Introduction

The human brain, a three-pound universe of staggering complexity, represents the final frontier of medicine. To be a neurosurgeon is to be an explorer, a mechanic, and a guardian of this frontier. It is a profession synonymous with immense prestige, intellectual rigor, and profound responsibility. For those drawn to this demanding field, the question of compensation is not just a practical consideration but a reflection of the years of dedication, unparalleled skill, and the life-altering impact they have. When aspiring medical professionals research the potential salary for neurosurgeon roles, they are looking at one of the highest-paid professions in the world—a figure that mirrors the Everest-like climb required to reach its peak.
The financial rewards are indeed significant, with average annual salaries comfortably exceeding half a million dollars and top earners in private practice potentially reaching well into seven figures. However, this journey is not for the faint of heart. It demands more than a decade of post-secondary education and grueling residency training where 80-hour work weeks are the norm. In my two decades as a career analyst specializing in high-stakes professions, I've rarely encountered a field that so perfectly embodies the principle of high risk, high reward. I once had the privilege of interviewing a pediatric neurosurgeon who, after describing a 14-hour surgery to remove a tumor from a five-year-old's brainstem, spoke not of the salary, but of the moment he could tell the parents their child had a future. That conversation solidified the reality that for these elite specialists, the compensation, while extraordinary, is often secondary to the calling.
This comprehensive guide will dissect every facet of a neurosurgeon's career, from the intricate daily responsibilities to the complex factors that dictate their earning potential. We will explore the demanding path to becoming a neurosurgeon, the future outlook for the profession, and provide a data-driven, authoritative analysis of the salary you can expect at every stage of this remarkable career.
### Table of Contents
- [What Does a Neurosurgeon Do?](#what-does-a-neurosurgeon-do)
- [Average Neurosurgeon Salary: A Deep Dive](#average-neurosurgeon-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
What Does a Neurosurgeon Do?

The title "neurosurgeon" often conjures images of a steely-eyed physician performing delicate, high-stakes surgery on the brain. While this is a critical component of the job, it represents only a fraction of their wide-ranging responsibilities. A neurosurgeon is a highly specialized medical doctor who diagnoses and surgically treats disorders affecting the central, peripheral, and autonomic nervous systems. This includes the brain, spinal cord, skull, and the vast network of nerves that extend throughout the body.
Their expertise is not limited to the operating room (OR). A significant portion of their work is diagnostic and consultative. They are masters of interpreting complex imaging like MRIs, CT scans, and PET scans to pinpoint tumors, aneurysms, hemorrhages, and degenerative diseases. They work closely with other specialists, particularly neurologists (who treat nervous system disorders with non-surgical methods), oncologists, and radiologists, to develop comprehensive treatment plans. Many conditions that fall under a neurosurgeon's care, such as certain types of back pain or minor head trauma, are managed non-surgically with medication, physical therapy, or observation. The decision *not* to operate is often as critical as the decision to proceed with surgery.
Core Responsibilities and Daily Tasks:
- Patient Consultation and Diagnosis: Meeting with patients to understand their symptoms, review their medical history, and perform neurological examinations. This is where they build rapport and explain complex medical conditions in understandable terms.
- Surgical Planning and Execution: When surgery is necessary, the neurosurgeon meticulously plans the procedure. This can range from minimally invasive spine surgery to complex multi-hour craniotomies for tumor removal or aneurysm clipping.
- Pre- and Post-Operative Care: Managing patients before surgery to ensure they are medically optimized, and overseeing their recovery afterward in the intensive care unit (ICU) and on the surgical floor. This includes managing pain, monitoring for complications, and coordinating with rehabilitation teams.
- Emergency and Trauma Care: Neurosurgeons are often on-call for emergencies, responding to traumatic brain injuries (TBIs), spinal cord injuries, and acute strokes that require immediate surgical intervention.
- Research and Academics: Many neurosurgeons, particularly those in academic medical centers, are actively involved in research to advance the understanding of neurological diseases and develop new treatment techniques. They may also teach medical students and train the next generation of neurosurgical residents.
