Introduction

Imagine being the professional a worried family turns to when their child faces a mysterious and frightening neurological condition. You are the detective, the scientist, and the compassionate guide who navigates the intricate landscape of the developing brain to provide answers, treatments, and hope. This is the profound reality of a pediatric neurologist. It's a career that demands immense dedication, intellectual rigor, and emotional resilience, but it offers a reward that few professions can match: the chance to fundamentally alter the course of a child's life for the better.
Beyond this deep intrinsic value lies a career that is also financially rewarding and remarkably stable. The salary of a pediatric neurologist reflects the years of specialized training and the critical demand for their expertise, with most professionals earning well into the six-figure range, often starting above $200,000 and climbing significantly with experience. I once had the privilege of speaking with a senior pediatric neurologist who recounted diagnosing a rare, treatable metabolic disorder in an infant who had been seen by multiple specialists without success. She said, "That moment—when you tell a family not only what's wrong, but that you have a plan to help—is the reason you endure a decade of training." That single sentiment captures the powerful synthesis of purpose and profession that defines this field.
This comprehensive guide is designed to be your definitive resource, whether you are a medical student weighing specialties, a resident exploring fellowships, or simply curious about this vital field. We will dissect every facet of a pediatric neurologist's compensation, explore the factors that drive salary variations, analyze the job outlook, and provide a clear, step-by-step roadmap to entering this exceptional career.
### Table of Contents
- [What Does a Pediatric Neurologist Do?](#what-does-a-pediatric-neurologist-do)
- [Average Pediatric Neurologist Salary: A Deep Dive](#average-pediatric-neurologist-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Become a Pediatric Neurologist](#how-to-become-a-pediatric-neurologist)
- [Conclusion: Is a Career in Pediatric Neurology Right for You?](#conclusion-is-a-career-in-pediatric-neurology-right-for-you)
---
What Does a Pediatric Neurologist Do?

A pediatric neurologist, or child neurologist, is a highly specialized physician dedicated to the diagnosis, treatment, and management of disorders affecting the nervous system in children, from newborns to young adults. Their domain is the most complex organ in the body—the brain—as well as the spinal cord, nerves, and muscles. Unlike adult neurology, this field is uniquely focused on conditions that arise during the dynamic process of development, including congenital defects, genetic and metabolic disorders, and injuries that can have lifelong implications.
The core of their work is a blend of meticulous diagnostic investigation and long-term patient care. They are medical detectives, piecing together clues from a patient's history, physical examinations, and advanced imaging and electrical studies to arrive at a diagnosis.
Core Responsibilities and Daily Tasks:
- Patient Consultation: Meeting with children and their families to discuss symptoms, take detailed medical histories, and perform comprehensive neurological exams to assess motor skills, sensory function, reflexes, balance, and cognitive abilities.
- Diagnostic Testing: Ordering and interpreting a wide range of sophisticated tests, including:
- Electroencephalography (EEG): To record brain electrical activity, crucial for diagnosing seizures and epilepsy.
- Magnetic Resonance Imaging (MRI) & Computed Tomography (CT) Scans: To visualize the brain and spinal cord, identifying tumors, malformations, or signs of injury.
- Lumbar Punctures (Spinal Taps): To analyze cerebrospinal fluid for signs of infection, inflammation, or metabolic issues.
- Electromyography (EMG) and Nerve Conduction Studies (NCS): To assess the health of muscles and the nerves that control them.
- Treatment Planning: Developing and overseeing comprehensive treatment plans that may include medication (e.g., anti-epileptic drugs), dietary therapies (e.g., ketogenic diet), referrals to physical, occupational, or speech therapists, and coordination with other medical specialists.
- Managing Chronic Conditions: A significant portion of the role involves long-term management of chronic illnesses like epilepsy, cerebral palsy, muscular dystrophy, and developmental disorders such as autism spectrum disorder, often building relationships with families that last for years.
- Collaboration: Working as part of a multidisciplinary team alongside pediatricians, neurosurgeons, geneticists, psychiatrists, and rehabilitation specialists to provide holistic care.
- Research and Academics: Many pediatric neurologists, particularly in academic centers, are actively involved in clinical research to advance the understanding and treatment of neurological diseases, as well as teaching medical students and residents.
