Introduction

For the aspiring medical professional drawn to both the intricate science of dermatology and the unique challenges of pediatric care, the field of pediatric dermatology represents a pinnacle of specialization. It’s a career that demands immense dedication, a compassionate bedside manner, and a sharp diagnostic eye. But what does this dedication yield in terms of financial reward and professional satisfaction? The answer is substantial. A pediatric dermatologist salary is among the highest in the medical field, with average earnings frequently landing between $350,000 and $500,000 annually, and top earners pushing well beyond that.
This isn't just a job; it's a calling with the profound ability to change a child's life. I once spoke with a dermatologist who shared a story about a young patient, a shy seven-year-old girl with a prominent vascular birthmark on her face that made her withdraw from school activities. After a series of precise laser treatments, the birthmark faded significantly, and the doctor described the breathtaking moment the girl looked in the mirror, broke into a wide smile, and turned to her mother to say, "Now I can play with everyone." It's in these moments that the true value of this profession—far beyond any salary figure—becomes crystal clear.
This guide is designed to be your definitive resource, whether you're a high school student dreaming of medical school, a medical student charting your specialty, or a resident weighing fellowship options. We will dissect every facet of a pediatric dermatologist's career, from the day-to-day responsibilities to the complex factors that shape your earning potential. We will explore the rigorous path to becoming a specialist and the bright future that awaits those who complete the journey.
### Table of Contents
- [What Does a Pediatric Dermatologist Do?](#what-does-a-pediatric-dermatologist-do)
- [Average Pediatric Dermatologist Salary: A Deep Dive](#average-pediatric-dermatologist-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
---
What Does a Pediatric Dermatologist Do?

A pediatric dermatologist is a medical doctor who has completed training in both dermatology and pediatrics, culminating in a specialized fellowship. This dual expertise uniquely qualifies them to diagnose and treat skin, hair, and nail conditions in infants, children, and adolescents. Their patient population ranges from newborns with complex genetic disorders to teenagers struggling with severe acne.
The scope of their practice is incredibly broad and requires a deep understanding of how skin diseases manifest and evolve differently in children compared to adults. Children's bodies are still developing, their immune systems are maturing, and their skin is more delicate, making them susceptible to a unique set of dermatologic issues.
Core Responsibilities and Conditions Treated:
- Diagnosis and Management of Common Conditions: While a general pediatrician can handle mild cases, a pediatric dermatologist is the expert for severe or resistant conditions like atopic dermatitis (eczema), psoriasis, warts, molluscum contagiosum, and acne.
- Congenital and Genetic Skin Disorders (Genodermatoses): This is a key area of their expertise. They manage rare and complex conditions present from birth, such as ichthyosis (disorders of dry, scaly skin), epidermolysis bullosa (a group of blistering skin conditions), and neurofibromatosis.
- Vascular Anomalies: They are the primary specialists for diagnosing and treating vascular birthmarks, including infantile hemangiomas ("strawberry marks") and port-wine stains. Treatment often involves advanced laser therapy.
- Pigmented Lesions and Skin Cancer: While skin cancer is rarer in children, pediatric dermatologists are trained to monitor moles and other pigmented lesions, identify risk factors, and diagnose and treat pediatric melanomas and other skin malignancies when they occur.
- Infections and Infestations: They treat complex or unusual bacterial, fungal, or viral skin infections, as well as infestations like severe scabies or lice.
- Procedural Dermatology: A significant part of their work involves hands-on procedures, including skin biopsies, cryosurgery (freezing), electrosurgery, surgical excisions of cysts and lesions, and sophisticated laser treatments.
### A Day in the Life of Dr. Anya Sharma, Pediatric Dermatologist
To make this role more tangible, let's walk through a typical day in a busy, hospital-affiliated pediatric dermatology clinic.
7:45 AM: Dr. Sharma arrives at the clinic. She grabs a coffee and spends 30 minutes reviewing the charts for her morning patients. She notes a follow-up on a 6-month-old with a growing hemangioma, a new patient referral for a 10-year-old with blistering lesions, and a teenager with cystic acne who isn't responding to standard therapy.
8:30 AM - 12:30 PM: Morning clinic begins. Patient appointments are scheduled every 20-30 minutes.