- Administrative Duties: Like all physicians, neurosurgeons spend a considerable amount of time on administrative tasks, including charting patient records, dictating operative notes, communicating with insurance companies, and attending departmental meetings.
### A Day in the Life: Dr. Eleanor Vance, Attending Neurosurgeon
To make this tangible, let's walk through a hypothetical but typical day for a hospital-employed neurosurgeon.
- 5:30 AM: The alarm rings. Dr. Vance is at the hospital by 6:15 AM. She starts her day with "rounding" on her post-operative patients in the neuro-ICU and on the surgical ward. She reviews overnight events, checks vital signs, examines patients, and adjusts their care plans with the resident team.
- 7:30 AM: She scrubs in for her first scheduled case: a lumbar microdiscectomy for a patient with debilitating sciatica. This is a relatively routine, minimally invasive spine surgery that will take about 90 minutes.
- 9:30 AM: After speaking with the patient's family, she quickly grabs a coffee and heads to a different OR for her major case of the day: a craniotomy to resect a glioblastoma, an aggressive brain tumor. This surgery is highly complex and will likely take 5-6 hours.
- 3:30 PM: The tumor resection is successful. Dr. Vance oversees the patient's transfer to the neuro-ICU and provides a detailed update to the anxious family. She hasn't eaten lunch.
- 4:00 PM: She heads to her afternoon clinic, where she will see a mix of new patient referrals and post-operative follow-ups. She sees a patient with a newly diagnosed pituitary adenoma, another with chronic back pain she will manage non-surgically, and a patient she operated on two months ago who is now symptom-free.
- 6:30 PM: Clinic is finished. She spends the next hour and a half at her desk completing patient charts, responding to emails, and reviewing the scans for tomorrow's surgical cases.
- 8:00 PM: Dr. Vance heads home. Tonight, she is not on call, but her phone is never truly off. An emergency can page her back to the hospital at any moment. This demanding schedule, combining intense clinical focus, physical stamina, and deep intellectual engagement, is the foundation upon which a neurosurgeon's salary is built.
Average Neurosurgeon Salary: A Deep Dive
Neurosurgery consistently ranks as one of the most, if not *the* most, lucrative medical specialties. The extensive training, the high-stakes nature of the work, the demanding lifestyle, and the complex procedures all contribute to a compensation package that is unmatched in most other fields. When examining the data, it's essential to look at multiple authoritative sources to get a complete picture, as methodology and the populations surveyed can vary.
According to the 2023 Medscape Physician Compensation Report, one of the most respected annual surveys in the industry, neurosurgery is the highest-paid specialty. The report found the average annual salary for a neurosurgeon to be $788,313. This figure represents total compensation, including salary, bonuses, and profit-sharing contributions.
Other reputable sources provide similar, albeit slightly different, figures, reinforcing this top-tier status:
- Doximity's 2023 Physician Compensation Report, which analyzes data from over 190,000 U.S. physicians, placed neurosurgery at the top of its list with an average annual compensation of $773,201.
- Salary.com, which aggregates real-time data from employers, reports a median neurosurgeon salary in the United States of $698,501 as of late 2023, with the typical range falling between $526,101 and $883,801.
- It's important to note that the U.S. Bureau of Labor Statistics (BLS) groups neurosurgeons with all other surgeons in their Occupational Outlook Handbook, reporting a median pay of $239,200 per year in 2022. While the BLS is an excellent resource for many professions, this broad category significantly underrepresents the specific earning potential of a highly specialized field like neurosurgery. Therefore, physician-specific sources like Medscape and Doximity are more accurate for this analysis.
### Salary by Experience Level
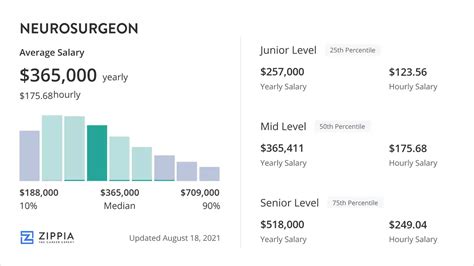
A neurosurgeon's salary follows a steep trajectory, beginning with a modest training salary and growing exponentially upon completion of residency.
