For those driven by an unyielding passion for medicine, a profound desire to make a life-altering impact, and the intellectual stamina to master one of the most complex fields in existence, the career of a pediatric neurosurgeon stands as a pinnacle of professional achievement. It is a path defined by immense responsibility, intricate skill, and the daily reality of holding a child's future in one's hands. But alongside this profound sense of purpose comes a question of practical consideration for any aspiring medical professional: what is the paediatric neurosurgeon salary?
The answer is as complex and multifaceted as the career itself. While headline figures often point to some of the highest earnings in any profession, the reality is a spectrum influenced by a decade-plus of training, geographic location, practice type, and an array of other factors. The compensation is, without question, extraordinary, with top earners comfortably exceeding a million dollars annually. However, this financial reward is the byproduct of a level of dedication and sacrifice few can comprehend. I once met the parents of a child who underwent a complex surgery for a brain tumor. The way they spoke of their pediatric neurosurgeon wasn't just with respect, but with a profound reverence, as if describing the person who had single-handedly returned their world to its axis. It’s a stark reminder that this career is measured in far more than dollars.
This guide will dissect every component of a pediatric neurosurgeon's earnings, career path, and future outlook. We will move beyond simple averages to provide a granular, data-driven analysis for students, residents, and anyone captivated by this challenging and uniquely rewarding specialization.
### Table of Contents
- [What Does a Paediatric Neurosurgeon Do?](#what-does-a-paediatric-neurosurgeon-do)
- [Average Paediatric Neurosurgeon Salary: A Deep Dive](#average-paediatric-neurosurgeon-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
What Does a Paediatric Neurosurgeon Do?

A pediatric neurosurgeon is a highly specialized medical doctor who diagnoses, treats, and surgically manages disorders of the central and peripheral nervous systems in children, from newborns and infants through adolescence. Their domain is the brain, spine, and the intricate network of nerves that control every function of a developing body. This is not simply adult neurosurgery scaled down; it is a distinct specialty that requires a deep understanding of the dynamic, growing nature of a child's anatomy and physiology.
The conditions they treat are among the most serious and complex in medicine:
- Congenital Abnormalities: Issues present at birth, such as spina bifida (myelomeningocele), hydrocephalus (the buildup of fluid in the brain), encephalocele, and craniofacial anomalies like craniosynostosis (premature fusion of skull sutures).
- Brain and Spinal Cord Tumors: Diagnosing and performing complex resections of both benign and malignant tumors in delicate, developing neural tissue.
- Traumatic Brain and Spine Injuries: Managing severe head trauma, spinal fractures, and other injuries resulting from accidents.
- Epilepsy and Movement Disorders: Performing surgical procedures like hemispherectomies, lesionectomies, or implanting vagus nerve stimulators (VNS) or deep brain stimulation (DBS) devices to control intractable seizures or conditions like dystonia.
- Vascular Malformations: Treating conditions like arteriovenous malformations (AVMs) and moyamoya disease, which can cause strokes in children.
- Spasticity: Performing procedures like selective dorsal rhizotomy (SDR) to relieve severe muscle tightness in children with cerebral palsy.
### A Day in the Life of a Paediatric Neurosurgeon
The concept of a "typical day" is often elusive, as the role is a demanding blend of scheduled procedures, emergent crises, and patient consultations. However, a representative day might look something like this:
- 5:30 AM - 6:30 AM (Pre-Rounds): The day begins before dawn. The neurosurgeon arrives at the hospital, gets coffee, and immediately begins reviewing overnight events, imaging scans (MRIs, CTs) of post-operative patients, and lab results for the entire service. They check in with the on-call resident or fellow to discuss any urgent patient issues that arose overnight.
- 6:30 AM - 7:30 AM (Morning Rounds): The neurosurgeon leads the clinical team—which includes residents, fellows, physician assistants, and nurse practitioners—on rounds. They go room-to-room in the Pediatric ICU and the neurosurgery floor, examining each patient, speaking with parents, adjusting treatment plans, and teaching the junior members of the team.
