Introduction

Imagine the profound responsibility of holding a human life—and the promise of a new one—in your hands. This is the daily reality for an organ transplant surgeon, a profession that stands at the apex of medical science, human resilience, and profound ethical consideration. It's a career not for the faint of heart, demanding years of relentless training, unwavering precision, and an emotional fortitude that few possess. For those drawn to this incredible calling, the rewards are immense, not only in the immeasurable satisfaction of saving lives but also in the significant financial compensation that reflects the immense skill and dedication required. An organ transplant surgeon salary is among the highest in the medical field, with experienced practitioners often earning well over $500,000 to $700,000 annually, and top earners exceeding the million-dollar mark.
This isn't just a job; it's a lifelong commitment to mastery. I once had a conversation with the family of a young woman who received a life-saving liver transplant. They didn't just speak of the surgeon's technical skill; they spoke of the calm reassurance and unwavering confidence that gave them hope during the darkest hours, a testament to the fact that this role transcends the operating room. This guide is designed to be your definitive resource, whether you are a high school student dreaming of a medical career, a medical student charting your specialty, or a general surgery resident contemplating a fellowship. We will dissect every facet of the organ transplant surgeon's career, from the intricate daily responsibilities to a granular breakdown of the salary you can expect, the factors that influence it, and a step-by-step roadmap to achieving this extraordinary professional goal.
### Table of Contents
- [What Does an Organ Transplant Surgeon Do?](#what-does-an-organ-transplant-surgeon-do)
- [Average Organ Transplant Surgeon Salary: A Deep Dive](#average-organ-transplant-surgeon-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Become an Organ Transplant Surgeon: The Step-by-Step Path](#how-to-become-an-organ-transplant-surgeon-the-step-by-step-path)
- [Conclusion: Is the Demanding Path Worth the Reward?](#conclusion-is-the-demanding-path-worth-the-reward)
---
What Does an Organ Transplant Surgeon Do?
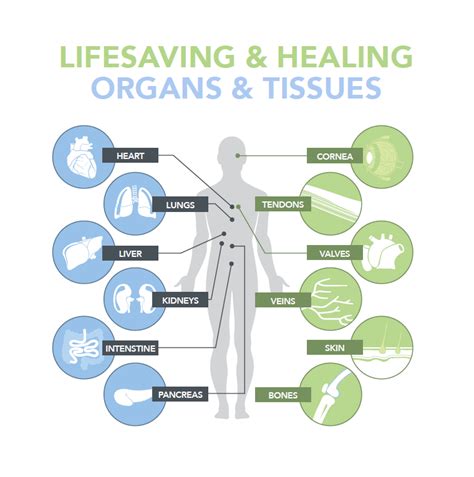
An organ transplant surgeon is a highly specialized physician who performs organ transplantations, which involve removing a diseased or failing organ from a patient and replacing it with a healthy organ from a donor. This description, however, only scratches the surface of a complex and multifaceted role that extends far beyond the confines of the operating theater.
The surgeon's involvement begins long before any incision is made. They are central figures in the comprehensive care team that manages the entire transplant journey for a patient. Their core responsibilities can be broken down into three primary phases: pre-operative, operative, and post-operative.
Core Responsibilities and Daily Tasks:
- Pre-Operative Patient Evaluation: Surgeons meticulously evaluate potential transplant candidates to determine their eligibility. This involves reviewing extensive medical histories, conducting physical examinations, and collaborating with a multidisciplinary team including transplant coordinators, hepatologists, nephrologists, cardiologists, social workers, and psychiatrists to assess the patient's overall health and support system.
- Donor Evaluation and Organ Procurement: In the case of living donors (e.g., kidney or liver segments), the surgeon is responsible for evaluating the donor's health to ensure the procedure is safe for them. For deceased donors, the surgeon often travels, sometimes at a moment's notice, to procure the organ. This is a high-stakes, time-sensitive procedure to ensure the organ's viability.
- Surgical Procedures: This is the most visible part of the job. Transplant surgeons perform complex and lengthy operations, including:
- Recipient Operation (Transplantation): Removing the diseased organ and implanting the new one, which involves the delicate reconnection of major arteries, veins, and ducts.
- Donor Operation (Procurement): Surgically removing the organ from a deceased donor or a portion of an organ from a living donor.