| Career Stage | Typical Years of Experience | Typical Annual Compensation Range | Notes |
| :--- | :--- | :--- | :--- |
| Neurosurgical Resident | Years 1-7 (Post-M.D.) | $65,000 - $85,000 | This is a training salary, not reflective of professional earning potential. Varies by institution and location. |
| Fellow | Years 8-9 (Post-M.D.) | $80,000 - $100,000 | A slightly higher training salary for those pursuing a subspecialty after residency. |
| Early Career Neurosurgeon| 1-5 Years Post-Residency| $350,000 - $600,000 | Initial salaries can be lower as surgeons build their practice, reputation, and efficiency. Signing bonuses are common. |
| Mid-Career Neurosurgeon | 6-15 Years | $600,000 - $950,000 | Peak earning years. Surgeons have established referral networks, high efficiency, and may be partners in a private practice. |
| Senior Neurosurgeon | 15+ Years | $750,000 - $1,200,000+ | Earnings can remain high or even increase, especially for those in private practice or with world-renowned expertise. Some may scale back clinical work, slightly reducing income. |
*Disclaimer: These ranges are estimates compiled from industry reports and are subject to significant variation based on the factors discussed in the next section.*
### Deconstructing the Compensation Package
The headline salary figure is only part of the story. A neurosurgeon's total compensation is a blend of several components:
- Base Salary: A guaranteed annual salary, more common in academic positions or some hospital-employed models. In many cases, the base salary is modest, with the bulk of earnings coming from productivity bonuses.
- Productivity Bonuses (RVU-Based): This is the most significant driver of income for most neurosurgeons. Compensation is tied to Work Relative Value Units (wRVUs), a measure of physician work assigned to each medical service or procedure by Medicare. Complex surgeries like a craniotomy are assigned a high RVU value. Surgeons are paid a certain dollar amount per RVU generated, incentivizing high volume and complex cases.
- Signing Bonus: To attract top talent out of residency or fellowship, hospitals and private groups often offer substantial signing bonuses, which can range from $25,000 to over $100,000.
- Call Pay: Neurosurgeons are often paid an additional daily stipend for being on call for a hospital's emergency department, especially for trauma coverage.
- Profit Sharing / Partnership Income: For those in private practice, a significant portion of their income comes from the practice's profits after overhead costs are paid. This offers the highest earning potential but also carries the financial risks of running a business.
- Benefits and Perks: The value of the benefits package is substantial. It almost always includes:
- Malpractice Insurance: This is a critical and extremely expensive benefit, often costing over $100,000 per year, which is typically covered by the employer or practice.
- Health, Dental, and Vision Insurance.
- Generous Retirement Plans: Such as 401(k) or 403(b) with significant employer matching contributions.
- Continuing Medical Education (CME) Allowance: Funds to attend conferences and stay current with the latest techniques.
- Relocation Assistance.
Understanding these components is crucial for any aspiring neurosurgeon evaluating a job offer. A lower base salary with a high RVU potential in a busy practice can ultimately be far more lucrative than a high guaranteed salary in a lower-volume setting.
Key Factors That Influence Salary

While the national averages provide a strong benchmark, the actual salary for neurosurgeon professionals can vary dramatically based on a confluence of factors. A neurosurgeon in a rural state performing high-volume spine surgery in a private practice will have a vastly different income statement than a pediatric neurosurgeon in an academic center in a major metropolitan area. This section breaks down the most critical variables that dictate earning potential.
### ### 1. Area of Specialization
After a grueling seven-year residency, many neurosurgeons pursue an additional one-to-two-year fellowship to become subspecialists. This choice has arguably the most significant impact on their career trajectory and long-term earnings. Reimbursement rates, case volume, and market demand differ substantially between subspecialties.
- Spine Surgery: This is consistently the most lucrative subspecialty within neurosurgery. The high prevalence of degenerative spine disease in an aging population creates immense demand. Procedures like spinal fusions, laminectomies, and discectomies are common and have high RVU values. A spine-focused neurosurgeon in a busy practice can often be among the highest earners in all of medicine, with compensation frequently exceeding $1 million annually.