- 7:30 AM - 4:00 PM (The Operating Room): This is the heart of the job. Today’s main case is a craniotomy for a 6-year-old with a cerebellar tumor. The procedure will last 6-8 hours. It is an act of supreme focus and precision, using high-powered microscopes and sophisticated neuronavigation technology. The surgeon may take a brief break while an assistant closes the incision. Between or after major cases, they might perform a shorter procedure, like a shunt placement for a baby with hydrocephalus.
- 4:00 PM - 6:00 PM (Afternoon Clinic): After scrubbing out, the surgeon heads to their outpatient clinic. Here, they see a mix of new patient consultations and post-operative follow-ups. This involves examining children, explaining complex diagnoses and surgical plans to anxious parents in clear, empathetic language, and coordinating care with neurologists, oncologists, and pediatricians.
- 6:00 PM - 8:00 PM (Administrative Work & Evening Rounds): The day is far from over. The surgeon dictates operative notes, answers dozens of emails, responds to pages, reviews new consults and scans, and prepares for the next day's surgeries. They will perform a final check-in on their most critical patients ("evening rounds") before heading home.
- On-Call: Several times a month, the neurosurgeon is on call, meaning they are available 24/7 to handle any emergency—a child with a severe head injury from a car accident, a baby born with spina bifida, or a shunt that has suddenly failed. This often means returning to the hospital in the middle of the night for life-saving surgery.
This relentless schedule underscores why the compensation for this role is so significant. It is a career that demands a complete fusion of one's personal and professional life.
Average Paediatric Neurosurgeon Salary: A Deep Dive
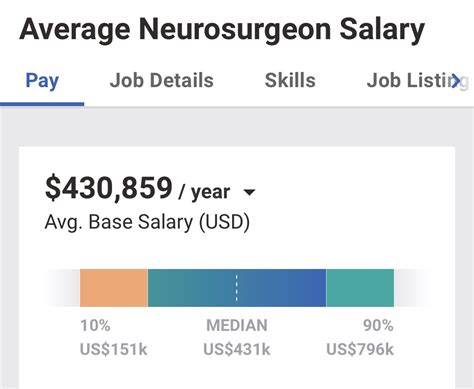
The paediatric neurosurgeon salary is consistently ranked among the highest in the medical field and, indeed, across all professions. This level of compensation reflects the unparalleled length of training (12-15 years post-college), the high-stakes nature of the work, the grueling hours, and the scarcity of qualified practitioners.
While exact figures fluctuate based on the source and the factors discussed in the next section, a clear picture of earning potential emerges from leading industry reports and salary aggregators.
According to the 2023 Medscape Physician Compensation Report, which surveys a wide range of physicians, neurosurgery (as a whole) is the highest-paid specialty, with an average annual compensation of $788,313. While this report doesn't always isolate the pediatric subspecialty, other specialized data confirms that pediatric neurosurgeons earn within this top tier.
Data from the salary platform [Salary.com](https://www.salary.com/research/salary/benchmark/neurosurgeon-salary) corroborates these high figures. As of late 2023, their data suggests the median neurosurgeon salary in the United States is approximately $698,701, with a typical range falling between $526,301 and $883,701.
It's crucial to understand that these figures are not static and represent a midpoint. Early-career and late-career earnings can differ dramatically.
### Salary by Experience Level
The salary trajectory for a pediatric neurosurgeon shows significant growth after the initial post-fellowship years. Reputation, efficiency in the operating room, and the ability to take on more complex (and thus higher-reimbursement) cases all contribute to this increase.
