Table of Contents

- [Introduction](#introduction)
- [What Does a Surgical Resident Do? The Grueling Reality of Training](#what-does-a-surgical-resident-do)
- [Average Surgical Resident Salary: A Deep Dive into Compensation](#average-salary-a-deep-dive)
- [Key Factors That Influence a Surgical Resident's Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth for Surgeons](#job-outlook-and-career-growth)
- [How to Become a Surgical Resident: Your Step-by-Step Roadmap](#how-to-get-started)
- [Conclusion: The True Value of a Surgical Residency](#conclusion)
---
Introduction

The sterile scent of the operating room, the focused hum of life-sustaining machinery, the intense, almost tangible silence before the first incision—this is the world you aspire to command. The path to becoming a surgeon is one of the most demanding, rigorous, and respected journeys in all of medicine. It’s a calling defined by immense responsibility, intellectual challenge, and the profound ability to change lives. But as you stand at the precipice of this life-altering commitment, a practical and crucial question surfaces: What is the salary for a surgical resident?
Let's be direct: during residency, you will not be compensated in a way that reflects your hours worked, your level of education, or the life-and-death decisions you make daily. The average surgical resident in the United States earns between $60,000 and $85,000 per year. This figure, while a livable wage, is a modest stipend for a doctor who has already invested nearly a decade and hundreds of thousands of dollars into their education. It is, in essence, an investment—a trade of short-term financial gain for unparalleled training and a future of significant earning potential.
I once spent an evening speaking with a third-year general surgery resident after she had finished a grueling 28-hour call. Exhausted but lucid, she told me, "My paycheck covers my rent and my student loan payments, but the real salary isn't deposited in my bank account. It's the moment my attending trusts me to perform a critical part of a procedure alone. That's the compensation that matters right now." Her perspective encapsulates the core truth of residency: the salary is the education, and the paycheck simply allows you to survive the process.
This guide is designed to be your definitive resource, providing a comprehensive, data-driven, and transparent look at the financial realities of surgical residency. We will dissect national salary data, explore the myriad factors that influence your pay, analyze the long-term career outlook, and provide a clear roadmap for how to embark on this challenging but incredibly rewarding path. We will move beyond simple numbers to give you the context and insight necessary to make informed decisions about your future.
---
What Does a Surgical Resident Do? The Grueling Reality of Training

A surgical resident is a physician who has graduated from medical school (with an M.D. or D.O. degree) and is now undergoing supervised, hands-on training in a specific surgical specialty at a hospital or academic medical center. This period, known as residency, can last anywhere from five years for general surgery to seven years or more for specialties like neurosurgery or plastic surgery. The role is a unique and demanding hybrid: you are simultaneously a student, a teacher, a clinician, and a frontline medical provider.
The core of a surgical resident's job is to progressively master the art and science of surgery under the direct supervision of experienced attending surgeons. This involves a meticulously structured escalation of responsibility, beginning with basic procedures and culminating in the ability to perform complex operations independently.
Core Responsibilities and Daily Tasks:
- Patient Care (Pre- and Post-Operative): Residents are responsible for the complete care of surgical patients. This includes conducting initial consultations in the emergency department or clinic, ordering and interpreting diagnostic tests, obtaining informed consent, and managing patients' medical conditions before surgery. Post-operatively, they manage pain, monitor for complications, change dressings, and coordinate discharge planning.
- Operating Room Assistance and Performance: Junior residents (interns, or PGY-1s, for Post-Graduate Year 1) typically start by holding retractors, suturing incisions, and learning the flow of the operating room. As they gain experience and trust, they progress to performing parts of operations and, eventually, leading entire cases with an attending surgeon supervising.
- Rounding: A significant portion of the day is spent on "rounds," where the surgical team (attending, residents, medical students) visits each patient on their service. Residents present the patient's case, provide overnight updates, and formulate a treatment plan for the day.
- On-Call Duties: Surgical residents work long hours, frequently including overnight and weekend "call" shifts. During a call shift, a resident is the first point of contact for all issues related to their service's patients in the hospital, as well as for new consults from the emergency room. This can involve triaging patients, performing emergency bedside procedures, or taking a patient for an urgent operation in the middle of the night.
