The decision to pursue a career in pediatric neurosurgery is rarely, if ever, made lightly. It is a path forged through more than a decade of relentless academic pursuit, grueling training, and an unwavering commitment to one of the most demanding disciplines in modern medicine. You are drawn to the profound challenge of operating on the most delicate and complex organ—the developing brain and nervous system of a child. It is a world where millimeters decide futures and where the intersection of courage, compassion, and scientific brilliance creates miracles.
While the intrinsic rewards of saving and improving young lives are the primary motivator, the practical considerations of compensation are a significant and valid part of the career equation. The salary of a pediatric neurosurgeon reflects the immense responsibility, extensive training, and specialized expertise required for the role. With average annual earnings comfortably in the high six-figures and often exceeding a million dollars for experienced practitioners, this field represents the pinnacle of medical earning potential. But what does that number truly represent?
As a career analyst who has guided countless medical professionals, I once had a conversation with a Chief of Neurosurgery that has always stuck with me. He said, "We don't pay our pediatric neurosurgeons for the hours they're in the OR. We pay them for the 15 years it took to get there and for the sleepless nights they spend thinking about a single child's case." That sentiment perfectly encapsulates the value proposition of this career—it's a compensation package for a lifetime of dedication.
This comprehensive guide will deconstruct every facet of a pediatric neurosurgeon's salary and career path. We will move beyond the national averages to explore the intricate factors that shape your earning potential, from geography and practice type to the nuances of sub-specialization. Whether you are a student dreaming of this path, a resident navigating your training, or a professional considering a specialization, this article will serve as your definitive resource.
### Table of Contents
- [What Does a Pediatric Neurosurgeon Do?](#what-does-a-pediatric-neurosurgeon-do)
- [Average Pediatric Neurosurgeon Salary: A Deep Dive](#average-pediatric-neurosurgeon-salary-a-deep-dive)
- [Key Factors That Influence a Pediatric Neurosurgeon's Salary](#key-factors-that-influence-a-pediatric-neurosurgeons-salary)
- [Job Outlook and Career Growth for Pediatric Neurosurgeons](#job-outlook-and-career-growth-for-pediatric-neurosurgeons)
- [How to Become a Pediatric Neurosurgeon: A Step-by-Step Guide](#how-to-become-a-pediatric-neurosurgeon-a-step-by-step-guide)
- [Conclusion: Is the Journey Worth the Reward?](#conclusion-is-the-journey-worth-the-reward)
What Does a Pediatric Neurosurgeon Do?

A pediatric neurosurgeon is a highly specialized medical doctor who diagnoses, treats, and surgically manages disorders of the central, peripheral, and autonomic nervous systems in children, from the fetal period through adolescence. Their domain is the brain, spine, and nerves of the youngest and most vulnerable patients. This specialization is distinct from adult neurosurgery because a child's nervous system is not merely a smaller version of an adult's; it is a dynamic, developing entity that presents unique challenges and requires a specialized approach.
The scope of their work is incredibly broad and involves treating a range of congenital, developmental, traumatic, and acquired conditions. Their responsibilities extend far beyond the operating room and encompass a full spectrum of patient care, research, and collaboration.
Core Responsibilities and Conditions Treated:
- Congenital Abnormalities: Treating conditions present at birth, such as hydrocephalus (excess fluid in the brain), spina bifida and other neural tube defects, and craniofacial anomalies like craniosynostosis (premature fusion of skull bones).
- Neuro-Oncology: Diagnosing and surgically excising brain and spinal cord tumors, which are the most common solid tumors in children. This often involves working within a multidisciplinary team of pediatric oncologists, radiation oncologists, and pathologists.
- Epilepsy Surgery: Performing complex procedures to control or eliminate seizures in children with medication-resistant epilepsy. This can include resections, disconnections (like a corpus callosotomy), or the implantation of neurostimulation devices.
- Vascular Neurosurgery: Managing conditions like arteriovenous malformations (AVMs), cavernous malformations, and Moyamoya disease in children.
- Trauma: Providing emergency surgical care for traumatic brain injuries (TBI) and spinal cord injuries resulting from accidents, falls, or abuse.
- Spasticity Management: Performing procedures like selective dorsal rhizotomy or implanting baclofen pumps to alleviate severe muscle spasticity associated with conditions like cerebral palsy.