| Career Stage | Years of Experience | Typical Annual Salary Range | Notes |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-3 years post-fellowship | $450,000 - $650,000 | Often includes a guaranteed salary for the first 1-2 years to build a practice. May have a lower starting point in purely academic roles. |
| Mid-Career | 4-10 years | $650,000 - $950,000 | Transition to productivity-based models (RVUs). Reputation is established, leading to more referrals. |
| Senior/Experienced | 11-20 years | $850,000 - $1,200,000+ | Peak earning years. May hold leadership positions (e.g., Division Chief). Highly sought after for complex cases. |
| Late Career / Pre-Retirement | 20+ years | $700,000 - $1,000,000+ | May choose to scale back on call duties or operative volume, leading to a slight decrease from peak earnings, but still exceptionally high. |
*Sources: Aggregated data from Medscape, Doximity Physician Compensation Reports, AMGA surveys, and observations from industry recruiters.*
### Anatomy of a Compensation Package
The headline salary is only one part of the total compensation package. A pediatric neurosurgeon's earnings are typically a blend of several components, especially after the first few years of practice.
- Base Salary: This is the guaranteed portion of the salary. In the first 1-2 years at a new job, this may be the entirety of the compensation to allow the surgeon to build their patient volume.
- Productivity Bonuses (RVU-Based): This is the most significant component for most experienced surgeons. Compensation is tied to Relative Value Units (RVUs), a measure used by Medicare to value the work involved in a physician's service. Every procedure, clinic visit, and consultation is assigned an RVU value. The surgeon earns a certain dollar amount per RVU generated above a set threshold. This model directly rewards high surgical volume and efficiency. For example, a complex tumor resection can be worth 60-100 RVUs, while a simple shunt placement might be 15-20 RVUs.
- Performance & Quality Bonuses: Many hospitals and large practice groups are incorporating bonuses tied to quality metrics. These can include patient outcomes, patient satisfaction scores, infection rates, and participation in hospital quality improvement committees.
- On-Call Stipends: Surgeons are often paid a separate daily or hourly stipend for the days they are on call for the hospital, compensating them for the lifestyle disruption and the burden of handling emergencies.
- Sign-On Bonus: To attract top talent in a competitive market, hospitals often offer substantial sign-on bonuses, which can range from $50,000 to over $200,000.
- Relocation Allowance: A stipend to cover the costs of moving to a new city.
- Retirement & Benefits: This includes robust retirement plans (e.g., 401(k) or 403(b) with generous employer matching), comprehensive health, dental, and vision insurance for the surgeon and their family.
- Malpractice Insurance: Crucially, the employer almost always pays for the surgeon's medical malpractice insurance, a significant expense that can exceed $100,000 per year for neurosurgeons. This is a vital part of the compensation package.
- Continuing Medical Education (CME) Allowance: An annual stipend (e.g., $5,000 - $15,000) to cover the costs of attending conferences, subscribing to journals, and fulfilling other educational requirements to maintain their medical license and board certification.
For those in private practice, compensation can also include a share of the practice's profits, making the earning potential even higher, though this comes with the added responsibilities of running a business.
Key Factors That Influence a Paediatric Neurosurgeon Salary
While the national averages provide a strong benchmark, an individual pediatric neurosurgeon's salary can vary by hundreds of thousands of dollars based on a confluence of factors. Understanding these variables is key to maximizing earning potential over a long career.
###
1. The Unrivaled Impact of Education and Training
The immense salary is a direct consequence of the longest and arguably most arduous training path in all of medicine. This journey is a process of extreme vetting and specialization that produces a very small number of qualified individuals.
- Undergraduate Degree (4 years): A bachelor's degree with a rigorous pre-med curriculum (biology, chemistry, physics, organic chemistry).
- Medical School (4 years): Earning an M.D. (Doctor of Medicine) or D.O. (Doctor of Osteopathic Medicine) degree. Aspiring neurosurgeons must achieve top scores on the United States Medical Licensing Examination (USMLE).
- Neurosurgery Residency (7-8 years): This is the crucible. After medical school, doctors match into a neurosurgery residency program. These are notoriously competitive. The seven years are spent in grueling 100-hour work weeks, learning the foundations of brain and spine surgery on adult patients. The final year is often a "Chief Resident" year with significant administrative and teaching responsibilities.