### A Day in the Life of a Hospital-Based Pediatric Neurologist
To make this role more tangible, consider a typical day:
- 7:30 AM - 9:00 AM: Inpatient Rounds. The day begins at the hospital, seeing patients admitted overnight or those being monitored. This might include a child in the pediatric ICU with a traumatic brain injury, a newborn in the NICU having seizures, or a patient admitted for an extended EEG monitoring session. The neurologist reviews charts, examines patients, and collaborates with the hospitalist team to adjust treatment plans.
- 9:30 AM - 12:30 PM: Morning Outpatient Clinic. The scene shifts to the outpatient clinic. The schedule is packed with a mix of new consultations and follow-up visits.
- *9:30 AM:* A new 6-year-old patient with frequent, debilitating headaches. The task is to differentiate between common migraines and something more serious.
- *10:15 AM:* A follow-up with a 10-year-old with well-controlled epilepsy to discuss medication adjustments and school performance.
- *11:00 AM:* A complex consultation for a toddler with developmental delays and muscle weakness, requiring a thorough exam and plans for genetic testing.
- 12:30 PM - 1:30 PM: Administrative and Review Time. This hour is a frantic catch-up period. It's spent reviewing the morning's MRI and EEG results, dictating patient notes into the electronic health record, returning urgent phone calls from parents, and grabbing a quick lunch.
- 1:30 PM - 4:00 PM: Afternoon Procedures and Meetings. The afternoon may involve a specialized clinic (e.g., a muscular dystrophy clinic) or procedures. The neurologist might attend a multidisciplinary team meeting to discuss a complex neuro-oncology case with surgeons, oncologists, and radiation therapists.
- 4:00 PM - 5:30 PM: Finalizing Work. The last part of the day is dedicated to finishing notes, signing off on orders, responding to non-urgent messages, and preparing for the next day’s clinic. For those on call, the day may extend late into the night with emergency consultations from the ER.
---
Average Pediatric Neurologist Salary: A Deep Dive
The journey to becoming a pediatric neurologist is long and arduous, but the financial compensation is substantial, reflecting the high level of specialization and critical need for these physicians. The salary of a pediatric neurologist is among the highest in the medical field, though it can vary significantly based on a number of factors we will explore in the next section.
It's important to understand that physician compensation is complex. It's not just a flat salary; it's a package that often includes a base salary, productivity bonuses, and a suite of benefits.
National Average Salary and Typical Range
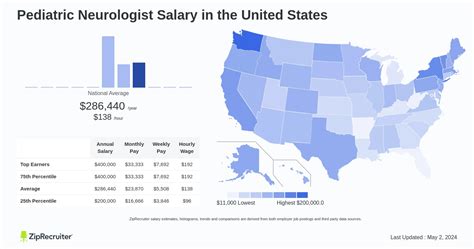
When analyzing physician salaries, it's best to consult multiple authoritative sources to get a balanced picture. Here’s a breakdown of what recent data shows for pediatric neurologists in the United States:
- Medscape Physician Compensation Report 2023: While this report often groups neurologists together, its data is considered a gold standard. The average salary for Neurologists (both adult and pediatric) was $313,000. Pediatric subspecialties often earn slightly less than their adult-focused counterparts due to differences in billing and procedure volume, but they remain firmly in this high-earning bracket.
- Salary.com: As of late 2023 and early 2024, data from Salary.com shows the average base salary for a Pediatric Neurologist in the U.S. is $262,459, with a typical range falling between $228,811 and $309,692. It's crucial to note this often represents the *base* salary, not the total compensation.
- Payscale: This platform reports a slightly lower average base salary of around $225,500, but also highlights that total pay, including bonuses, can reach up to $300,000 or more for experienced professionals.
- Doximity Physician Compensation Report 2023: This report places Child Neurology compensation at an average of $293,736, reinforcing its position as a high-earning specialty.
Synthesizing this data, a realistic national average for a pediatric neurologist's *total compensation* is likely in the $270,000 to $310,000 range. The wide salary band is influenced heavily by experience, location, and practice type.