- 8:30 AM: The 6-month-old with the hemangioma. Dr. Sharma examines the lesion, takes clinical photos to track its growth, and discusses the risks and benefits of starting oral propranolol with the anxious parents.
- 9:00 AM: The teenager with cystic acne. Dr. Sharma has a long, empathetic conversation about the psychological impact of the condition. They discuss the next line of treatment: isotretinoin. She carefully explains the medication's side effects and the mandatory iPLEDGE program requirements.
- 9:30 AM: A 4-year-old with severe eczema covering 40% of his body. Dr. Sharma adjusts his topical steroid regimen and introduces the parents to wet wrap therapy techniques.
- 10:00 AM: The new 10-year-old patient with blistering. Dr. Sharma performs a careful examination and suspects a form of epidermolysis bullosa. She performs a small punch biopsy for definitive diagnosis, explaining every step to the child and parent to minimize fear.
- The rest of the morning is a mix of wart treatments, mole checks, and follow-ups for psoriasis and atopic dermatitis.
12:30 PM - 1:30 PM: Lunch and administrative time. Dr. Sharma dictates her morning notes, reviews lab results that have come in, and responds to urgent messages from referring pediatricians. She also has a quick call with a pediatric rheumatologist to coordinate care for a patient with a skin rash related to a systemic autoimmune disease.
1:30 PM - 4:30 PM: Afternoon procedure clinic. This block is dedicated to more time-intensive procedures.
- 1:30 PM: A 9-year-old with a port-wine stain undergoes their third pulsed dye laser treatment. Dr. Sharma and her nurse ensure the child is comfortable with topical anesthetic and distraction techniques.
- 2:30 PM: Dr. Sharma surgically excises a suspicious nevus (mole) from a 15-year-old's back, sending the tissue to pathology for analysis.
- 3:30 PM: A complex consultation with a family whose newborn was diagnosed with a rare genetic skin condition. This is an hour-long session focused on education, prognosis, and connecting the family with support networks and other specialists.
4:30 PM - 5:30 PM: Dr. Sharma wraps up her patient notes, signs off on prescription refills, and prepares her schedule for the next day. Once a week, this time is dedicated to a resident teaching session or a departmental research meeting. She leaves the clinic around 5:30 PM, fulfilled by the direct impact she's made on the health and confidence of her young patients.
---
Average Pediatric Dermatologist Salary: A Deep Dive
The financial compensation for the extensive training and specialized skill set of a pediatric dermatologist is significant. This subspecialty is one of the most lucrative in all of medicine, driven by high demand, a limited supply of qualified practitioners, and the procedural nature of the work.
It's important to note that salary data aggregators often group all dermatologists together. However, pediatric dermatology is on par with, and in some cases can exceed, the earnings of a general or cosmetic dermatologist, particularly in high-demand settings.
National Average Salary and Range
While specific data exclusively for pediatric dermatologists is less common, we can draw highly accurate conclusions from top-tier physician compensation reports covering all dermatologists. The subspecialty of pediatric dermatology does not negatively impact these figures and often enhances them due to its scarcity.
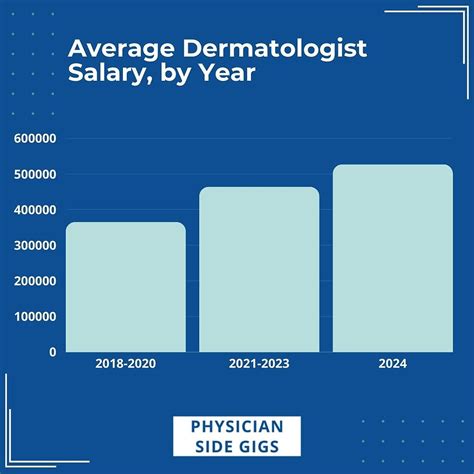
- According to the 2023 Doximity Physician Compensation Report, the average annual compensation for dermatologists is $501,000.
- The 2023 Medscape Dermatologist Compensation Report reports an average salary of $443,000.
- Data from Salary.com, updated for late 2023, shows the average dermatologist salary in the United States is $395,690, with a typical range falling between $340,190 and $461,290.