- Pediatric Neurosurgery Fellowship (1-2 years): After completing the demanding neurosurgery residency, a doctor who wants to specialize in children must then complete an additional fellowship dedicated solely to pediatric neurosurgery. This is where they learn the nuances of operating on developing brains and spines.
- Board Certification: After completing all training, the final step is achieving board certification from the American Board of Neurological Surgery (ABNS), which involves rigorous written and oral examinations. Subsequently, they can obtain a subspecialty certification from the American Board of Pediatric Neurological Surgery (ABPNS). Being board-certified is a non-negotiable requirement for any reputable hospital and is a significant factor in commanding a top-tier salary.
This entire path, from the start of college to finishing fellowship, takes a minimum of 16-17 years. The immense debt accumulated (often $200,000-$400,000 in student loans) and the delayed entry into high-earning years are factored into the ultimate compensation.
###
2. The Unwavering Climb: Years of Experience
As illustrated in the previous section's table, experience is one of the most powerful drivers of salary growth. This isn't just about automatic yearly raises; it's about a qualitative change in the surgeon's value.
- Early Career (Years 1-3): Surgeons focus on building a practice, establishing referral patterns with pediatricians and neurologists, and honing their efficiency. They are typically on a guaranteed salary that transitions to a productivity model.
- Mid-Career (Years 4-10): The surgeon has now established a strong reputation. They are faster and more confident in the OR, allowing them to perform more cases. They begin to take on more complex, higher-RVU cases that were previously handled by senior partners. Their income climbs steeply as they move fully into the RVU-based model.
- Peak Career (Years 11-20+): At this stage, a pediatric neurosurgeon is a master of their craft. They are sought after for the most difficult cases regionally or even nationally. They often take on leadership roles such as Chief of Pediatric Neurosurgery or Surgical Director of a hospital's Neuroscience Institute. These administrative roles come with additional stipends and elevate their standing and salary. Their vast experience makes them highly efficient, maximizing their RVU generation. This is where salaries can regularly surpass the $1 million mark.
###
3. Location, Location, Location: Geographic Disparities
Where a pediatric neurosurgeon practices has a profound impact on their salary. This is driven by supply and demand, cost of living, and the concentration of major medical centers.
Data from physician recruiting firms and salary aggregators consistently shows a pattern where salaries are often higher in the Midwest, Southeast, and non-coastal West. This is counterintuitive to many, who assume salaries are highest in major coastal cities like New York or Los Angeles. However, these areas often have a higher concentration of surgeons competing for positions at prestigious academic centers, which can sometimes pay less than private or hospital-employed positions in less saturated markets.
- High-Paying Regions/States: States in the Midwest (e.g., Wisconsin, Indiana, Ohio) and Southeast (e.g., Florida, Georgia, Tennessee) often offer some of the most competitive compensation packages to attract scarce talent. These areas may have a large patient population served by fewer specialists. For example, a state with only one or two major children's hospitals will create intense demand for the surgeons who work there.
- Moderate-to-High Paying Regions/States: The West (excluding the Pacific coast) and Southwest also offer very strong salaries.
- Variable/Lower-Paying Regions/States: The Northeast and the Pacific Coast (California) can be more variable. While the raw salary numbers are still immense, they may not be as high when adjusted for the astronomical cost of living. Furthermore, the desirability of these locations means academic medical centers there may not need to offer the highest possible dollar amount to attract top-tier candidates.
According to a Doximity report, some of the highest-paying metropolitan areas for specialists are often not the largest ones, with cities like Charlotte, NC, and St. Louis, MO, frequently out-earning New York and Boston in terms of physician compensation.
###
4. The Practice Setting: Academic vs. Private vs. Hospital-Employed
The type of organization a surgeon joins is a critical determinant of their compensation structure and overall earning potential.
- Academic Medical Centers: These are large hospitals affiliated with a university and medical school (e.g., Boston Children's Hospital, Children's Hospital of Philadelphia).