### Salary by Experience Level
Like most professions, compensation in pediatric neurology grows significantly with experience. The sharpest increase typically occurs after the first few years of practice as a physician builds a reputation, becomes more efficient, and often takes on more senior responsibilities.
| Experience Level | Typical Years of Practice (Post-Fellowship) | Estimated Annual Salary Range (Total Comp) | Source Notes |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-3 Years | $220,000 - $265,000 | Represents the initial contract out of fellowship. Often includes a signing bonus. |
| Mid-Career | 4-10 Years | $260,000 - $310,000 | The physician has become more established, efficient with patient loads, and may qualify for higher productivity bonuses. |
| Senior/Experienced | 10+ Years | $290,000 - $350,000+ | At this stage, neurologists may hold leadership roles (e.g., Department Chair, Medical Director), have a share in a private practice, or be highly sought-after experts. |
*Source: Synthesized from Salary.com, Doximity, and industry hiring trends.*
### Deconstructing the Compensation Package
The number on a contract is rarely the full story. A pediatric neurologist's total compensation package is a mosaic of different components:
- Base Salary: The guaranteed, predictable portion of pay. In hospital-employed or academic settings, this makes up the bulk of the compensation.
- Productivity Bonuses: This is a major variable. Many employers use a system based on Relative Value Units (RVUs). An RVU is a measure of value used by Medicare that factors in the time, skill, and intensity required to provide a patient service. Physicians are often given a target number of RVUs to generate per year; if they exceed it, they receive a bonus. This incentivizes seeing more patients or performing more procedures.
- Signing Bonus: To attract top talent, especially in underserved areas, hospitals and practices often offer a one-time signing bonus, which can range from $10,000 to $50,000 or more.
- Relocation Allowance: A stipend to cover the costs of moving, typically ranging from $5,000 to $15,000.
- Retirement Plans: This is a significant part of long-term wealth building. Employers typically offer a 401(k) or 403(b) plan with a matching contribution (e.g., matching 50% of employee contributions up to 6% of salary).
- Continuing Medical Education (CME) Allowance: An annual stipend (usually $2,000 - $5,000) to cover the cost of attending conferences, buying journals, and fulfilling state licensing requirements for ongoing education.
- Professional Dues and Licenses: Employers often cover the cost of medical licenses, board certification fees, and membership dues for professional organizations like the American Academy of Neurology (AAN).
- Malpractice Insurance: Comprehensive "claims-made" or "occurrence-based" malpractice insurance is a standard and essential benefit provided by the employer.
- Health and Disability Insurance: Full health, dental, and vision insurance for the physician and their family, as well as crucial long-term disability insurance, are standard parts of the package.
When evaluating a job offer, it's vital to look beyond the base salary and calculate the total value of this comprehensive package.
---
Key Factors That Influence Salary

While we've established a strong baseline for the salary of a pediatric neurologist, the actual figure an individual earns can swing by tens of thousands of dollars based on a combination of critical factors. Understanding these variables is key for anyone looking to maximize their earning potential in this field. This section provides a granular look at what drives compensation up or down.
###
Level of Education and Advanced Training
In medicine, the educational path is highly standardized, so unlike in business, having a specific degree (MD vs. DO) rarely impacts salary directly once a physician is board-certified and practicing. All pediatric neurologists complete a rigorous path: an undergraduate degree, four years of medical school, a residency, and a fellowship.
However, further specialization *beyond* the standard three-year pediatric neurology fellowship can significantly enhance earning potential and job prospects. This is known as sub-specialization. A physician who completes an additional one-to-two-year fellowship in a high-demand area becomes a more valuable asset.
Examples of high-value sub-specialty fellowships:
- Epilepsy: Specialists who can manage complex, drug-resistant epilepsy, interpret long-term video EEGs, and oversee surgical epilepsy cases are in extremely high demand. This is one of the most common and lucrative sub-specialties.
- Neuromuscular Medicine: Focusing on conditions like muscular dystrophy and spinal muscular atrophy (SMA) can be financially rewarding, especially with the advent of new, high-cost genetic therapies.
- Neuro-Oncology: Treating brain and spinal cord tumors is a highly specialized and challenging field, often commanding a higher salary within large academic cancer centers.
- Headache Medicine: While it may sound common, specialists in pediatric headache are sought after to manage debilitating chronic migraines and other headache syndromes.