### A Day in the Life of a Pediatric Neurosurgeon
To make this role more tangible, consider a typical (though no day is truly typical) day for Dr. Elena Vance, a pediatric neurosurgeon at a major children's hospital.
- 6:00 AM - Morning Rounds: Dr. Vance arrives at the hospital. Her first stop is the Pediatric Intensive Care Unit (PICU) to check on a 4-year-old patient who underwent a complex tumor resection yesterday. She reviews the overnight vitals, neuro-checks, and new imaging with the critical care team, making adjustments to the patient's care plan.
- 7:00 AM - Pre-Operative Consult: She meets with the parents of a 6-month-old infant scheduled for surgery to correct craniosynostosis. With immense empathy and clarity, she explains the procedure, uses a 3D model of the skull to illustrate the surgical plan, discusses the risks, and answers their anxious questions.
- 8:00 AM - 3:00 PM - Surgery: The main event of the day. Today's major case is a 7-hour procedure to remove an ependymoma, a type of tumor, from the spine of a 9-year-old. This requires microscopic precision, intraoperative neuro-monitoring to protect nerve function, and intense, unwavering focus. She works in concert with her surgical team, including an anesthesiologist, surgical nurses, and a neurophysiologist.
- 3:30 PM - Post-Operative Update: Immediately after the surgery, Dr. Vance finds the 9-year-old's family in the waiting room. She delivers the news that the tumor was successfully removed and the patient is stable, providing a moment of profound relief.
- 4:00 PM - Afternoon Clinic: Dr. Vance heads to her outpatient clinic. For the next three hours, she sees a mix of patients: a teenager for a follow-up after a concussion, a 2-year-old for an adjustment to their programmable shunt, and a family seeking a second opinion on a complex spinal condition. Each 30-minute appointment is a blend of clinical examination, imaging review, and deep, empathetic conversation.
- 7:00 PM - Administrative Work & Research: The clinical day is over, but the work isn't. Dr. Vance spends an hour updating patient charts, dictating surgical notes, responding to urgent emails, and reviewing referrals from pediatricians. She also carves out time to review data for a research paper she is co-authoring on long-term outcomes for epilepsy surgery.
- 8:00 PM - On Call: Dr. Vance heads home, but she is the on-call neurosurgeon tonight. Her phone could ring at any moment with a call from the ER about a child with a severe head trauma, meaning she may have to return to the hospital to perform emergency surgery in the middle of the night.
This demanding schedule highlights that the role is a fusion of technical mastery, profound human connection, intellectual rigor, and relentless dedication.
Average Pediatric Neurosurgeon Salary: A Deep Dive
The compensation for pediatric neurosurgeons is among the highest in any profession, a direct reflection of the extensive training, high-stakes environment, and scarcity of qualified specialists. While figures vary, the data consistently points to a robust seven-figure potential for experienced practitioners.
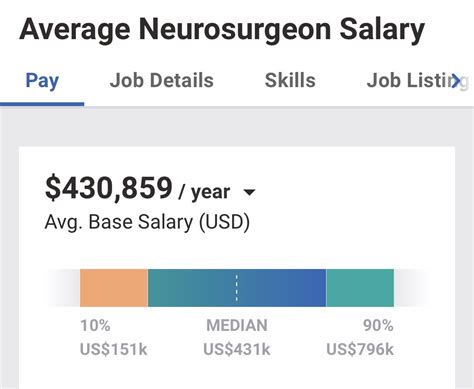
It's important to note that "Neurosurgery" is often reported as a single category in salary surveys, with pediatric neurosurgery being a sub-specialty within it. Pediatric specialists typically fall within the upper range of these neurosurgery salary bands due to the added fellowship training and complexity of their patient population.
### National Averages and Salary Ranges
Multiple authoritative sources provide a clear picture of the earning landscape. Here’s a synthesis of the most recent data:
- Medscape's 2023 Physician Compensation Report, one of the most comprehensive surveys, places neurosurgery consistently among the top 3 highest-paid specialties. While not singling out pediatrics, the overall average for neurosurgeons was $788,313.
- Salary.com provides more granular data, listing the median salary for a "Neurosurgeon" in the United States as $699,501, with a typical range falling between $527,001 and $885,801. Their data for top earners pushes well into the high six figures.
- The Medical Group Management Association (MGMA) is considered a gold standard for physician compensation data, though its detailed reports are proprietary. Public summaries and industry analyses consistently place median academic pediatric neurosurgeon compensation around $750,000 - $850,000 and private practice compensation significantly higher, often approaching or exceeding $1,000,000.