- Pros: Prestige, cutting-edge research opportunities, teaching responsibilities (training residents and fellows), access to the most complex and rare cases. Robust benefits and support staff.
- Cons: Salaries are often on the lower end of the spectrum for the specialty. There is often a "salary cap" and less flexibility in compensation. A significant portion of time is dedicated to non-clinical (and non-RVU-generating) activities like research and teaching. The path to promotion can be rigid.
- Private Practice: This involves a surgeon joining or becoming a partner in a small- to medium-sized group that contracts with hospitals to provide neurosurgical services.
- Pros: The highest earning potential. Once a partner, the surgeon shares in the practice's profits. Greater autonomy in business and clinical decisions.
- Cons: Significant administrative burden (managing staff, billing, insurance negotiations, marketing). Less job security and more financial risk. Responsible for covering practice overhead. Must purchase their own benefits and malpractice insurance if not a large group.
- Hospital Employment: The most common model today. The surgeon is a direct employee of a hospital or a large, multi-specialty health system.
- Pros: High and stable salary, often with strong productivity bonuses. No administrative or business management responsibilities. The hospital covers all overhead, including staff, equipment, and malpractice insurance. Excellent benefits and job security.
- Cons: Less autonomy. The surgeon is an employee and must adhere to hospital policies and productivity targets. There may be less flexibility in scheduling and more pressure to meet volume metrics.
###
5. Niche Expertise: The Power of Sub-Specialization
Within the already niche field of pediatric neurosurgery, developing a national reputation in a specific sub-specialty can further enhance earning potential and professional standing. While this doesn't always translate to a different base salary, it dramatically increases referrals for high-complexity, high-RVU cases, thus driving up productivity-based pay.
- Pediatric Neuro-Oncology: Focusing on the surgical treatment of brain and spinal tumors.
- Pediatric Epilepsy Surgery: Specializing in complex procedures to control seizures.
- Fetal Neurosurgery: An emerging field involving surgery on babies while still in the womb to correct conditions like spina bifida.
- Craniofacial Surgery: Working as part of a multidisciplinary team to correct complex skull and facial abnormalities.
- Minimally Invasive Neurosurgery: Mastering endoscopic techniques to treat conditions like hydrocephalus or certain tumors with smaller incisions and faster recovery times.
A surgeon known as "the" person to see for complex epilepsy surgery in a multi-state region will have a packed surgical schedule and, consequently, very high earnings.
###
6. In-Demand Skills That Boost Your Value
Beyond the scalpel, certain skills can make a neurosurgeon more valuable to a hospital system and lead to higher compensation or leadership opportunities.
- Robotics and Advanced Technology: Proficiency with surgical robots, advanced neuronavigation systems, and new imaging modalities.
- Leadership and Administrative Skills: The ability to lead a department, manage budgets, and oversee quality and safety initiatives is highly valued and compensated with administrative stipends.
- Research and Grant Writing: For academic surgeons, securing major research grants (e.g., from the National Institutes of Health - NIH) can come with protected time and salary support, making them a huge asset to their institution.
- Communication and Empathy: While a "soft skill," the ability to communicate effectively and compassionately with the families of sick children is paramount. Surgeons with high patient satisfaction scores are a major asset to hospitals in today's value-based care environment.
Job Outlook and Career Growth

The career outlook for pediatric neurosurgeons is exceptionally strong and stable. While the total number of positions is small, reflecting the niche nature of the field, the demand for qualified practitioners consistently outstrips the supply.
The U.S. Bureau of Labor Statistics (BLS) projects that employment for "Physicians and Surgeons" overall is expected to grow by 3% from 2022 to 2032. However, this general statistic doesn't capture the specific dynamics of a highly specialized field like pediatric neurosurgery. The true demand is driven by several key factors:
1. Scarcity of Specialists: There are only a few hundred board-certified pediatric neurosurgeons practicing in the entire United States. The lengthy and demanding training pipeline naturally limits the number of new entrants into the field each year. This scarcity creates a competitive job market where qualified candidates are highly sought after by children's hospitals.