Completing one of these fellowships not only deepens expertise but also allows a neurologist to become the go-to expert in a region, attracting more complex (and often better-reimbursing) cases and potentially leading to directorship of a specialized center.
###
Years of Experience
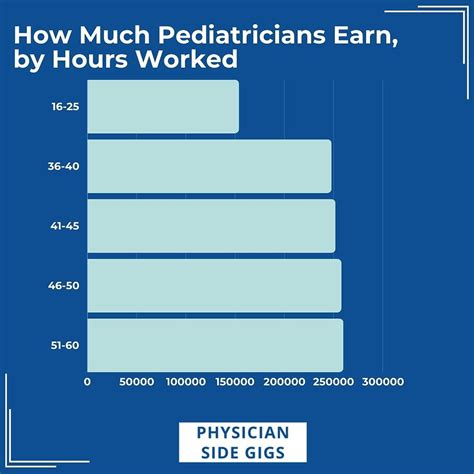
As detailed in the previous section, experience is one of the most powerful drivers of salary growth. The compensation trajectory is not a straight line but rather a curve that steepens after the initial years.
- Early Career (0-3 Years): A new graduate from fellowship is focused on building clinical speed and confidence. Their salary is typically based on the "going rate" for new hires in that market. They have less negotiating power and are still learning the business side of medicine. Salary Range: $220,000 - $265,000.
- Mid-Career (4-10 Years): This is the "sweet spot" for salary growth. The neurologist is now highly efficient, can handle a full patient load, and has a proven track record. They have likely surpassed their initial RVU targets, triggering significant bonuses. At this stage, they may switch jobs for a substantial pay increase or renegotiate their contract from a position of strength. Salary Range: $260,000 - $310,000.
- Senior Career (10+ Years): Earning potential continues to rise, but growth may be driven more by leadership than clinical volume. A senior neurologist might become the Chief of Pediatric Neurology, a Fellowship Program Director, or a Vice Chair of a department. These administrative roles come with additional stipends and higher base salaries. For those in private practice, this is when their ownership stake fully matures, leading to the highest possible earnings. Salary Range: $290,000 - $350,000+.
###
Geographic Location
Where you practice medicine has a colossal impact on your salary, often creating variations of $50,000 or more for the exact same job. This is driven by supply and demand, cost of living, and the concentration of healthcare systems.
Interestingly, the highest salaries are often *not* in the most glamorous, high-cost-of-living cities on the coasts. These areas (e.g., Boston, New York, San Francisco) have a high concentration of academic medical centers and are desirable places to live, leading to a surplus of specialists willing to accept lower salaries.
Conversely, less populated states and regions, particularly in the Midwest and Southeast, often have a shortage of specialists and must offer higher compensation to attract talent.
Illustrative Geographic Salary Comparison:
| Location Category | Example States/Regions | Estimated Average Salary | Rationale |
| :--- | :--- | :--- | :--- |
| High Paying | North Dakota, Wisconsin, Alabama, Oklahoma, Indiana | $300,000 - $340,000+ | High demand, low supply of specialists. Health systems must be competitive to recruit. Lower cost of living means salary goes further. |
| Average Paying | Texas, Ohio, Arizona, Georgia | $270,000 - $300,000 | A balance of large metro areas and secondary cities with competitive, but not top-tier, compensation. |
| Lower Paying | Massachusetts, New York, Maryland, parts of California | $240,000 - $280,000 | High concentration of academic institutions and desirable locations creates a competitive job market, depressing salaries relative to the cost of living. |
*Source: Analysis based on data from Doximity, Medscape, and physician recruitment firm reports.*
When considering a job, it's crucial to analyze the salary in the context of the local cost of living. A $280,000 salary in Jackson, Mississippi, affords a much higher quality of life than a $300,000 salary in Los Angeles.
###
Practice Type and Size
The type of organization a pediatric neurologist works for is another primary determinant of both salary structure and overall earning potential.
- Hospital-Employed/Health System: This is now the most common employment model. The neurologist is a direct employee of a hospital or a large, integrated health system.
- Pros: Stable, predictable salary; strong benefits package; no administrative burden of running a business; built-in referral base.
- Cons: Less autonomy; salary is often capped by institutional pay scales; compensation is heavily tied to productivity metrics (RVUs) that you don't control.