- Cranial and Skull Base Surgery: This involves the treatment of brain tumors, aneurysms, and other complex vascular issues. These are among the most difficult and highest-risk procedures in medicine. While the case volume may be lower than in spine surgery, the complexity and high reimbursement per case result in very high compensation.
- Endovascular Neurosurgery: A highly technical and growing field where surgeons treat vascular conditions like aneurysms and arteriovenous malformations (AVMs) using minimally invasive, catheter-based techniques from within the blood vessels. This specialization is in high demand, and its practitioners command top-tier salaries due to their unique skillset.
- Pediatric Neurosurgery: This field requires an additional fellowship and a unique skillset to operate on the developing nervous systems of infants and children. While incredibly rewarding, it can sometimes be less lucrative than adult spine or cranial surgery. Case volumes are lower, and the payer mix may include a higher percentage of Medicaid, which reimburses at lower rates. However, compensation remains exceptionally high compared to nearly any other profession.
- Functional Neurosurgery: This subspecialty focuses on surgically treating movement disorders (like Parkinson's disease via deep brain stimulation), epilepsy, and chronic pain. It is a rapidly advancing field with growing demand, offering strong earning potential.
- Peripheral Nerve Surgery: This involves treating conditions like carpal tunnel syndrome, ulnar nerve entrapment, and nerve injuries. While an important field, it generally involves less complex procedures with lower reimbursement rates compared to cranial or spine surgery, leading to comparatively lower (though still very high) overall compensation.
### ### 2. Geographic Location
Where a neurosurgeon practices has a profound impact on their salary, driven by supply and demand, cost of living, and local insurance markets. The Doximity 2023 compensation report highlights significant regional variations.
Highest-Paying States/Regions:
Often, less populated states or those in the Midwest and Southeast offer higher salaries to attract and retain scarce surgical talent. States that have enacted tort reform, which limits malpractice liability, can also be more financially attractive. According to various industry reports, states like Wisconsin, Nebraska, North Carolina, and Indiana often appear in the top ten for physician compensation.
- Example: A private practice group in a mid-sized city in the Midwest might offer a starting salary of $750,000 plus productivity bonuses to a new spine surgeon, as they are competing with only a few other groups in a large catchment area.
Lower-Paying (but still high) States/Regions:
Conversely, major metropolitan areas on the coasts, such as New York City, Los Angeles, and Boston, may have slightly lower average salaries. This is counterintuitive given the high cost of living, but it's a result of market saturation. These cities have numerous prestigious academic medical centers and a high density of surgeons, leading to greater competition for patients and more leverage for insurance companies.
- Example: An academic neurosurgeon at a world-renowned hospital in Boston might earn $550,000. While this is an elite salary, it may be less than what they could earn in a less competitive market, but the prestige, research opportunities, and quality of life may be considered a fair trade-off.
Urban vs. Rural Divide:
The most significant geographical salary driver is the urban vs. rural gap. Rural hospitals and communities face chronic shortages of specialists and must offer premium compensation packages, often including student loan forgiveness and housing allowances, to recruit neurosurgeons. A surgeon willing to practice in a less-desirable, underserved area can command a salary significantly above the national average.
### ### 3. Practice Setting (Type of Employer)
The type of organization a neurosurgeon works for is a primary determinant of their compensation structure and overall earning potential.
- Private Practice (Physician-Owned Group): This model offers the highest earning potential. After an initial period as an employee (typically 2-3 years), a surgeon may be offered partnership. As a partner, they share in the practice's profits. These groups are run as businesses, focused on efficiency and productivity. Top-earning neurosurgeons making well over $1 million per year are almost always partners in a successful private practice. However, this model also carries the most risk and administrative burden, as partners are responsible for overhead, staffing, billing, and marketing.
- Hospital-Employed: This is now the most common employment model. The hospital or health system employs the surgeon directly, handling all administrative and business aspects. This provides stability, predictable hours (to an extent), and excellent benefits, including covered malpractice insurance. Compensation is typically a base salary plus a productivity (wRVU) bonus. While the ceiling for earnings is generally lower than in private practice, it removes the risks of business ownership and is an attractive option for many.