2. Population Needs: While major pediatric neurological conditions are rare, they occur at a steady rate. The need for experts to treat hydrocephalus, brain tumors, spina bifida, and trauma is constant. Major metropolitan areas and regions need dedicated children's hospitals, and these hospitals cannot function without a pediatric neurosurgery service.
3. Retirement of an Aging Workforce: A significant portion of the current pediatric neurosurgical workforce is approaching retirement age. As these highly experienced surgeons retire, they will create vacancies that need to be filled by the next generation, ensuring a steady stream of job openings for newly trained fellows.
4. Advancements in Treatment: Medical and technological progress continually expands what is possible. The development of fetal surgery, new minimally invasive techniques, and advanced treatments for epilepsy and tumors means that conditions once considered untreatable now have surgical options. This expands the scope of the specialty and the need for surgeons trained in these cutting-edge methods.
### Future Challenges and Trends
Despite the positive outlook, the profession faces ongoing challenges and is subject to evolving trends:
- Burnout: The combination of extremely long hours, high-stakes pressure, life-and-death decisions, and emotional toll of treating sick children makes burnout a significant risk. Health systems are increasingly focused on physician wellness initiatives to mitigate this.
- Healthcare Reform and Reimbursement: Changes in healthcare policy and insurance reimbursement models can impact compensation. There is a continuous shift towards "value-based care," where payment is tied more to outcomes than to the volume of procedures performed. This may alter compensation structures in the future.
- Medical-Legal Environment: Neurosurgery, particularly pediatric neurosurgery, operates in a high-risk medical-legal environment. The cost of malpractice insurance, even when covered by an employer, reflects the immense risk associated with the specialty.
- Rise of Artificial Intelligence (AI): AI is not a threat to replace surgeons but a tool to augment their abilities. In the future, AI will likely play a greater role in analyzing medical images, planning surgical approaches, and predicting outcomes, requiring surgeons to adapt and integrate these new technologies into their practice.
### How to Stay Relevant and Advance
Advancement in this career is less about climbing a traditional corporate ladder and more about building expertise, reputation, and leadership.
- Lifelong Learning: Medicine is constantly changing. The best surgeons are committed to lifelong learning, regularly attending conferences, and mastering new techniques and technologies as they emerge.
- Publishing and Research: Contributing to the medical literature by publishing research papers and presenting at national conferences is key to building a national reputation and is essential for advancement in academia.
- Leadership Development: Taking on administrative roles—serving on hospital committees, mentoring residents, and eventually becoming a service line chief or department chair—is the primary path to formal advancement and higher earnings through administrative stipends.
- Building a Niche: As mentioned earlier, becoming the go-to expert for a specific complex condition is a powerful way to ensure a steady flow of high-acuity cases and solidify one's value.
How to Get Started in This Career: A 17-Year Roadmap
The path to becoming a pediatric neurosurgeon is a marathon of immense dedication, not a sprint. It requires foresight, resilience, and exceptional academic and personal discipline from a very early stage. Here is a step-by-step guide for the aspiring surgeon.
Step 1: High School (The Foundation)
- Focus: Excel in advanced science and math courses: AP Biology, AP Chemistry, AP Physics, and AP Calculus.
- Develop Skills: Cultivate strong study habits, time management, and a passion for learning.
- Gain Exposure: Volunteer at a local hospital or clinic to confirm your interest in medicine and patient care.
Step 2: Undergraduate University (4 Years - The Pre-Med Gauntlet)
- Major: Choose a major you are passionate about, but ensure you complete all pre-medical requirements with near-perfect grades (Biology, General Chemistry, Organic Chemistry, Physics, Biochemistry, English). A science major is common but not required.
- GPA and MCAT: Your goal is a GPA of 3.8 or higher. You must also achieve a top-tier score on the Medical College Admission Test (MCAT). For neurosurgery, this is non-negotiable.
- Extracurriculars: This is critical for differentiating your application.
- Research: Get involved in meaningful