Based on these authoritative sources and industry knowledge, a reasonable and well-supported average annual salary for a U.S.-based pediatric dermatologist is approximately $420,000 to $470,000. However, the range is vast. An entry-level academic pediatric dermatologist might start closer to $280,000, while an experienced partner in a thriving private practice in a major metropolitan area could easily earn over $700,000.
Salary by Experience Level
Compensation in medicine grows significantly with experience, reputation, and efficiency. As a pediatric dermatologist builds their practice, they become faster, more proficient with procedures, and attract more referrals, all of which drive income.
| Experience Level | Typical Years of Experience | Estimated Annual Salary Range | Key Drivers |
| :--- | :--- | :--- | :--- |
| Entry-Level | 1-3 years (Post-Fellowship) | $280,000 - $380,000 | Initial guaranteed salary, building a patient base, lower productivity initially. |
| Mid-Career | 4-10 years | $390,000 - $550,000 | Strong referral network, high patient volume, increased efficiency, potential for partnership track in private practice. |
| Senior/Experienced | 10+ years | $500,000 - $750,000+ | Peak efficiency, strong reputation, leadership roles, partnership income, potential for ancillary revenue streams. |
*Note: These ranges are estimates synthesized from industry reports and are highly dependent on the factors discussed in the next section.*
Beyond the Base Salary: Understanding the Full Compensation Package
A pediatric dermatologist's income is rarely just a flat salary. The total compensation package is a complex mix of components that can dramatically increase overall earnings.
- Base Salary: This is the guaranteed portion of your pay. In academic and some hospital-employed models, this makes up the bulk of compensation. In private practice, it might be a lower figure, with the majority of income coming from productivity bonuses.
- Production Bonuses (RVUs): This is the most common form of incentive pay. RVU stands for Relative Value Unit, a standardized measure used by Medicare and other payers to value the work involved in a physician's service. Every patient visit, procedure, and consultation has an assigned RVU value. Doctors are often paid a certain dollar amount per RVU generated above a specific threshold. An efficient dermatologist who performs many procedures can earn substantial bonuses.
- Sign-On Bonus: To attract a rare subspecialist like a pediatric dermatologist, hospitals and large group practices frequently offer significant sign-on bonuses, which can range from $25,000 to $100,000 or more.
- Profit Sharing / Partnership Income: For those in private practice, the ultimate financial goal is often partnership. Partners share in the profits of the entire practice, which can lead to the highest levels of income in the field. This comes with the added responsibility of managing the business.
- Comprehensive Benefits: These are a crucial, non-taxable part of compensation.
- Malpractice Insurance: A non-negotiable benefit, often with "tail coverage" which protects the physician even after they leave the practice. This can be worth $15,000-$30,000 per year.
- Health, Dental, and Vision Insurance: Comprehensive family plans.
- Retirement Plans: Robust 401(k) or 403(b) plans with generous employer matching contributions.
- Continuing Medical Education (CME) Allowance: An annual stipend of $5,000 - $15,000 to cover the cost of conferences, journals, and courses needed to maintain medical licenses.
- Relocation Allowance: Financial assistance for moving to accept a new position.
- Paid Time Off (PTO): Typically 4-6 weeks of vacation plus sick leave and time for CME.
When evaluating a job offer, it is critical to look beyond the base salary and calculate the total value of the entire compensation and benefits package.
---
Key Factors That Influence Salary

While the national averages provide a strong baseline, a pediatric dermatologist's actual salary is a dynamic figure influenced by a powerful combination of factors. Understanding these variables is essential for negotiating job offers and maximizing long-term earning potential. This is where a candidate can move from an average earner to a top-tier one.
###
Practice Setting and Employment Model
This is arguably the most significant factor determining a physician's compensation structure and ultimate take-home pay.
- Private Practice (Physician-Owned): This model offers the highest earning potential.
- Associate to Partner Track: A new dermatologist typically joins as an employee with a guaranteed base salary plus a productivity bonus. After 2-4 years, they may be offered the opportunity to "buy in" to the practice, becoming a partner.
- Partner: As a business owner, a partner's income is a share of the practice's profits. This directly ties their work and the practice's success to their income. An efficient partner in a well-managed practice can earn significantly more than their hospital-employed counterparts, often exceeding $600,000 - $800,000+. However, this comes with the responsibilities of business management, including staffing, billing, marketing, and overhead.