- Post-Operative Care: The surgeon's responsibility does not end when the patient leaves the operating room. They are heavily involved in the immediate post-operative care in the Intensive Care Unit (ICU), managing complications like bleeding, infection, or organ rejection. They continue to follow patients for years after the surgery through outpatient clinics to monitor organ function and manage immunosuppressive medications.
- Collaboration and Team Leadership: Transplant surgeons work at the heart of a large team. They must communicate effectively with referring physicians, nurses, transplant coordinators, and other specialists to ensure seamless, integrated patient care.
- Research and Academia: Many transplant surgeons, particularly those at academic medical centers, are actively involved in research to improve transplant outcomes, develop new surgical techniques, and advance the science of immunosuppression. They also teach medical students and train the next generation of general and transplant surgery residents and fellows.
- On-Call Responsibilities: The nature of organ transplantation is unpredictable. Surgeons are on call for organ offers, which can come at any time, day or night, requiring them to be ready to perform surgery with little notice.
> ### A Day in the Life of a Transplant Surgeon
>
> 5:30 AM: Wake up, review overnight patient vitals and lab results from the ICU on the hospital's electronic health record system.
> 6:30 AM: Arrive at the hospital for morning rounds. Lead the transplant team (fellows, residents, nurse practitioners) to see all post-operative patients, discussing their progress, adjusting medication, and making a plan for the day.
> 8:00 AM: Scrub in for a scheduled 8-hour liver transplant surgery. The atmosphere is one of intense focus and precise teamwork.
> 4:00 PM: Surgery complete. The surgeon dictates the operative note and speaks with the patient's anxious family, providing an update and explaining the critical next steps in the ICU.
> 5:00 PM: Head to the outpatient clinic to see patients who are weeks, months, or even years post-transplant. These appointments involve reviewing bloodwork, adjusting immunosuppression, and addressing any patient concerns.
> 7:00 PM: Attend a departmental meeting to discuss research progress and review complex patient cases with the multidisciplinary team.
> 8:30 PM: Head home for dinner, but remain on call.
> 11:00 PM: Phone rings. The transplant coordinator has a potential deceased donor organ offer for a high-priority patient. The surgeon evaluates the donor information, accepts the offer, and prepares to head back to the hospital for an overnight procurement and subsequent transplant surgery. The day starts again.
---
Average Organ Transplant Surgeon Salary: A Deep Dive
The journey to becoming a transplant surgeon is one of the longest and most arduous in medicine, and the compensation structure reflects this immense investment. An organ transplant surgeon salary is consistently positioned in the upper echelon of physician earnings, driven by the complexity of the procedures, the high-stakes nature of the work, and the extensive training required.
According to a variety of authoritative sources, the national average salary for an organ transplant surgeon in the United States typically falls between $450,000 and $750,000 per year. However, this is just a median range, and the actual figures can vary dramatically.
- Salary.com reports the median salary for a Transplant Surgeon to be $557,113 as of late 2023, with a typical range falling between $466,723 and $671,353.
- The Medscape Physician Compensation Report 2023 places general surgery among high-earning specialties, and transplant surgery is a subspecialty that often commands a premium above the general surgery average of $412,000. Specialized fields like cardiothoracic surgery (which includes heart and lung transplants) report average earnings of $706,775.
- Data from physician recruiting firms and platforms like Doximity consistently show that procedural specialists, especially those in highly complex surgical fields like transplant, are among the top earners in medicine.
It's crucial to understand that the "average" salary is just a starting point. The compensation journey for a transplant surgeon progresses significantly with experience.
### Organ Transplant Surgeon Salary by Experience Level
The salary trajectory shows a steep climb from the initial post-fellowship years to senior-level positions, where surgeons often take on administrative and leadership roles in addition to their clinical duties.
| Experience Level | Typical Years of Experience | Typical Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-3 Years Post-Fellowship | $350,000 - $500,000 | Recently completed fellowship. Focus is on building clinical volume, refining surgical skills, and establishing a reputation. Often in academic settings. |
| Mid-Career | 4-10 Years | $500,000 - $750,000 | Established surgeon with a solid track record. Higher productivity, more complex cases. May start taking on leadership roles (e.g., Associate Program Director). |
| Senior / Late-Career | 10+ Years | $700,000 - $1,000,000+ | Highly experienced, nationally recognized expert. Often holds leadership positions like Chief of Transplant Surgery or Program Director. Compensation heavily influenced by bonuses, administrative stipends, and practice ownership. |
*Sources: Synthesized data from Salary.com, Medscape, Doximity Physician Compensation Reports, and data from medical recruiting firms like Merritt Hawkins.*
### A Closer Look at the Full Compensation Package
The base salary is only one piece of the puzzle. The total compensation for a transplant surgeon is a comprehensive package that often includes significant variable pay and robust benefits.
