For those drawn to medicine, few paths offer the unique blend of scientific challenge, profound human connection, and lifelong impact as pediatrics. It is a career dedicated to nurturing the health and well-being of society's most vulnerable, from the first cry of a newborn to the complex transition of adolescence. But beyond the calling, there lies a practical reality: the need for a stable, rewarding profession that justifies the immense investment of time, effort, and financial resources. This brings us to a crucial question for any aspiring doctor considering this specialty: What is a realistic pediatrician yearly salary?
This guide is designed to be your definitive resource, moving far beyond a single, misleading number. We will dissect the financial landscape of a career in pediatrics, exploring the national averages, the critical factors that cause salaries to fluctuate, and the long-term earning potential. We will provide a transparent, data-driven look at what you can expect to earn and how to maximize that potential throughout your career. I remember, early in my own professional journey, advising a young pre-med student who was torn between specialties. When we mapped out the career path for pediatrics, it wasn't just the salary that stood out, but the stability and consistent demand—a testament to the essential, non-negotiable role pediatricians play in every community. This career is not just a job; it's a pillar of our healthcare system.
Whether you are a high school student dreaming of a white coat, a medical student navigating specialty choices, or a resident preparing for your first contract, this article will provide the in-depth knowledge you need to make informed decisions. We will explore everything from the day-to-day responsibilities to the decade-long job outlook, giving you a complete picture of what it truly means—and what it truly pays—to be a pediatrician.
### Table of Contents
- [What Does a Pediatrician Do?](#what-does-a-pediatrician-do)
- [Average Pediatrician Yearly Salary: A Deep Dive](#average-pediatrician-yearly-salary-a-deep-dive)
- [Key Factors That Influence a Pediatrician's Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth for Pediatricians](#job-outlook-and-career-growth)
- [How to Become a Pediatrician: A Step-by-Step Guide](#how-to-get-started-in-this-career)
- [Conclusion: Is a Career in Pediatrics Right for You?](#conclusion)
What Does a Pediatrician Do?
A pediatrician is a medical doctor who specializes in the physical, emotional, and social health of children from birth through adolescence, typically up to age 18 or 21. They are the primary care physicians for the youngest members of our society, serving as the first point of contact for virtually all health concerns. Their expertise is broad, encompassing everything from preventative health and wellness to the diagnosis and treatment of acute and chronic illnesses.
The role of a pediatrician extends far beyond simply treating a sick child. They are trusted advisors, educators, and advocates for their patients. They guide parents through the crucial milestones of development, provide anticipatory guidance on nutrition and safety, and administer life-saving immunizations. They are trained to recognize the subtle signs of developmental delays, behavioral issues, and even social problems like abuse or neglect, making their role vital in the long-term health and safety of a child.
Core Responsibilities and Daily Tasks:
A pediatrician's work is incredibly varied, but most of their time is spent in direct patient care. Key responsibilities include:
- Well-Child Visits: Conducting routine physical examinations to monitor a child's growth and development against established milestones. These visits are crucial for preventative care, screenings, and administering vaccines.
- Diagnosing and Treating Illnesses: Managing a wide range of common childhood illnesses, from ear infections and strep throat to asthma and diabetes.
- Managing Chronic Conditions: Providing long-term care for children with chronic health issues such as allergies, eczema, ADHD, or more complex genetic disorders.
- Patient and Parent Education: A significant portion of the job involves educating parents and caregivers on topics like nutrition, sleep hygiene, safety precautions, and behavioral strategies.
- Administering Immunizations: Following the recommended vaccination schedule to protect children from preventable diseases like measles, polio, and tetanus.
- Maintaining Medical Records: Meticulously documenting patient histories, examinations, diagnoses, and treatment plans in Electronic Health Records (EHR) systems.
- Collaboration and Referrals: Working closely with other healthcare professionals and referring patients to pediatric subspecialists (like cardiologists or neurologists) when necessary.
### A Day in the Life of a General Pediatrician
To make the role more tangible, let's walk through a typical day for a pediatrician working in a busy outpatient private practice:
7:45 AM - Morning Huddle: The day begins before the first patient arrives. The pediatrician meets with the nursing staff and medical assistants to review the day's schedule. They discuss any complex cases, anticipate needs for specific vaccines or tests, and coordinate the workflow.
8:00 AM - 12:00 PM - Morning Appointments (Well-Child Focus): The morning is often packed with scheduled well-child visits. A typical schedule might include a 2-month-old for their first set of vaccines, a 2-year-old for a developmental screening, and a 9-year-old for their annual check-up and school physical form. Each visit involves a thorough exam, plotting growth charts, discussing developmental milestones with parents, and answering a myriad of questions ranging from picky eating to screen time limits.
12:00 PM - 1:00 PM - Administrative Time & Lunch: This hour is a whirlwind of activity. The pediatrician finishes charting from the morning's patients, reviews lab results that have come in, and returns urgent phone calls from parents. If they’re lucky, they grab a quick lunch at their desk.
1:00 PM - 4:30 PM - Afternoon Appointments (Sick-Visit Focus): The afternoon is typically reserved for acute or "sick" visits. These are often same-day appointments. The pediatrician might see a toddler with a high fever and a cough, a 7-year-old with a sore throat (requiring a strep test), and a teenager with a suspected sports injury. This part of the day requires sharp diagnostic skills and the ability to work efficiently under pressure. There might also be a follow-up visit for a child with recently diagnosed asthma to check on their response to a new inhaler.
4:30 PM - 5:30 PM (or later) - Wrap-Up: After the last patient leaves, the work isn't over. The pediatrician must complete all remaining patient charts, sign off on prescription refills, review non-urgent patient messages, and consult with colleagues about challenging cases. They might also have to make a call to a subspecialist to coordinate care for a patient. Some pediatricians also share "on-call" duties, meaning they may be responsible for handling patient calls after hours or on weekends, adding another layer to their responsibilities.
This snapshot reveals a profession that is fast-paced, intellectually stimulating, and deeply relational. It requires a unique combination of medical expertise, communication skills, patience, and a genuine love for working with children and their families.
Average Pediatrician Yearly Salary: A Deep Dive
Understanding the financial compensation for a pediatrician is a critical component of career planning, especially given the significant educational investment required. While pediatricians are among the lower-paid physician specialists, they still earn a substantial income that provides a high quality of life. The pediatrician yearly salary can vary widely based on numerous factors, which we will explore in the next section, but establishing a baseline is essential.
It's important to consult multiple authoritative sources to get a well-rounded picture, as methodologies can differ. For instance, some reports survey physicians directly, while others analyze job postings or employer-reported data.
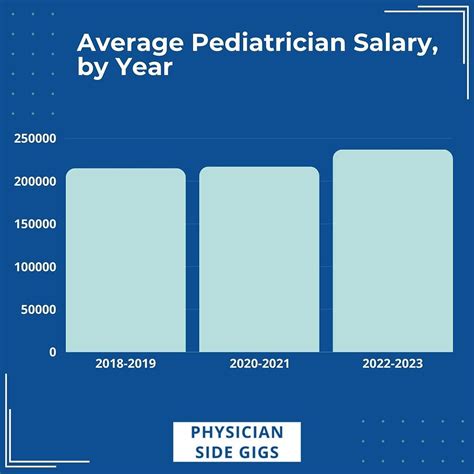
National Average Pediatrician Salary and Range
Here is a consolidated look at the average yearly salary for general pediatricians in the United States, based on the most recent data from leading sources:
- Medscape Physician Compensation Report 2023: This is one of the most comprehensive physician salary reports, based on survey data from over 10,000 physicians. It reports the average annual compensation for pediatricians at $251,000.
- U.S. Bureau of Labor Statistics (BLS): The BLS Occupational Employment and Wage Statistics (OEWS) program provides robust data based on employer surveys. As of May 2022, the BLS reported the mean annual wage for General Pediatricians at $203,240. The BLS also provides percentile data, which illustrates the typical salary range:
- 10th Percentile: $80,480 (Likely representing residents or part-time roles)
- 25th Percentile: $132,130 (Entry-level, post-residency)
- 50th Percentile (Median): $190,430
- 75th Percentile: >$239,200 (The BLS often caps the upper limit in its public data)
- 90th Percentile: >$239,200
- Doximity 2023 Physician Compensation Report: Doximity, a social network for healthcare professionals, places the average compensation for pediatricians at $242,832.
- Salary.com: This aggregator, which analyzes employer-reported data, shows a median salary for a "Physician - Pediatrics" at $226,701 as of late 2023, with a typical range falling between $197,501 and $269,701.
Summary of National Averages:
Across these primary sources, a realistic average salary for a general pediatrician in the U.S. falls somewhere between $200,000 and $250,000 per year. The significant range highlights the influence of experience, location, and practice setting.
### Salary Progression by Experience Level
A pediatrician's salary is not static; it grows significantly from residency to late-career stages. Here's a breakdown of the typical financial trajectory:
| Experience Level | Typical Timeframe | Estimated Yearly Salary Range | Key Notes |
| :--- | :--- | :--- | :--- |
| Pediatric Resident | Years 1-3 Post-Med School | $60,000 - $75,000 | Residents are trainee physicians. Salary is set by the hospital/institution and increases slightly each year of residency (PGY-1, PGY-2, PGY-3). |
| Entry-Level (Post-Residency) | Years 0-3 of Practice | $170,000 - $210,000 | This is the first attending physician role. Salaries often start with a guaranteed base, sometimes with a small production bonus. |
| Mid-Career | Years 4-10 of Practice | $210,000 - $260,000 | Physicians have become more efficient, built a patient panel, and may be eligible for productivity-based bonuses. Some may become partners in a private practice. |
| Senior/Experienced | Years 11+ of Practice | $240,000 - $300,000+ | At this stage, earning potential is maximized. Higher salaries are often tied to practice ownership, leadership roles, or high productivity in a hospital setting. |
*(Note: These are estimates for general pediatrics. Subspecialists will have a different trajectory, often with higher earning potential.)*
### Beyond the Base Salary: Understanding the Full Compensation Package
The annual salary is just one piece of the puzzle. A pediatrician's total compensation package is a comprehensive suite of benefits and incentives that add significant value. When evaluating a job offer, it's crucial to look beyond the base number.
Common Components of a Pediatrician's Compensation:
- Base Salary: The guaranteed annual income. In many hospital or large group settings, this is the primary form of payment.
- Production Bonuses (RVU-based): This is a critical component in many modern compensation models. Physicians earn Relative Value Units (RVUs) for each service they provide (e.g., a well-child check is worth more RVUs than a simple sick visit). After meeting a certain threshold, the physician earns a bonus for each additional RVU generated. This directly rewards productivity.
- Signing Bonus: A one-time, lump-sum payment offered to entice a physician to join a practice or hospital. These can range from $10,000 to $50,000 or more, especially in underserved areas.
- Relocation Assistance: A stipend to cover the costs of moving to a new city for a job.
- Student Loan Repayment: A highly valuable incentive. Some employers, particularly in rural or underserved areas and non-profit hospitals, offer significant student loan repayment assistance, sometimes totaling over $100,000 over several years.
- Malpractice Insurance: Employer-paid malpractice coverage is standard. It's important to know the type of policy offered ("claims-made" vs. "occurrence") and whether tail coverage is included.
- Health and Disability Insurance: Comprehensive health, dental, vision, and both short-term and long-term disability insurance are standard benefits.
- Retirement Plans: Access to a 401(k) or 403(b) plan with an employer match is a key part of long-term financial planning. The employer match is essentially free money and a significant part of the total compensation.
- Continuing Medical Education (CME) Stipend: An annual allowance (e.g., $2,000 - $5,000) and paid time off to attend conferences and courses required to maintain medical licensure.
- Paid Time Off (PTO): Includes vacation, sick days, and holidays. Typically ranges from 4 to 6 weeks per year.
- Profit Sharing / Partnership Track: In private practices, there is often a pathway to becoming a partner after a few years. Partners share in the profits of the practice, leading to significantly higher income potential than that of an employed physician.
When all these elements are combined, the total value of a pediatrician's compensation package is substantially higher than the base salary alone.
Key Factors That Influence a Pediatrician's Salary
While we've established a baseline salary range of $200,000 to $250,000, the reality is that a pediatrician yearly salary is not one-size-fits-all. It is a highly variable figure influenced by a complex interplay of professional choices, geographic location, and market demands. Understanding these factors is the key to maximizing your earning potential throughout your career. This section provides an exhaustive breakdown of the elements that will have the most significant impact on your paycheck.
---
### `
` 1. Area of Specialization and Subspecialty Training
The single most impactful factor in a physician's salary is their choice of specialty and subspecialty. Within pediatrics, there is a vast difference in earning potential between a generalist and a highly trained subspecialist.
- General Pediatrics: As we've detailed, general pediatricians form the foundation of children's healthcare. Their average salary, as reported by Medscape, is $251,000. They have the broadest scope of practice but are on the lower end of the physician pay scale.
- Pediatric Subspecialties: After completing a three-year pediatric residency, a physician can choose to pursue a fellowship in a specific area. These fellowships typically last three years or more and lead to board certification in that subspecialty. This additional training and expertise command a significant salary premium.
Here is a comparison of average annual salaries for various pediatric subspecialties, demonstrating the substantial financial impact of fellowship training (Data primarily sourced from Medscape and Doximity reports):
| Subspecialty | Average Annual Salary | Description |
| :--- | :--- | :--- |
| Pediatric Cardiology | $350,000 - $450,000+ | Manages congenital and acquired heart conditions in children. Often involves procedural work. |
| Pediatric Critical Care (PICU) | $330,000 - $420,000+ | Works in the Pediatric Intensive Care Unit, managing critically ill or injured children. |
| Neonatology (NICU) | $320,000 - $400,000+ | Cares for sick or premature newborn infants in the Neonatal Intensive Care Unit. |
| Pediatric Gastroenterology | $300,000 - $380,000+ | Treats digestive system, liver, and nutritional problems. Often performs procedures like endoscopies. |
| Pediatric Hematology/Oncology | $280,000 - $350,000+ | Treats children with cancer and blood disorders. Demanding but highly rewarding. |
| Pediatric Pulmonology | $270,000 - $330,000+ | Manages breathing and lung disorders, such as severe asthma and cystic fibrosis. |
| Pediatric Emergency Medicine | $260,000 - $320,000+ | Works in the emergency department, treating acute illnesses and injuries in children. |
| Developmental-Behavioral Peds| $230,000 - $280,000+ | Focuses on developmental delays and behavioral problems like ADHD and autism spectrum disorder. |
| Pediatric Infectious Disease | $220,000 - $270,000+ | Manages complex and rare infections. More academic and less procedural, hence lower pay. |
| General Pediatrics | $251,000 | Baseline for comparison. |
The trend is clear: subspecialties that are procedure-heavy (cardiology, gastroenterology) or involve high-acuity intensive care (critical care, neonatology) command the highest salaries. This is due to the higher reimbursement rates for procedures and the intense nature of the work.
---
### `
` 2. Geographic Location
Where you choose to practice medicine has a profound impact on your salary. This variation is driven by supply and demand, cost of living, and the local healthcare market dynamics. Intriguingly, the highest salaries are often found not in the major coastal cities but in regions with a greater need for physicians.
State-by-State and Regional Variations:
According to multiple compensation reports, including those from Doximity and Medscape, states in the Southeast and Midwest often offer the highest compensation for physicians, including pediatricians. This is done to attract talent away from the more traditionally "desirable" (but oversaturated) coastal markets.
- Highest-Paying States for Pediatricians (often exceeding $270,000 - $300,000 on average):
- Alaska
- South Dakota
- Wyoming
- Mississippi
- Alabama
- Tennessee
- Oklahoma
- Indiana
- Lowest-Paying States for Pediatricians (often below $200,000 on average):
- Maryland
- Massachusetts
- New York
- Colorado
- District of Columbia (D.C.)
Urban vs. Rural vs. Suburban:
- Rural Areas: Often offer the highest starting salaries, significant signing bonuses, and generous loan repayment options. This is a direct strategy to combat physician shortages. While the base salary is high, cultural amenities and school options may be limited.
- Suburban Areas: Can represent a sweet spot, offering strong salaries that are competitive with urban centers but with a lower cost of living. These areas have high demand due to large populations of young families.
- Major Urban Centers (e.g., NYC, LA, Boston): These markets are highly saturated with physicians due to the presence of prestigious academic centers and cultural attractions. The high supply of doctors drives down compensation. When coupled with an extremely high cost of living, the effective take-home pay can be significantly lower than in other regions.
---
### `
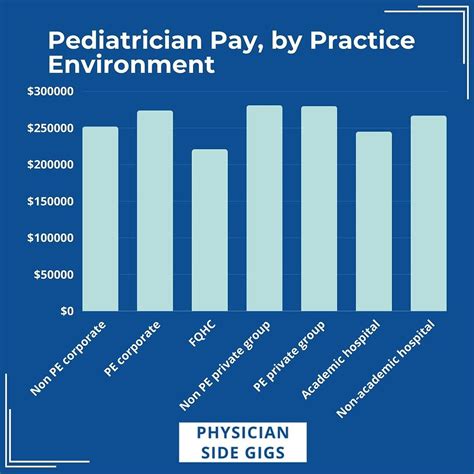
` 3. Practice Setting and Employment Model
The type of organization you work for is another crucial determinant of your income and overall work-life balance.
- Private Practice (Physician-Owned): This model offers the highest long-term earning potential.
- Employed Physician: When first joining, you'll work as an employee with a guaranteed salary, often with a 2-4 year track to partnership.
- Partner/Owner: Once you become a partner, you share in the practice's profits. Your income is directly tied to the success of the business. This can push a general pediatrician's income well over $300,000 or $400,000, but it comes with the responsibilities of running a business: managing staff, payroll, billing, and overhead.
- Hospital or Health System Employment: This is the most common employment model for new physicians.
- Pros: Offers a stable, predictable salary, excellent benefits, no administrative burden, and built-in infrastructure. The hospital handles billing, staffing, and overhead.
- Cons: Less autonomy and a lower income ceiling compared to practice ownership. Compensation is often strictly based on productivity (RVUs), which can create pressure to see a high volume of patients. Salaries typically fall within the national average range of $220,000 to $270,000.
- Academic Medical Centers: These are hospitals affiliated with a medical school.
- Pros: Opportunities for teaching medical students and residents, conducting research, and treating complex cases. This path carries significant prestige.
- Cons: Salaries are consistently lower than in private practice or general hospital employment, often by $30,000 to $50,000 or more per year. The institution justifies this with the non-monetary rewards of academia.
- Federally Qualified Health Centers (FQHCs) & Public Health:
- These centers serve medically underserved populations. Salaries are generally on the lower end of the spectrum. However, they come with a major benefit: eligibility for significant federal and state loan forgiveness programs, like the National Health Service Corps (NHSC), which can be worth hundreds of thousands of dollars.
---
### `
` 4. Years of Experience and Career Trajectory
As outlined in the previous section, experience level directly correlates with income. The salary growth curve is steepest in the first decade of practice.
- Residency (PGY 1-3): Stipends are low, around $60,000-$75,000.
- First Attending Job (Years 1-3): A massive jump in income to the $170,000-$210,000 range. This period is about building clinical speed and confidence.
- Mid-Career (Years 4-10): Efficiency increases, patient panels are full, and compensation models often shift to be more productivity-based. This is where salaries grow into the $210,000-$260,000 range. This is also the typical timeframe for making partner in a private practice.
- Late Career (Years 11+): For employed physicians, salaries tend to plateau. For practice owners or those in leadership roles (e.g., Medical Director, Chief of Pediatrics), income can continue to grow. An experienced practice partner can comfortably earn over $300,000.
---
### `
` 5. In-Demand Skills and Other Influences
Beyond the major categories, several other skills and factors can provide a financial edge:
- Productivity (Work Ethic): In models that heavily use RVUs, a pediatrician who is efficient and willing to see more patients per day will earn significantly more than a colleague who prefers a slower pace.
- Business Acumen: For those in private practice, understanding the business side of medicine—billing codes, overhead management, and marketing—directly translates to higher profits and personal income.
- Telehealth Proficiency: The rise of virtual care has created new opportunities. Pediatricians who are comfortable and efficient with telehealth platforms can increase their patient volume and accessibility.
- Leadership Roles: Taking on administrative responsibilities, such as becoming the lead physician of a clinic or a department chair, comes with a stipend or salary increase.
- Multilingual Abilities: In diverse communities, being fluent in a second language (especially Spanish) can make a candidate more attractive to employers and may command a higher salary or bonus.
By strategically considering these five key areas—specialization, location, practice type, experience, and unique skills—an aspiring or practicing pediatrician can actively shape their financial future.
Job Outlook and Career Growth for Pediatricians
After investing over a decade in education and training, a prospective