- Administrative and Didactic Work: Beyond clinical duties, residents must meticulously document patient encounters in electronic health records, present cases at morbidity and mortality (M&M) conferences, attend lectures, and study relentlessly for in-training exams and board certification tests. Many are also required to conduct clinical research and publish their findings.
### A Day in the Life of a Junior Surgical Resident (PGY-2)
To make this tangible, here is a realistic, albeit compressed, look at a typical day for a second-year general surgery resident on a busy trauma service:
- 4:30 AM: Wake up. Quickly get ready, grab a protein bar, and head to the hospital.
- 5:00 AM - 6:30 AM: "Pre-rounding." You arrive at the hospital and, with your intern, see all 15 patients on your team's list. You check their vitals, review overnight nurse notes, check drains and wounds, and read any new lab or imaging results. You formulate a preliminary plan for each patient.
- 6:30 AM - 7:30 AM: Team Rounds. The entire team, including the chief resident and attending surgeon, convenes. You present each patient succinctly, field questions, and finalize the day's plan. New orders are placed.
- 7:45 AM - 1:00 PM: Operating Room. Today's case is a complex colectomy. As the PGY-2, you are the "first assist." You help position the patient, make the initial incision under supervision, and perform key parts of the dissection. The attending guides you, quizzing you on anatomy and technique throughout the procedure.
- 1:00 PM - 2:00 PM: A quick lunch in the physician's lounge while answering pages about post-op patients and placing orders.
- 2:00 PM - 5:00 PM: "Floor work." You follow up on the plans made during morning rounds. This involves calling consulting services, talking to families, performing bedside procedures like placing a central line, and writing progress notes. You also see a new consult in the ER for acute appendicitis and book them for surgery later that evening.
- 5:00 PM - 6:30 PM: Evening Rounds & Sign-Out. You and the intern round again on the sickest patients to ensure they are stable. You then prepare a detailed "sign-out" list for the on-call resident, carefully transferring responsibility for every patient.
- 6:30 PM: You leave the hospital. The day isn't over.
- 7:30 PM - 10:00 PM: Dinner, followed by reading. You have to prepare for tomorrow's scheduled cases, which means reviewing the relevant anatomy and surgical steps. You also study a chapter for your upcoming in-training exam.
- 10:00 PM: Sleep. The alarm is set for 4:30 AM.
This grueling schedule, often exceeding the 80-hour work week limit set by the ACGME (Accreditation Council for Graduate Medical Education), is the crucible in which a surgeon is forged. The salary is the means to endure it; the education is the reason to pursue it.
---
Average Surgical Resident Salary: A Deep Dive into Compensation

When analyzing the salary for a surgical resident, it's crucial to understand that the pay structure is fundamentally different from almost any other profession. It is not a free-market wage determined by individual negotiation or performance. Instead, resident salaries are standardized stipends set by the hospital or institution, primarily influenced by the resident's post-graduate year (PGY) level and the geographic location of the training program.
The most authoritative source for this data is the Association of American Medical Colleges (AAMC). According to the AAMC's 2023 Survey of Resident/Fellow Stipends and Benefits, the national average stipend for a first-year resident (PGY-1) was $64,200. This figure serves as the baseline, with compensation increasing incrementally each year of training.
A comprehensive view of the salary landscape looks like this:
- National Average PGY-1 Stipend: ~$64,200 per year
- Typical National Salary Range (All PGY Levels): $60,000 to $85,000 per year
- Top-Tier Programs in High-Cost-of-Living Areas: May reach up to $90,000+ for senior residents.
It is important to distinguish this from data provided by the U.S. Bureau of Labor Statistics (BLS). The BLS reports on "Physicians and Surgeons," with a median pay of $239,200 per year in 2023. This figure represents *attending* physicians who have completed residency, not residents in training. The ~7-fold difference highlights the financial sacrifice residency entails and the significant income jump that occurs upon its completion.
### Salary Progression by Experience (PGY Level)
The most direct determinant of a resident's salary is their PGY level. Each year, as a resident gains experience and assumes more responsibility, their stipend increases. This annual raise is typically between $2,000 and $3,500.