- Base Salary: The guaranteed annual income, which forms the foundation of the compensation package.
- Productivity Bonuses: This is a major component of a surgeon's earnings, especially in private practice or hospital-employed models. It is often tied to Work Relative Value Units (wRVUs). An wRVU is a metric used by Medicare to determine the value of a physician's service, factoring in the time, skill, and intensity required. A complex liver transplant can generate a high number of wRVUs, directly translating to a larger bonus.
- Sign-On Bonus: To attract top talent in a competitive market, hospitals and practices often offer substantial sign-on bonuses, which can range from $25,000 to $100,000 or more.
- Retention Bonuses: Bonuses paid for staying with an employer for a specified period (e.g., 3-5 years).
- Relocation Assistance: A stipend to cover the costs of moving to a new city for a job.
- Academic/Administrative Stipend: Surgeons in academic medical centers or those who serve as a Division Chief or Medical Director receive an additional stipend for their leadership and teaching responsibilities.
- Comprehensive Benefits: This is a significant, non-taxable part of compensation. It almost always includes:
- Professional Liability (Malpractice) Insurance: This is an extremely expensive but critical benefit, usually covered entirely by the employer.
- Health, Dental, and Vision Insurance: For the surgeon and their family.
- Retirement Plans: Generous 401(k) or 403(b) plans with employer matching contributions.
- Continuing Medical Education (CME) Allowance: An annual stipend (e.g., $5,000 - $15,000) to cover costs for conferences, journals, and courses required to maintain medical licensure.
- Paid Time Off (PTO): Typically 4-6 weeks of vacation, plus sick leave.
When all these elements are combined, the total value of an organ transplant surgeon's compensation package can be 20-30% higher than their base salary alone.
---
Key Factors That Influence an Organ Transplant Surgeon Salary

While the national averages provide a useful benchmark, a transplant surgeon's actual earnings are influenced by a complex interplay of several key factors. Understanding these variables is essential for anyone aiming to maximize their earning potential in this field. This is the most critical section for understanding the nuances behind the numbers.
###
1. Level of Education, Training, and Certification
In surgery, the educational path is less about a variety of degrees and more about the depth and prestige of training. All transplant surgeons must complete a grueling educational journey, but specific elements can impact starting salaries and long-term earning potential.
- Medical School (MD vs. DO): All transplant surgeons will have a doctorate in medicine, either an M.D. (Doctor of Medicine) or a D.O. (Doctor of Osteopathic Medicine). Both degrees provide a path to residency and licensure. In surgery, there is historically no significant salary difference based on the degree type, as compensation is determined by specialty and performance post-residency.
- General Surgery Residency: This is a 5- to 7-year training program following medical school. The reputation of the residency program (e.g., at a top-tier academic institution like Johns Hopkins, Massachusetts General Hospital, or Stanford) can enhance a surgeon's competitiveness for top fellowship positions and, subsequently, premier job offers with higher starting salaries.
- Transplant Surgery Fellowship: This is the critical 2- to 3-year period of subspecialty training that defines a transplant surgeon. Completing a fellowship at a high-volume, highly-respected transplant center is paramount. These programs provide exposure to a high number of complex cases, cutting-edge research, and connections with leaders in the field, all of which directly translate to higher value in the job market.
- Board Certification: After completing residency and fellowship, surgeons must become board-certified by the American Board of Surgery (ABS). This is a non-negotiable requirement for practicing at any reputable hospital. Maintaining certification through continuous learning and periodic exams is mandatory and essential for full earning potential. A lack of board certification would severely limit employment options and drastically reduce salary.
###
2. Years of Experience and Reputation
As illustrated in the salary table above, experience is one of the most significant drivers of income growth. This is not simply a reward for longevity; it reflects a tangible increase in value.
- Early Career (0-5 Years): Surgeons fresh out of fellowship are still building their speed, efficiency, and reputation. Their focus is on proving their skills and handling a steady volume of standard cases.
- Mid-Career (5-15 Years): At this stage, a surgeon has established a strong reputation. They are faster and more efficient in the operating room, can handle more complex and high-risk cases, and have demonstrably good patient outcomes. Their productivity (wRVU generation) is typically at its peak, leading to substantial bonus-based compensation. They may also be invited to speak at national conferences, further enhancing their reputation and value.
- Senior Career (15+ Years): Senior surgeons often transition into leadership roles. While their surgical volume might decrease slightly, their overall compensation often increases due to administrative stipends for positions like:
- Chief of Transplant Surgery: Overseeing the entire transplant division.
- Surgical Director of a Transplant Program (e.g., Liver Transplant Director): Leading a specific organ program.
- Chair of the Department of Surgery: A top-level academic and administrative role.
These roles come with significant additional compensation that can push total earnings towards the top of the spectrum.
###
3. Geographic Location
Where a transplant surgeon practices has a profound impact on their salary. This variation is driven by a combination of local market demand, the cost of living, and the concentration of medical facilities.
- High-Paying States and Regions: Generally, salaries tend to be higher in the Midwest and Southeast. States like Alabama, Kentucky, Tennessee, Wisconsin, and Indiana often offer very competitive compensation packages to attract surgeons away from the more traditionally popular coastal cities. This is a classic supply-and-demand scenario.
- Lower-Paying (but still high) States and Regions: Major metropolitan areas on the coasts, such as New York City, Boston, Los Angeles, and San Francisco, may offer slightly lower base salaries. This is often because these are highly desirable places to live and have a high concentration of academic medical centers, creating more competition for positions. However, the high cost of living in these areas can sometimes offset the perceived salary difference.
- Rural vs. Urban: Transplant surgery is almost exclusively practiced in major urban centers at large tertiary or quaternary care hospitals, as these are the only facilities with the requisite infrastructure (ICUs, specialized staff, etc.). Therefore, the typical "rural premium" seen in some other medical specialties is less applicable here. The key distinction is between a major academic hub and a large community hospital system in a mid-sized city.
Illustrative Regional Salary Differences (Estimated Annual Median)
| Region | Example States/Cities | Estimated Median Salary | Rationale |
| :--- | :--- | :--- | :--- |
| Southeast | Atlanta, GA; Birmingham, AL | $650,000 - $800,000+ | High demand, strong hospital systems competing for talent. |
| Midwest | Cleveland, OH; Milwaukee, WI | $600,000 - $750,000 | Major transplant centers (e.g., Cleveland Clinic), lower cost of living. |
| West Coast | Los Angeles, CA; Seattle, WA | $500,000 - $650,000 | Higher cost of living, desirable location, high concentration of surgeons. |
| Northeast | Boston, MA; New York, NY | $475,000 - $600,000 | Heavy concentration of prestigious academic centers, high competition for roles. |
*Source: Analysis based on Doximity and Merritt Hawkins compensation report trends.*
###
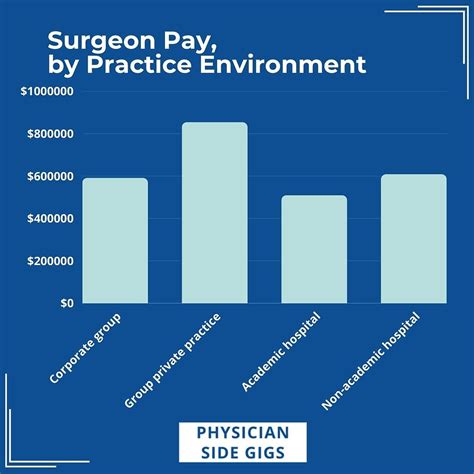
4. Practice Setting & Employer Type
The type of institution a surgeon works for is a critical determinant of both their salary structure and overall earning potential.
- Academic Medical Centers: These are university-affiliated hospitals.
- Pros: Prestige, opportunities for research and teaching, cutting-edge technology, typically excellent benefits, and a focus on complex, groundbreaking cases.