- Doximity's 2023 Physician Compensation Report reported an average compensation for neurosurgeons of $763,908, further cementing its position at the top of the medical pay scale.
Based on an aggregation of these sources, a conservative and realistic salary spectrum for a pediatric neurosurgeon in the United States looks like this:
- National Average Salary: Approximately $875,000 per year.
- Typical Salary Range: $600,000 (entry-level academic) to $1,200,000+ (experienced, private practice).
### Salary by Experience Level
Compensation grows significantly with experience, reputation, and efficiency. Here is a breakdown of the typical salary progression.
| Career Stage | Years of Experience | Typical Annual Salary Range | Notes |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-3 years post-fellowship| $450,000 - $650,000 | Starting in an academic setting. Focus is on building a practice and gaining experience. Often includes a guaranteed salary for the first 1-2 years. |
| Mid-Career | 4-10 years | $700,000 - $950,000 | Transition to productivity-based pay (wRVUs). Has established a referral base and is surgically efficient. May take on junior leadership roles. |
| Senior / Late-Career| 11-20+ years | $900,000 - $1,500,000+| Peak earning years. Recognized expert with a strong reputation. May be a department chair or lead a specialized center. High surgical volume and complexity. |
*(Salary ranges are estimates synthesized from multiple sources including Medscape, MGMA data summaries, and industry reports.)*
### Beyond the Base Salary: Understanding the Full Compensation Package
The annual salary is only one part of a pediatric neurosurgeon’s total compensation. The benefits and bonus structure are substantial and contribute significantly to their overall financial picture.
- Base Salary: The guaranteed annual income. In academic or hospital-employed models, this is a significant portion of the total pay.
- Productivity Bonus (wRVU-Based): This is the most common and impactful bonus structure. Physicians earn wRVUs (weighted Relative Value Units) for each procedure and service they provide. The wRVU value is set by Medicare and reflects the time, skill, and intensity required for a service. The surgeon is paid a certain dollar amount per wRVU generated above a set threshold. A highly efficient surgeon who performs many complex procedures can earn hundreds of thousands of dollars in productivity bonuses alone.
- Sign-On Bonus: To attract top talent, particularly in competitive markets or underserved areas, hospitals and practices offer substantial sign-on bonuses, often ranging from $50,000 to $200,000 or more.
- Quality & Performance Bonuses: Increasingly, compensation includes bonuses tied to patient outcomes, safety metrics, and patient satisfaction scores, although this is a smaller component than productivity.
- Retirement Contributions: Generous retirement plans, such as 401(k) or 403(b) plans, with significant employer matching contributions (often 5-10% of salary).
- Continuing Medical Education (CME) Allowance: An annual stipend (e.g., $5,000 - $15,000) to cover the costs of attending conferences, subscribing to journals, and other educational activities required to maintain their license and skills.
- Malpractice Insurance: Comprehensive "claims-made" or "occurrence" malpractice insurance is a non-negotiable part of the package. The annual premiums for neurosurgery can be astronomical ($50,000 - $150,000+), and this is almost always fully covered by the employer. This is a massive, non-taxable financial benefit.
- Relocation Allowance: Financial assistance for moving expenses if the position requires relocating.
- Comprehensive Health Benefits: Top-tier health, dental, vision, life, and disability insurance for the surgeon and their family.
When all these elements are combined, the total value of a pediatric neurosurgeon's compensation package can be 20-30% higher than the base salary figure alone suggests.
Key Factors That Influence a Pediatric Neurosurgeon's Salary

While the national averages provide a benchmark, a surgeon's actual take-home pay is determined by a complex interplay of several key variables. Understanding these factors is critical for anyone planning their career trajectory and negotiating their compensation. This section, the most detailed in our guide, will break down each element.
### ### 1. The Educational Path and Advanced Credentials
The foundation of a neurosurgeon's salary is built upon an exceptionally long and arduous educational and training pathway. There are no shortcuts, and each step is a prerequisite for the next. This journey itself is the primary justification for the high compensation floor.
- Undergraduate Degree (4 years): A bachelor's degree with a strong pre-med focus (biology, chemistry, physics).
- Medical Degree (4 years): Earning an M.D. (Doctor of Medicine) or D.O. (Doctor of Osteopathic Medicine). Top performance and high USMLE/COMLEX scores are essential.