- Salary Potential: Strong and stable, typically aligning with the national averages ($260k - $320k).
- Academic Medical Center: This involves working for a university-affiliated hospital. The role is a mix of clinical care, teaching, and research.
- Pros: Intellectually stimulating environment; opportunities for groundbreaking research and publication; prestige; often better work-life balance.
- Cons: Salaries are notoriously lower than in private practice or even some hospital systems. The "academic discount" is a real phenomenon.
- Salary Potential: Generally the lowest, often 10-20% below other models. A starting academic salary might be closer to $210,000 - $240,000.
- Private Practice (Group or Solo): This is the traditional entrepreneurial model, though it's becoming less common for new graduates.
- Pros: Highest earning potential; complete autonomy over clinical decisions and business operations; opportunity to build equity. After several years, partners in a successful private practice can be the highest earners in the field.
- Cons: High risk; significant administrative responsibilities (billing, staffing, marketing); income can be volatile; requires business acumen.
- Salary Potential: Highest ceiling. While a new associate might start with a guaranteed salary, a senior partner in a busy practice could earn well over $400,000.
###
Area of Specialization
As mentioned briefly, the specific niche within pediatric neurology can influence pay. This is primarily a function of the procedures a specialist performs and the demand for their skills.
Neurologists who perform and interpret procedures are compensated for those procedures in addition to their standard evaluation and management services. The most common and impactful procedure is EEG interpretation. A pediatric neurologist who spends a significant portion of their time reading EEGs (especially in a high-volume epilepsy center) will almost certainly have a higher income than one who primarily does consultative work without procedures. This is a direct driver of RVU generation.
Specialties like Epilepsy and Neuromuscular Medicine are therefore often more lucrative than, for example, a practice focused solely on developmental/behavioral neurology or headaches, which are less procedure-heavy.
###
In-Demand Skills and Other Factors
Beyond the major categories, several other skills and attributes can provide a salary edge:
- Leadership and Administrative Skills: Taking on a role as a Medical Director, Division Chief, or a hospital committee chair often comes with an administrative stipend or a higher base salary.
- Proficiency in Tele-neurology: As virtual health becomes more integrated, physicians comfortable and efficient with telehealth platforms are valuable, especially for systems looking to expand their reach into rural areas.
- Clinical Research Experience: While academic research may lower the base salary, being a principal investigator on industry-sponsored clinical trials can provide significant supplemental income.
- Bilingualism: In many parts of the country, being fluent in a second language (especially Spanish) can make a candidate more attractive and may command a slightly higher salary or bonus.
---
Job Outlook and Career Growth

For those investing over a decade in training, job security and future prospects are paramount. The outlook for pediatric neurologists is exceptionally strong, arguably one of the most secure in all of medicine. This is driven by a simple and powerful economic reality: demand for their services significantly outstrips the available supply.
Analysis of Job Growth and Demand
The U.S. Bureau of Labor Statistics (BLS) projects that employment for all Physicians and Surgeons will grow by 3% from 2022 to 2032, which is about as fast as the average for all occupations. However, this broad statistic masks the acute reality within specific sub-specialties. For pediatric neurology, the situation is far more urgent.
Multiple studies and reports from organizations like the Child Neurology Society (CNS) and the American Academy of Neurology (AAN) have consistently highlighted a nationwide shortage of pediatric neurologists. A 2020 study published in *Neurology* noted the persistent gap between the number of specialists needed and the number available, a trend that is expected to continue.
Key Reasons for the Strong Job Outlook:
1. Persistent Shortage: There are simply not enough pediatric neurologists being trained to meet the needs of the population. This means that newly graduated fellows often receive multiple job offers and have considerable leverage in negotiations.
2. Increasing Prevalence of Neurological Disorders: Greater awareness and better diagnostic tools have led to an increase in the diagnosis of conditions like autism spectrum disorder, epilepsy, and developmental delays, all of which require specialist care.
3. Advances in Treatment: The development of new therapies, particularly for rare genetic and neuromuscular diseases, means that more patients are living longer and require ongoing, complex neurological management.
4. Geographic Mismatch: While major cities may have a reasonable number of specialists, vast swaths of the country, particularly rural areas,