Here is a representative table of salary progression, based on aggregated data from AAMC and Medscape's 2023 Resident Salary & Debt Report. Actual figures will vary by institution, but the structure is consistent.
| Post-Graduate Year (PGY) | Typical Role / Responsibility Level | Average Annual Salary Range |
| ------------------------ | ------------------------------------------------ | --------------------------- |
| PGY-1 (Intern) | Foundational skills, basic procedures, floor work | $62,000 - $67,000 |
| PGY-2 | Increased OR responsibility, managing interns | $64,000 - $70,000 |
| PGY-3 | Mid-level resident, more complex cases | $66,000 - $73,000 |
| PGY-4 | Senior resident, leading junior team members | $69,000 - $76,000 |
| PGY-5 (Chief) | Administrative duties, leading complex cases | $72,000 - $80,000 |
| PGY-6 / PGY-7 | For longer specialties (e.g., Neurosurgery) | $75,000 - $85,000+ |
*(Source: Data compiled and synthesized from AAMC 2023 Survey of Resident/Fellow Stipends and Benefits and Medscape Resident Salary & Debt Report 2023.)*
As a chief resident (the final year of most general surgery programs), you are not just an advanced trainee but also a junior manager, responsible for scheduling, teaching, and running a clinical service. The salary increase reflects this added administrative and leadership burden.
### Beyond the Stipend: A Look at Total Compensation
While the base stipend is the headline number, the total compensation package offers significant value that is often overlooked. Hospitals are competing to attract the best medical school graduates, and they do so by offering robust benefits packages.
Common Components of a Resident's Compensation Package:
- Health Insurance: Comprehensive medical, dental, and vision insurance is almost always provided at little to no cost to the resident. Family plans are also typically available.
- Malpractice Insurance: The hospital provides complete professional liability coverage. This is a massive benefit, as private malpractice insurance for a surgeon can cost tens of thousands of dollars per year.
- Disability and Life Insurance: Most programs provide group long-term disability and life insurance policies, protecting you and your family in case of tragedy.
- Retirement Savings Plans: Residents are usually eligible to contribute to a 401(k) or 403(b) retirement plan. Many institutions offer a matching contribution (e.g., matching 50% of your contribution up to 6% of your salary). This is "free money" and a critical tool for building wealth, even on a resident's salary.
- Educational Stipend/Fund: Programs typically provide an annual allowance (e.g., $1,000 - $2,500) that can be used for textbooks, medical equipment (like surgical loupes), board review courses, or travel to academic conferences.
- Meal Stipend/Call-Room Food: Most hospitals provide a meal allowance or have designated cafeterias and doctor's lounges with free food and drink for on-call residents.
- Paid Time Off (PTO): Residents typically receive 3-4 weeks of paid vacation per year. However, the culture of surgery can make it challenging to take all of it.
- Licensing and Exam Fees: Many programs will reimburse the costs of state medical licenses and board examinations, which can amount to several thousand dollars.
When you factor in these benefits, the true value of the compensation package is significantly higher than the base stipend alone. The lack of bonuses or profit-sharing is standard; the reward is the training that unlocks a high six-figure or even seven-figure income in the future.
---
Key Factors That Influence a Surgical Resident's Salary
While PGY level is the primary driver of a resident's base salary within a single institution, several other crucial factors create significant variations in pay across the country. Understanding these variables is key to evaluating different residency program offers and managing your personal finances during these demanding years. This is the most detailed part of our analysis, as it holds the keys to understanding the *why* behind the numbers.
###
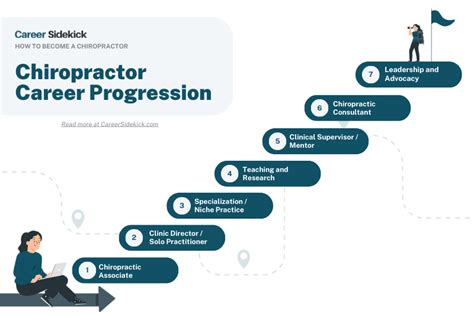
Years of Experience (Post-Graduate Year)
As established, this is the most significant and consistent factor. A residency program's salary schedule is almost always a lock-step progression based on PGY year. The rationale is straightforward: a PGY-5 chief resident brings far more value, skill, and efficiency to the hospital than a PGY-1 intern. They can manage a service, perform complex procedures with minimal supervision, and teach junior residents and students, effectively acting as a force multiplier for the attending surgeon.