- Hospital-Owned or Multi-Specialty Group: This is a very common model offering a blend of security and earning potential.
- Structure: The physician is an employee of the hospital or a large corporate medical group. Compensation is typically a competitive base salary combined with a productivity bonus based on wRVUs (work Relative Value Units).
- Pros: Minimal administrative burden (the hospital handles billing, staffing, etc.), strong referral base from within the system, excellent benefits, and often more predictable hours.
- Cons: A ceiling on earning potential compared to private practice ownership. Salaries are high but less likely to reach the absolute highest echelons of the field. A typical range might be $350,000 to $550,000.
- Academic Medical Center: This path is for those passionate about teaching, research, and treating the most complex cases.
- Structure: The pediatric dermatologist is faculty at a university's medical school. Their time is split between clinical duties, teaching medical students and residents, and conducting research.
- Pros: Intellectually stimulating environment, opportunities to shape the next generation of doctors, access to cutting-edge technology and research funding, and often excellent benefits and retirement/pension plans.
- Cons: Compensation is almost always lower than in private or hospital-based practice. The focus is split, so clinical productivity is lower. An academic pediatric dermatologist might earn between $280,000 and $400,000, with variations based on academic rank (Assistant, Associate, or Full Professor).
###
Geographic Location
Where you practice has a profound impact on your salary, driven by a classic supply-and-demand economic model, as well as local cost of living and insurance reimbursement rates.
- High-Demand, Lower-Supply Areas: Rural and less "desirable" urban areas often offer the highest salaries. To attract a rare subspecialist, health systems in these regions must offer top-tier compensation packages, often with large sign-on bonuses and loan repayment assistance. It is not uncommon for salaries in the Midwest or Southeast to be higher than in ultra-competitive coastal cities.
- Major Metropolitan Areas (High Cost of Living): Cities like New York, Los Angeles, and San Francisco have very high costs of living, which does drive up salaries. However, these areas are also saturated with physicians, creating more competition. While salaries are high in absolute terms (e.g., $450,000+), they may not have the same purchasing power as a similar salary in a lower-cost state.
- Reimbursement Rates: State-specific Medicaid and private insurance reimbursement rates can also play a role. States with more favorable reimbursement schedules can support higher physician salaries.
Regional Salary Variation for Dermatologists (Illustrative)
| Region/State Example | Average Annual Salary (Approximate) | Analysis |
| :--- | :--- | :--- |
| Midwest (e.g., Wisconsin, Indiana) | $534,000 | Often a top-earning region due to high demand and lower specialist saturation. |
| Southeast (e.g., Alabama, Georgia) | $495,000 | Strong demand and growing populations support high compensation. |
| West (e.g., Utah, Oregon) | $482,000 | Competitive market with a mix of high-paying urban and rural opportunities. |
| Northeast (e.g., Massachusetts, New York) | $422,000 | High cost of living, but also high saturation of specialists can temper salary growth relative to other regions. |
*Source: Adapted from Doximity 2023 Physician Compensation Report data for general dermatology.*
###
Years of Experience and Reputation
As detailed in the previous section, experience is a primary driver of income growth. This is not just about longevity; it's about the tangible benefits that experience brings.
- Efficiency: An experienced dermatologist can see more patients in a day and perform procedures more quickly and accurately than a new graduate. In a productivity-based model, this directly translates to higher income.
- Reputation: Over time, a skilled and compassionate pediatric dermatologist builds a powerful reputation among local pediatricians and other specialists. This leads to a steady and high-quality stream of referrals, keeping their schedule full with the complex and interesting cases they are best equipped to handle. A doctor with a 3-month waiting list has more leverage and earning power than one struggling to fill their schedule.
- Leadership: Senior physicians often take on leadership roles, such as Medical Director of a clinic or Chief of a Dermatology department. These roles come with administrative stipends and further increase overall compensation.
###
Procedural vs. Medical Focus
Within pediatric dermatology, there can be a focus on either the "medical" side or the "procedural" side. While all practitioners do both, the balance can impact income.