- Cons: Base salaries are often lower compared to private settings. A portion of the surgeon's time is "protected" for non-clinical academic work (research, teaching), which doesn't generate wRVUs, leading to lower productivity-based bonuses.
- Salary Structure: Moderate base salary + smaller bonus + academic stipend.
- Private Practice (Physician-Owned Group): This model is less common in transplant surgery than in other specialties but still exists.
- Pros: Highest income potential. Surgeons are often partners and share in the profits of the group. Direct correlation between work ethic and income.
- Cons: Higher risk, significant administrative and business responsibilities (hiring staff, managing billing), and the need to cover overhead and malpractice insurance costs.
- Salary Structure: Lower base salary (or a "draw") + very high percentage of profits/collections.
- Large Hospital Systems (Employed by Hospital): This is the most common model today. Surgeons are employees of a large non-profit or for-profit hospital or healthcare network.
- Pros: High and stable base salary, strong productivity bonuses, no administrative burden of running a business, excellent benefits, and access to the hospital's resources.
- Cons: Less autonomy compared to private practice. Subject to hospital administration policies and productivity targets.
- Salary Structure: High base salary + significant wRVU-based productivity bonus. This model often provides the best balance of high income and stability.
###
5. Area of Specialization (Organ Type)
Within the field of transplant surgery, there are further subspecializations based on the organ system. Compensation can vary depending on the complexity and length of the procedures, as well as the market demand for that specialty.
- Cardiothoracic (Heart and Lung) Transplant Surgery: This is generally the highest-paid transplant subspecialty. The procedures are incredibly complex, lengthy, and high-risk, commanding the highest wRVU values. The training path is also often longer, including a full cardiothoracic surgery residency. Average salaries can push towards $700,000 - $1,000,000+.
- Liver Transplant Surgery: Liver transplants are also extremely complex and lengthy procedures. Liver transplant surgeons are highly compensated, with salaries often in the $550,000 - $750,000 range. This field also includes living donor liver transplantation, a technically demanding procedure.
- Kidney and Pancreas Transplant Surgery: While still highly complex, kidney transplants are the most common transplant procedure. The surgeries are generally shorter and less complex than heart or liver transplants, which can result in slightly lower wRVU generation per case. Salaries are excellent but typically fall just below liver and heart, often in the $450,000 - $650,000 range. Surgeons in this field often perform a higher volume of surgeries.
###
6. In-Demand Skills and Additional Competencies
Beyond the standard job requirements, certain skills can make a surgeon more valuable and command a higher salary.
- Robotic and Minimally Invasive Surgery: Proficiency in using robotic platforms (like the da Vinci Surgical System) for donor nephrectomies (kidney removal) or other procedures is a highly sought-after skill. It can lead to better patient outcomes and is a major draw for hospitals looking to market their technological prowess.
- Living Donor Transplantation Expertise: Being an expert in living donor liver or kidney transplantation is a major value-add. These are elective, highly complex procedures that require a unique skillset in managing both the donor and the recipient.
- Pediatric Transplant Surgery: This is a niche within a niche. Pediatric transplant surgeons require additional fellowship training and possess a rare skillset, which often comes with premium compensation.
- Research and Grant Funding: For surgeons in academia, a strong track record of published research and, most importantly, the ability to secure major research grants (e.g., from the National Institutes of Health - NIH) is a direct path to promotion and higher salary through endowed professorships and institutional support.
- Leadership and Business Acumen: Skills in leadership, management, and understanding healthcare finance become increasingly important for senior roles. A surgeon who can effectively lead a team, manage a budget, and strategically grow a transplant program is invaluable to a hospital.
---
Job Outlook and Career Growth

For those willing to undertake the demanding training, the career outlook for organ transplant surgeons is exceptionally strong and stable. While the U.S. Bureau of Labor Statistics (BLS) does not track transplant surgeons as a distinct category, we can analyze the outlook by looking at the broader category of "Physicians and Surgeons" and combining it with industry-specific trends.
The BLS projects employment for Physicians and Surgeons to grow by 3% from 2022 to 2032, which is about as fast as the average for all occupations. However, this general number belies the specific, robust demand for transplant specialists. The key drivers fueling the need for more transplant surgeons are:
1. An Aging Population: As the large baby boomer generation ages, there is a corresponding increase in age-related organ failure, particularly