- PGY-1 to PGY-2: This jump often reflects the transition from being heavily supervised to gaining the first real taste of autonomy.
- PGY-3 to PGY-4: At this mid-level stage, residents are the workhorses of the program, trusted with significant operative and clinical responsibility. The salary increase acknowledges this growing competence.
- Chief Resident (PGY-5+): The chief resident's salary reflects their dual role as a senior clinician and a junior administrator. They are often responsible for creating the call schedule, running educational conferences, and handling initial disciplinary issues, justifying the highest stipend in the program.
The incremental raises, while modest, are a formal acknowledgment of your increasing expertise and value to the hospital ecosystem.
###
Geographic Location: The Cost-of-Living Conundrum
Geography is arguably the second-most important factor influencing nominal salary. Residency programs in high-cost-of-living metropolitan areas must offer higher stipends to ensure their residents can afford basic housing and necessities. However, a higher salary does not always equate to greater purchasing power.
According to Medscape's 2023 report, residents in the Northeast region of the U.S. reported the highest average salary (around $70,000), while those in the South Central region reported the lowest (around $62,500).
Let's look at a comparative example using data aggregated from FREIDA (the AMA's residency program database) and institutional GME (Graduate Medical Education) websites:
| City/Region | Representative Institution | Average PGY-1 Salary (Approx.) | 2-BR Apartment Rent (Avg.) | Real Wage Comparison |
| -------------------- | ------------------------------------ | ------------------------------ | -------------------------- | -------------------- |
| New York, NY | Major NYC Academic Center | ~$78,000 | $4,500+ / month | Lower Purchasing Power |
| Cleveland, OH | Major Ohio Academic Center | ~$65,000 | $1,400 / month | Higher Purchasing Power |
| San Francisco, CA | Bay Area University Program | ~$84,000 | $3,500+ / month | Lower Purchasing Power |
| Houston, TX | Texas Medical Center Institution | ~$64,000 | $1,600 / month | Higher Purchasing Power |
*(Sources: Institutional GME websites, Zumper/Rent.com rental data for 2023-2024)*
Analysis:
A resident in San Francisco might earn $20,000 more per year than a resident in Houston. However, the difference in annual rent for a modest apartment could easily exceed $22,000. In this scenario, the Houston resident has significantly more disposable income, despite the lower nominal salary. Aspiring residents must look beyond the gross salary figure and run a cost-of-living calculation to understand the true financial implications of a program's location.
Highest Paying States/Regions (Nominal Salary):
- Northeast (New York, Massachusetts, Connecticut)
- West Coast (California)
States/Regions with Higher Purchasing Power (Lower Salary, Lower Cost of Living):
- Midwest (Ohio, Michigan, Indiana)
- South/Southeast (Texas, Alabama, Georgia)
###
Institution Type & Size: Academic Giant vs. Community Hospital
The type of hospital hosting the residency program can also impact compensation, though often in subtle ways.
- Major University/Academic Medical Centers: These are large, research-intensive institutions often located in major cities (e.g., Johns Hopkins, Massachusetts General Hospital, UCSF). They tend to offer higher nominal salaries to compete for top talent and offset the high cost of living in their urban locations. They also provide unparalleled research opportunities and networking, which can be invaluable for future fellowship applications and academic careers.
- Community Hospital Programs: These are often smaller, more clinically-focused programs, sometimes located in suburban or rural areas. Their stipends may be slightly lower than their large academic counterparts. However, they can offer a different kind of value: a higher volume of "bread-and-butter" surgical cases, more one-on-one time with attending surgeons, and potentially a better work-life balance. The cost of living in these areas is also frequently lower, potentially making the financial package more attractive in real terms.
- Government/VA Hospitals: Programs at Veterans Affairs (VA) hospitals or other government institutions have salaries set by federal pay scales. These are often competitive and come with robust federal benefits, but may have less flexibility than private institutions.
The "size" of the program (number of resident spots) is less of a direct factor on salary but can influence the experience. Larger programs may feel more institutional, while smaller programs can foster a more tight-knit, familial atmosphere.