- Neurosurgical Residency (7 years): This is the core of the training. It is one of the longest and most competitive residency programs. During this time, residents earn a modest salary (typically $60,000 - $85,000 per year), while working 80-100 hours per week.
- Pediatric Neurosurgery Fellowship (1-2 years): After completing the neurosurgery residency, an additional fellowship dedicated solely to pediatric cases is required. This hyper-specialization is what qualifies a surgeon for the "pediatric" title and the associated salary premium.
- Board Certification: This is a critical factor for maximizing earnings. To achieve top-tier compensation, a surgeon must be board-certified by the American Board of Neurological Surgery (ABNS). Following that, they can pursue sub-specialty certification from the American Board of Pediatric Neurological Surgery (ABPNS). Certification signifies that the surgeon has met the highest standards of knowledge and practice in the field and is essential for securing positions at leading institutions and commanding top pay. Lack of board certification can be a significant barrier to employment and will result in substantially lower salary offers.
In essence, the ~16 years of post-high school training is the "buy-in" for the career. The salary reflects a return on this enormous investment of time, effort, and forgone income.
### ### 2. Years of Experience and Reputation
As illustrated in the salary table, experience is one of the most powerful drivers of income growth. This is not simply a reward for longevity; it is tied directly to tangible increases in value.
- Early Career (0-3 Years): Post-fellowship surgeons are often on a guaranteed salary for the first 1-2 years as they build their practice. They are learning to manage their own cases, build relationships with referring pediatricians, and become more efficient in the operating room. Their RVU production is typically lower as they start out.
- Mid-Career (4-10 Years): This is where a significant salary jump occurs. The surgeon has hit their stride. They are surgically faster and more efficient, allowing them to handle a higher volume of cases. They have built a robust referral network, ensuring a steady stream of patients. They are now typically on a productivity-based contract, where their income is directly linked to the work they perform. A surgeon at this stage might see their annual compensation increase by 50-75% from their starting salary. For example, a surgeon starting at $600,000 could easily be earning $900,000 or more by year seven.
- Senior Career & Leadership (11+ Years): Surgeons in this phase are at their peak. They are often sought out for the most complex cases regionally or even nationally. Their reputation alone drives referrals. At this stage, salary growth comes not just from surgical volume but from taking on leadership roles:
- Chief of Pediatric Neurosurgery: This role comes with a significant administrative stipend and leadership responsibilities.
- Department Chair of Neurosurgery: Overseeing the entire neurosurgery department (both adult and pediatric) at a major medical center.
- Medical Director Roles: Leading specialized programs like a hospital's epilepsy center or brain tumor institute.
These leadership positions can add another $100,000 to $300,000+ to their annual compensation.
### ### 3. Geographic Location
Where a pediatric neurosurgeon chooses to practice has a profound impact on their salary. The dynamics are often counter-intuitive; the highest salaries are not always found in the major coastal cities with the highest cost of living.
- Regional Variations: According to Medscape and Doximity data, the Midwest and Southeast regions of the U.S. often offer the highest compensation for physicians. This is driven by supply and demand; there are fewer specialists in these areas, and health systems must offer more competitive packages to attract and retain them. Conversely, desirable, high-cost-of-living areas like the Northeast (e.g., Boston, New York) and the West Coast (e.g., San Francisco, Los Angeles) can sometimes have slightly lower salaries due to a higher concentration of surgeons and a greater prevalence of academic institutions, which traditionally pay less than private practice.
- Urban vs. Rural/Suburban: Large metropolitan areas have numerous hospitals, but also more competition. A position in a less-saturated major city or a large suburban health system can be a financial sweet spot, offering high demand and strong compensation. Truly rural areas may have a critical need but may not have the infrastructure (like a dedicated children's hospital) to support a full-time pediatric neurosurgery practice.
- State-by-State Examples: While specific data for *pediatric* neurosurgery is sparse, overall neurosurgeon salary data is illustrative. States like Wisconsin, North Carolina, Indiana, and Georgia are often cited as having very high compensation levels for specialists. For example, a position in Charlotte, NC, might pay significantly more than a similar position in New York City, with the added benefit of a much lower cost of living, dramatically increasing disposable income.
| Location Type | Salary Potential | Rationale |
| :--- | :--- | :--- |
| Major Coastal City (e.g., NYC, LA) | