Introduction

Imagine standing at the intersection of life and death, where every decision carries immense weight and your expertise is the fine line between a patient's recovery and demise. This is the high-stakes, deeply rewarding world of the Pulmonary Critical Care (PCCM) physician. For those drawn to medicine's most intense challenges—diagnosing complex lung diseases and managing the sickest patients in the intensive care unit (ICU)—this dual specialty offers not only profound personal satisfaction but also exceptional financial compensation. The average pulmonary critical care salary reflects the years of rigorous training, the demanding nature of the work, and the critical need for these specialists in our healthcare system, with most physicians earning well over $400,000 annually.
As a career analyst, I've seen countless professionals weigh their options, but few paths offer such a direct and tangible impact. I vividly recall the calm, steady presence of the pulmonary critical care physician who managed my own father's care in the ICU. In a whirlwind of fear and uncertainty, she was the anchor, translating complex medical jargon into human terms and orchestrating a symphony of life-sustaining treatments. It's this unique blend of intellectual rigor, procedural skill, and profound human connection that defines the profession and justifies its high earning potential.
This guide is designed to be your definitive resource, whether you're a medical student contemplating specialties or a resident finalizing your fellowship plans. We will dissect every component of a pulmonary critical care salary, explore the factors that can significantly increase your earnings, and map out the exact steps required to enter this elite field.
### Table of Contents
- [What Does a Pulmonary Critical Care Physician Do?](#what-they-do)
- [Average Pulmonary Critical Care Salary: A Deep Dive](#salary-deep-dive)
- [Key Factors That Influence Salary](#key-factors)
- [Job Outlook and Career Growth](#job-outlook)
- [How to Get Started in This Career](#how-to-start)
- [Conclusion: Is a Career in Pulmonary Critical Care Right for You?](#conclusion)
What Does a Pulmonary Critical Care Physician Do?
A Pulmonary Critical Care physician is a medical doctor (MD or DO) who has completed advanced, dual-specialty training in both pulmonology and critical care medicine. This unique combination equips them to be experts in two distinct but often overlapping domains:
1. Pulmonology: The branch of medicine focused on diseases of the respiratory tract. This includes conditions like asthma, Chronic Obstructive Pulmonary Disease (COPD), lung cancer, interstitial lung disease, and pulmonary hypertension.
2. Critical Care Medicine (or Intensivist Medicine): The specialization focused on diagnosing and treating life-threatening conditions in critically ill patients, typically within an Intensive Care Unit (ICU). This involves managing organ failure, severe infections (sepsis), acute respiratory distress syndrome (ARDS), and shock.
This dual certification means their work environment is incredibly varied. A PCCM specialist's time is often split between the outpatient clinic, the general hospital floors for consultations, and the high-acuity environment of the ICU.
Core Responsibilities and Daily Tasks:
- Diagnosis and Management of Lung Disease: Conducting patient histories, physical exams, and interpreting diagnostic tests like pulmonary function tests (PFTs), chest X-rays, and CT scans in an outpatient clinic setting.
- Leading ICU Rounds: Functioning as the primary attending physician for patients in the ICU, leading a multidisciplinary team of residents, nurses, pharmacists, and respiratory therapists to create and execute daily care plans.
- Performing Advanced Procedures: PCCM is a procedure-heavy field. Common procedures include:
- Bronchoscopy: Using a flexible scope to visualize the airways, take biopsies, or clear obstructions.
- Endobronchial Ultrasound (EBUS): An advanced bronchoscopy technique to biopsy lymph nodes in the chest for cancer staging.
- Thoracentesis: Draining fluid from the space around the lungs.
- Intubation: Placing a breathing tube into a patient's trachea to connect them to a mechanical ventilator.
- Central Line Placement: Inserting large IVs into major veins for medication delivery and monitoring.
- Ventilator Management: This is a cornerstone of critical care. Physicians meticulously adjust ventilator settings to support a patient's breathing without causing further lung injury.
- Family Communication: A crucial and challenging part of the job is communicating with the families of critically ill patients, explaining complex prognoses, and guiding them through difficult end-of-life decisions.
- Consultations: Providing expert advice to other physicians in the hospital on patients with complex respiratory or critical illness issues.
### A "Day in the Life" Example
To make this tangible, a PCCM physician's schedule often follows a block model, such as one week of ICU service followed by three weeks of outpatient clinic and hospital consults.
A Typical "ICU Week" Day:
- 7:00 AM: Arrive at the hospital. Get a detailed "sign-out" from the overnight physician or resident on all ICU patients. Review overnight events, new lab results, and imaging studies.
- 8:00 AM - 9:00 AM: Pre-round on the most critical patients, performing a quick physical exam and reviewing ventilator settings.
- 9:00 AM - 12:00 PM: Lead multidisciplinary rounds. The team moves from room to room, discussing each patient's status, progress, and creating a detailed plan for the next 24 hours.
- 12:00 PM - 1:00 PM: A quick lunch, often while catching up on charting or responding to urgent pages.
- 1:00 PM - 4:00 PM: "Procedure time." This block is dedicated to performing scheduled or emergent procedures like bronchoscopies, placing lines, or intubations. It's also when family meetings are often held.
- 4:00 PM - 6:00 PM: Follow up on care plans, check new test results, and update patient charts. Handle new admissions to the ICU from the emergency department or other hospital floors.
- 6:00 PM - 7:00 PM: "Sign-out." Give a thorough report to the on-call or nighttime physician, ensuring a safe handoff of care. This day is intense, focused, and requires constant mental engagement.
A Typical "Clinic Week" Day:
- 8:30 AM: Arrive at the outpatient clinic. Review charts for the morning's patients—a mix of new consultations for issues like a chronic cough or shortness of breath, and follow-ups for patients with COPD, asthma, or sleep apnea.
- 9:00 AM - 12:00 PM: See patients. Each appointment is 20-40 minutes and involves a detailed history, exam, and review of PFTs or sleep studies.
- 12:00 PM - 1:00 PM: Lunch, often combined with reviewing and signing off on hospital consultation notes from the previous day.
- 1:00 PM - 4:30 PM: Afternoon patient sessions. This block might also include interpreting a batch of pulmonary function tests for the clinic.
- 4:30 PM - 5:30 PM: Finalize charts, answer patient messages through the electronic health record, and handle prescription refills. This day is more predictable but requires deep knowledge of chronic disease management.
Average Pulmonary Critical Care Salary: A Deep Dive
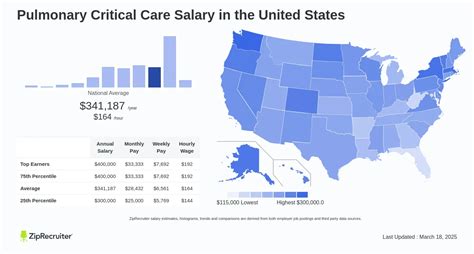
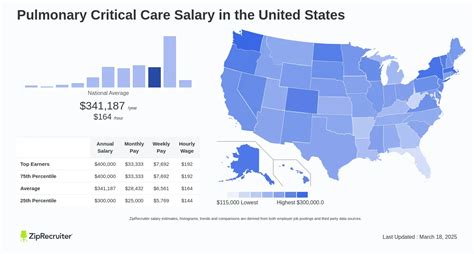
The compensation for pulmonary critical care physicians is among the highest in the medical field, a direct reflection of the extensive training required and the high-stakes nature of the work. Salary figures can vary widely based on numerous factors, but authoritative sources provide a clear picture of the earning potential.
According to the 2023 Medscape Physician Compensation Report, one of the most respected industry benchmarks, Pulmonologists earn an average of $408,000 per year. It's crucial to note that this figure often includes physicians who practice only pulmonology. Those with the dual certification in critical care, who take on the added responsibility and intensity of ICU work, typically command higher salaries.
Other major salary aggregators provide corroborating data, offering a comprehensive view of the salary range:
- Salary.com reports a median salary for a Pulmonary Critical Care Physician at $408,448 as of late 2023, with the typical range falling between $355,334 and $486,935.
- Doximity's 2023 Physician Compensation Report places Pulmonary Medicine at number 13 on its list of highest-paid specialties, with an average annual compensation of $433,024.
- Payscale.com indicates an average base salary closer to $330,000, but this figure may not fully capture the significant impact of bonuses and productivity incentives, which are a major part of a PCCM physician's total compensation.
The Bottom Line: A newly trained PCCM physician can realistically expect to start in the $350,000 to $400,000 range, with experienced physicians in lucrative practice settings easily surpassing $500,000 to $600,000 or more annually.
### Salary Brackets by Experience Level
Like any profession, income in PCCM grows significantly with experience, expertise, and reputation. The career trajectory sees a steep increase after fellowship, followed by steady growth.
| Experience Level | Typical Years Post-Fellowship | Typical Annual Salary Range | Key Characteristics |
| :--- | :--- | :--- | :--- |
| Early Career | Years 1-5 | $350,000 - $425,000 | Focus is on building clinical skills, speed, and efficiency. Often working as an employee of a hospital or large group. |
| Mid-Career | Years 6-15 | $425,000 - $550,000 | Has become highly efficient. May take on leadership roles (e.g., ICU Medical Director) or become a partner in a private practice, increasing income potential. |
| Senior/Late Career | Years 16+ | $500,000 - $650,000+ | A recognized expert. Often holds major administrative roles (e.g., Department Chair) or is a senior partner in a successful private practice. Earnings can be very high but may taper if clinical hours are reduced. |
*Source: Analysis of data from Medscape, Doximity, and Salary.com, combined with industry insights.*
### Breakdown of Compensation Components
A physician's "salary" is rarely just a flat number. The total compensation package is a complex mix of a base salary and various incentives designed to reward productivity and commitment.
- Base Salary: This is the guaranteed portion of your income. In hospital-employed and academic models, this makes up the bulk of the pay. In private practice, the base salary might be lower, with a greater emphasis on productivity.
- Productivity Bonuses (wRVU Model): This is the most significant variable component of a PCCM physician's income. Most health systems track physician work using Work Relative Value Units (wRVUs). Each patient encounter, procedure, and consultation is assigned an RVU value by Medicare. Physicians are often paid a certain dollar amount per wRVU generated above a set threshold. Because PCCM is a procedure-heavy specialty (bronchoscopies, lines, etc.) and involves caring for high-acuity (high-RVU) patients in the ICU, the potential for high productivity bonuses is substantial.
- Sign-On Bonus: To attract top talent, especially in less desirable geographic locations, hospitals and practices often offer a substantial one-time payment upon signing a contract. These can range from $20,000 to $75,000 or more.
- Call Pay: Physicians are often paid an extra stipend for being on-call for the hospital or ICU overnight or on weekends. This can be a per-diem rate or an hourly rate if called in to manage a patient.
- Quality Bonuses: An increasing number of health systems are tying a portion of compensation to quality metrics, such as patient outcomes, readmission rates, or patient satisfaction scores.
- Retirement Contributions: Employer contributions to 401(k) or 403(b) plans are a significant part of the overall financial picture. Generous plans can add tens of thousands of dollars to your net worth annually.
- CME Allowance: An annual stipend (typically $3,000 - $5,000) provided to cover the costs of continuing medical education (CME), such as attending conferences or subscribing to medical journals.
- Malpractice Insurance: A crucial and expensive benefit. The employer almost always covers the full cost of "claims-made" or "occurrence-based" malpractice insurance, which can be valued at $15,000 to $30,000+ per year.
Understanding this full compensation structure is vital. A job offer with a lower base salary but a highly lucrative wRVU model and excellent benefits could ultimately be more financially rewarding than a job with a higher, but flat, base salary.
Key Factors That Influence Pulmonary Critical Care Salary

While the national averages provide a solid baseline, your individual earning potential as a PCCM specialist is heavily influenced by a specific set of variables. Mastering these factors is the key to maximizing your career-long income. This is the most critical section for understanding the nuances of compensation in this field.
###
Practice Setting: The Single Biggest Driver of Income
Where you choose to work—the type of organization that signs your paycheck—is arguably the most significant factor determining your salary. Each setting offers a different balance of income, autonomy, workload, and lifestyle.
1. Private Practice (Physician-Owned Group)
- Salary Potential: Highest. $500,000 - $800,000+ is achievable for partners.
- Structure: Physicians are owners or partners in the business. After an initial period as an employee (typically 2-3 years on a "partnership track"), physicians can "buy in" to the practice.
- Pros:
- High Autonomy: You and your partners control business decisions, scheduling, and clinical protocols.
- Direct Financial Reward: Your hard work directly translates to higher income. You keep the profits generated from your clinical work and ancillary services.
- Ancillary Services: Private practices can generate substantial extra revenue by owning their own pulmonary function testing labs, sleep labs, or imaging equipment. This is a major income amplifier not available in other models.
- Cons:
- Administrative Burden: You are a business owner. This means dealing with billing, coding, HR, payroll, and marketing.
- Financial Risk: You share in the practice's expenses and financial downturns. The initial buy-in can be expensive.
- Less Predictable Schedule: Call responsibilities can be more demanding in smaller groups.
2. Hospital-Employed Model
- Salary Potential: Strong and stable. $400,000 - $550,000.
- Structure: You are a direct employee of a hospital or a large, integrated health system (e.g., Kaiser Permanente, HCA Healthcare).
- Pros:
- Stability and Security: You receive a regular paycheck, and the hospital handles all administrative and business aspects.
- Excellent Benefits: Hospitals typically offer robust benefits packages, including generous retirement plans, health insurance, and malpractice coverage.
- Work-Life Balance: Often features more predictable schedules, such as a "7 on, 7 off" block schedule for ICU work, providing dedicated time off.
- Cons:
- Less Autonomy: You must adhere to hospital administration's protocols, productivity targets, and scheduling mandates.
- Income Ceiling: While the salary is high, it's generally capped and lacks the unlimited upside potential of private practice ownership.
3. Academic Medical Center
- Salary Potential: Lowest of the main three. $325,000 - $450,000.
- Structure: Employed by a university-affiliated hospital. The role is a mix of clinical care, teaching residents and medical students, and conducting research.
- Pros:
- Prestige and Intellectual Stimulation: You are at the cutting edge of medicine, managing the most complex and rare cases.
- Teaching and Research: The opportunity to educate the next generation of physicians and contribute to scientific advancement is a primary driver for many.
- Excellent Benefits: Similar to hospital-employed roles, often with added perks like tuition assistance for family members.
- Cons:
- "Academic Discount": The salary is almost always lower than in private or community hospital settings. This is the trade-off for the non-clinical aspects of the job.
- Bureaucracy: University and hospital hierarchies can be complex and slow to navigate.
- "Publish or Perish": There is often pressure to secure research grants and publish papers to advance in academic rank (e.g., from Assistant to Associate Professor).
4. Locum Tenens (Temporary Work)
- Salary Potential: Extremely high on a per-diem basis. Can equate to $600,000+ if working full-time.
- Structure: You work as an independent contractor, filling in for physicians who are on vacation, leave, or in hospitals with staffing shortages. Assignments can last from a weekend to several months.
- Pros:
- Top-Tier Pay: Daily rates can be $2,000 - $3,500 or more.
- Ultimate Flexibility: You choose when and where you want to work.
- Travel Opportunities: A chance to experience different practice settings and parts of the country.
- Cons:
- No Stability or Benefits: You are responsible for your own health insurance, retirement, and malpractice insurance (though the staffing agency often provides the latter). There is no paid time off.
- Constant Change: Always being the "new person" can be professionally and personally isolating.
###
Geographic Location: Supply and Demand in Action
Physician salaries do not follow typical cost-of-living patterns. Often, the highest salaries are found in areas with the greatest need and the least competition, not in major coastal cities.
- Highest Paying Regions/States: According to Doximity and Medscape data, the states in the Southeast (e.g., Alabama, Georgia, Florida), Midwest (e.g., Indiana, Wisconsin, Ohio), and some Mountain West states consistently offer higher-than-average compensation.
- Why? There is a higher demand due to physician shortages, a less saturated market of specialists, and often a higher burden of chronic disease. A practice in rural Wisconsin might offer $50,000-$100,000 more per year than one in Boston to attract a qualified PCCM physician.
- Lower Paying Regions/States: The Northeast (e.g., Massachusetts, New York, Maryland) and some parts of the West Coast (e.g., California) tend to offer lower salaries.
- Why? These areas have a high concentration of academic medical centers and are considered highly desirable places to live, leading to a surplus of physicians competing for jobs. The salary is depressed by this market saturation.
- Urban vs. Rural Divide: Within any given state, rural and suburban areas will almost always pay more than major metropolitan centers. The "rural premium" is a significant and consistent factor across all medical specialties.
###
Years of Experience: The Path to Senior Partner
As detailed in the salary table, experience is a linear driver of income, but the *type* of experience matters.
- Early Career (Years 1-5): The focus is on transitioning from a trainee to an autonomous and efficient clinician. Your wRVU production will naturally increase during this time, leading to higher bonuses. The biggest salary jump often occurs when you leave your first job for your second, as you can now negotiate as an experienced attending physician.
- Mid-Career (Years 6-15): This is the peak earning phase. Clinically, you are at your most efficient. This is also when physicians often step into leadership roles that come with additional stipends, such as:
- ICU Medical Director: Adds $25,000 - $75,000 per year.
- Pulmonary Department Chief: Adds $50,000 - $100,000+ per year.
- Making Partner: In private practice, this is when you transition from a salaried employee to a full partner, sharing in the practice's profits. This can increase total compensation by 30-50% or more.
- Late Career (Years 16+): Income can remain high or even grow, especially for those in major leadership or ownership positions. However, some physicians may choose to scale back their clinical hours or drop the more demanding ICU component of their practice, which can lead to a planned decrease in income in exchange for a better lifestyle.
###
Sub-Specialization and Procedural Skills
Within the dual field of PCCM, further specialization can dramatically impact your value and income.
- Interventional Pulmonology (IP): This is the most lucrative sub-specialty. IP involves performing advanced, minimally invasive procedures to diagnose and treat lung cancer and other complex airway and pleural diseases (e.g., robotic bronchoscopy, tumor ablation, placing stents in the airway). It requires an additional year of fellowship training. Because these procedures are complex and highly reimbursed, an Interventional Pulmonologist can earn $100,000 to $200,000+ more per year than a general PCCM physician.
- Sleep Medicine: While it also requires an additional fellowship year, specializing in sleep medicine (and often running a sleep lab) can be a significant revenue stream, particularly in a private practice setting.
- Advanced Procedural Competence: Even without a formal IP fellowship, becoming the "go-to" physician in your group for difficult procedures like Endobronchial Ultrasound (EBUS) or navigational bronchoscopy will directly increase your wRVU production and, therefore, your bonus potential.
###
Board Certification and Educational Pedigree
- Dual Board Certification: To be marketable for top jobs, you *must* be board certified (or board eligible) by the American Board of Internal Medicine (ABIM) in both Pulmonary Disease and Critical Care Medicine. Lacking one of these certifications severely limits your job prospects and earning potential.
- Prestige of Training: While every US-trained physician is held to a high standard, graduating from a highly prestigious residency and fellowship program (e.g., Johns Hopkins, Massachusetts General Hospital, UCSF) can give you a competitive edge, particularly for sought-after academic positions or elite private practice groups. It acts as a powerful signal of quality to potential employers.
Job Outlook and Career Growth

The career outlook for pulmonary critical care physicians is exceptionally strong and is projected to remain so for the foreseeable future. This robust demand is driven by several powerful, long-term demographic and healthcare trends.
The U.S. Bureau of Labor Statistics (BLS) projects that employment for all physicians and surgeons will grow by 3% from 2022 to 2032. However, this aggregate figure masks the much higher demand for certain specialties. For PCCM, the outlook is significantly more bullish due to the following factors:
1. The Aging Population: The "baby boomer" generation is entering its 70s and 80s, an age where chronic diseases escalate. This directly increases the prevalence of conditions managed by pulmonologists, such as COPD, idiopathic pulmonary fibrosis (IPF), and lung cancer. An older population also means more frequent and complex hospitalizations, driving the need for