- Academic Medical Center: Neurosurgeons at university-affiliated hospitals balance their time between clinical work, teaching medical students and residents, and conducting research. This "three-legged stool" of responsibilities means less time is dedicated to clinical productivity compared to private practice. As a result, salaries in academia are typically the lowest of the three models. However, the compensation package often includes strong benefits, institutional prestige, and the non-monetary rewards of shaping the future of medicine. A typical academic neurosurgeon might earn in the $400,000 to $700,000 range.
- Locum Tenens: This involves working as a temporary, independent contractor to fill in for other surgeons who are on vacation, on leave, or to cover staffing shortages. *Locum tenens* work can be extremely lucrative, often paying a high daily rate (e.g., $2,000 - $4,000+ per day) plus travel and housing expenses. It offers flexibility but lacks the stability and benefits of a permanent position.
### ### 4. Years of Experience and Reputation
As detailed in the salary table, experience plays a direct role. This is not simply a matter of annual raises.
- Efficiency: An experienced surgeon is faster and more efficient in the OR. They can perform more cases in the same amount of time, directly increasing their wRVU generation and, therefore, their income.
- Referral Network: Over time, a neurosurgeon builds a strong reputation among local primary care physicians, neurologists, and emergency rooms. This leads to a steady stream of patient referrals, which is the lifeblood of any surgical practice.
- Complexity of Cases: Senior surgeons are often referred the most complex and challenging cases, which carry the highest reimbursement rates. Their experience allows them to take on cases that a younger surgeon might not be comfortable with.
### ### 5. In-Demand Skills and Technological Proficiency
Medicine is constantly evolving, and a surgeon's willingness and ability to adopt new technologies can enhance their value and earning potential.
- Minimally Invasive Surgery (MIS): Proficiency in minimally invasive techniques, particularly for spine surgery (MIS-TLIF, XLIF), is highly sought after. These procedures often lead to faster recovery times for patients and are increasingly in demand.
- Robotic-Assisted Surgery: While still emerging in neurosurgery, the use of robotic platforms for spine surgery and certain cranial procedures is a growing area. Surgeons with this expertise can be a major draw for hospitals looking to market themselves as technologically advanced.
- Endoscopic and Endovascular Techniques: Expertise in using endoscopes for skull base surgery or endovascular methods for aneurysms is a distinct, high-value skill set that separates a surgeon from their peers and drives higher compensation.
- Stereotactic Radiosurgery: Certification and skill in using focused radiation technologies like Gamma Knife or CyberKnife to treat tumors and other abnormalities non-invasively is another valuable adjunct to a neurosurgeon's practice.
Job Outlook and Career Growth

For anyone considering the decade-plus investment to become a neurosurgeon, the long-term viability of the profession is a critical concern. The good news is that the demand for neurosurgical services is strong and projected to grow, driven by powerful demographic and technological trends.
The U.S. Bureau of Labor Statistics (BLS) projects that employment for all physicians and surgeons will grow by 3% from 2022 to 2032. While this may seem modest, it represents approximately 24,300 new openings each year, on average, over the decade, primarily to replace physicians who retire or leave the profession. However, the outlook for neurosurgery, specifically, is even more robust than this general figure suggests due to several key factors.
Key Drivers of Demand:
1. An Aging Population: The "silver tsunami" of the baby boomer generation is the single most significant factor driving demand. As people age, they are more susceptible to the neurological conditions that neurosurgeons treat, including:
- Degenerative Spine Disease: Conditions like spinal stenosis, herniated discs, and spondylolisthesis become increasingly common with age, fueling the high demand for spine surgeons.
- Stroke: The risk of both ischemic and hemorrhagic stroke increases significantly with age. Neurosurgeons, particularly endovascular specialists, play a crucial role in the acute treatment of stroke.
- Brain Tumors: The incidence of certain brain tumors increases in older populations.
- Normal Pressure Hydrocephalus (NPH): A treatable form of dementia in the elderly that requires a neurosurgeon to place a shunt.
2. Technological Advancements: The continuous innovation in neurosurgical techniques and technologies is expanding the range of treatable conditions.
- Minimally Invasive Options: The development of MIS techniques makes surgery an option for older or sicker patients who may not have