###
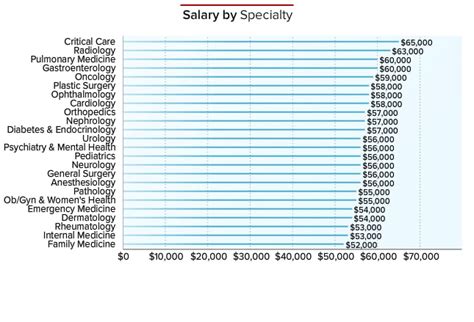
Area of Specialization: The Long Game
This is a critical point of clarification. During residency itself, the surgical subspecialty has very little direct impact on your salary. A PGY-3 neurosurgery resident and a PGY-3 general surgery resident at the same hospital will earn an almost identical stipend. The salary is tied to the institution and PGY level, not the specialty.
However, the choice of specialty dramatically impacts two things:
1. Length of Training: This affects your total earnings *during* the residency period.
2. Future Earning Potential: This is where the astronomical differences lie.
Let's compare:
| Surgical Specialty | Typical Residency Length | PGY-1 Salary (Same Institution) | Median Attending Salary (Post-Residency) |
| ----------------------- | ------------------------ | ------------------------------- | --------------------------------------------- |
| General Surgery | 5 Years | ~$65,000 | ~$402,000 |
| Orthopedic Surgery | 5 Years | ~$65,000 | ~$573,000 |
| Plastic Surgery | 6 Years (Integrated) | ~$65,000 | ~$571,000 |
| Neurosurgery | 7 Years | ~$65,000 | ~$788,000 |
*(Source: Medscape Physician Compensation Report 2023 for attending salaries)*
Analysis:
A neurosurgery resident will spend two additional years earning a resident's salary compared to a general surgeon. This means two more years of delayed gratification and accumulating student loan interest. However, their future earning potential is nearly double. When choosing a specialty, you are making a long-term financial calculation. The short-term salary is standardized, but the long-term financial trajectory is defined by this choice.
###
In-Demand Skills & Other Factors (Impacting Future, Not Current, Salary)
It's important to note that, unlike in a corporate environment, specific "skills" do not get you a raise during residency. You cannot negotiate a higher PGY-2 salary because you are a gifted researcher or have excellent laparoscopic skills. The pay structure is rigid.
However, developing certain skills during residency is the single most important thing you can do to maximize your *future* salary as an attending surgeon. These skills make you a top candidate for competitive fellowships and desirable private practice or academic positions.
Skills That Drive Future Value:
- Procedural Excellence & High Case Volume: Meticulously logging a high volume and wide variety of surgical cases proves your competence and readiness for independent practice.
- Research and Publications: A strong research portfolio with publications in peer-reviewed journals is essential for securing competitive fellowships and positions at academic medical centers.
- Leadership and Teaching: Excelling as a chief resident, winning teaching awards, and mentoring junior residents demonstrates leadership potential that is highly valued.
- Networking: Building strong relationships with attending surgeons and faculty who will write powerful letters of recommendation is invaluable.
- Fellowship Training: Completing a fellowship (e.g., in cardiothoracic, trauma, or surgical oncology after general surgery) is the most direct way to increase your specialization and, therefore, your earning potential as an attending.
Essentially, you are not paid for these skills during residency; you are paid *with* them. They are the currency that you will cash in upon graduation.
---
Job Outlook and Career Growth for Surgeons
While the residency years are financially lean, the long-term outlook for surgeons is exceptionally strong. The investment of time, effort, and forgone income during training pays off with a career that is not only professionally rewarding but also financially lucrative and stable.
### Job Growth Projections
The U.S. Bureau of Labor Statistics (BLS), in its Occupational Outlook Handbook, projects that employment for physicians and surgeons will grow by 3 percent from 2022 to 2032. While this is about as fast as the average for all occupations, the number belies the true demand.
The BLS projects about 24,300 openings for physicians and surgeons each year, on average, over the decade. Many of these openings are expected to result from the need to replace workers who transfer to different occupations or exit the labor force, such as to retire.
The key driver of this sustained demand is a combination of factors:
1. An Aging Population: As the large baby-boomer generation ages, there will be an increased need for surgical interventions, from joint replacements and cardiac procedures to cancer-related surgeries.
2. Physician Retirements: A significant portion of the current surgical workforce is approaching