who incorporate knowledge of nutrition, mental health, and wellness practices into their care will be in high demand.
- Increased Specialization: As the field grows, there will be more opportunities for WHNPs to sub-specialize in areas like infertility, oncology, or pelvic health, leading to new and exciting career paths.
Future Challenges:
- Scope of Practice Battles: While the trend is toward full practice authority, there is still political and professional opposition in some states. Advocating for the profession through professional organizations is crucial.
- Burnout: The demands of healthcare can be intense. High patient loads and administrative burdens can lead to burnout. It is essential for WHNPs to prioritize their own well-being and seek employers who support a healthy work-life balance.
- Staying Current: Women's health is a rapidly advancing field. New medications, guidelines, and technologies emerge constantly. A commitment to lifelong learning is non-negotiable.
### How to Advance and Stay Relevant
A career as a WHNP is not static. There are numerous pathways for advancement:
1. Become a Clinical Leader: Pursue roles like Lead NP, Clinic Manager, or Director of Advanced Practice Providers within a hospital system.
2. Specialize: Gain the experience and certifications needed to move into a lucrative sub-specialty like REI or gynecologic oncology.
3. Educate the Next Generation: With a DNP, you can become a clinical preceptor or a full-time faculty member at a university, shaping the future of nursing.
4. Embrace Entrepreneurship: In states with full practice authority, you can open your own women's health clinic, giving you ultimate autonomy and financial control.
5. Engage in Health Policy: Use your expertise to advocate for women's health issues and advance the nursing profession at the state or national level.
---
How to Get Started in This Career

Becoming an OB-GYN