- Procedural Focus: A practice that emphasizes procedures like laser therapy for vascular birthmarks, surgical excisions of cysts and nevi, and other hands-on treatments tends to be more lucrative. Procedures are reimbursed at a higher rate per unit of time than standard office visits (known as Evaluation & Management or E/M codes).
- Medical Focus: A practice centered on managing chronic conditions like eczema, psoriasis, or complex genodermatoses involves more cognitive work, patient education, and prescription management. While critically important, these activities are often reimbursed at a lower rate than procedures.
Many top earners strike a balance, maintaining a busy medical clinic while ensuring their schedule has dedicated time for well-reimbursed procedures.
###
Level of Education and Institutional Prestige
All pediatric dermatologists have an MD or DO, a dermatology residency, and a pediatric dermatology fellowship. The educational path is standardized and rigorous for everyone. However, the prestige of the institutions where one trains can have an impact, particularly on the first job out of fellowship.
- Top-Tier Programs: Graduating from a highly-ranked medical school, a prestigious dermatology residency program (like those at UCSF, NYU, or Stanford), and a renowned fellowship program can make a candidate more attractive to premier academic centers and top private practices. This can lead to higher starting salary offers and more opportunities.
- Research and Publications: A strong record of academic research, publications in major journals (like JAAD or JAMA Dermatology), and presentations at national conferences (like the AAD or SPD annual meetings) builds a national reputation. This is essential for a career in academia and can bolster negotiating power in any practice setting.
---
Job Outlook and Career Growth

The career outlook for pediatric dermatologists is exceptionally bright, characterized by high demand, low supply, and excellent long-term stability. This is a field where physicians can expect robust job security and consistent opportunities for professional and financial growth throughout their careers.
Demand Outpacing Supply: The Core of Job Security
The U.S. Bureau of Labor Statistics (BLS) projects that employment for all "Physicians and Surgeons" will grow by 3% from 2022 to 2032, which is about the average for all occupations. However, this general statistic vastly understates the reality for dermatology, and particularly for the subspecialty of pediatric dermatology. The true demand is much, much higher.
Several key factors create this favorable landscape:
1. The Residency Bottleneck: Dermatology is consistently one of the most competitive medical residencies to obtain. Each year, there are far more highly qualified medical school graduates applying than there are available residency spots. This severely limits the number of new dermatologists entering the workforce each year.
2. The Fellowship Funnel: After the dermatology residency bottleneck, an even smaller number of physicians go on to complete a 1-2 year fellowship in pediatric dermatology. The Society for Pediatric Dermatology (SPD) lists only a few dozen accredited fellowship programs in North America. This creates an even more pronounced scarcity of these highly trained subspecialists.
3. Increasing Public Awareness: Parents are more informed and proactive about their children's health than ever before. There is a greater awareness of the importance of early diagnosis and treatment of skin conditions, from monitoring moles to managing eczema, driving demand for specialist care.
4. Growing Complexity of Treatments: The advent of new biologics and advanced therapeutics for conditions like severe atopic dermatitis and psoriasis requires specialist knowledge for proper management, often beyond the scope of a general pediatrician or even a general dermatologist.
5. Lack of Coverage: There are entire states and large regions within the U.S. that have few, if any, board-certified pediatric dermatologists. Patients and their families often have to travel hundreds of miles and wait months for an appointment, highlighting the profound nationwide need.
The result of this imbalance is that newly graduated pediatric dermatologists are highly sought-after. They often receive multiple competitive job offers and can exercise significant choice in where and how they want to practice.
Emerging Trends Shaping the Future
The field is not static. Several trends are shaping the future of pediatric dermatology practice and creating new opportunities for growth.
- Teledermatology: The COVID-19 pandemic accelerated the adoption of virtual care. Teledermatology has proven to be an effective tool for follow-up appointments, managing chronic conditions, and providing access to care for families in remote areas. Proficiency in telemedicine is becoming a core skill and can provide flexible work arrangements.
- Advances in Therapeutics: The pipeline for new drugs, particularly biologics and Janus kinase (JAK) inhibitors for inflammatory conditions like atopic dermatitis, is robust. Staying at the forefront of these new treatments is essential and offers physicians powerful new tools to help their patients.
- Genetic Medicine: As our understanding of the genetic basis of skin disease (genodermatoses)
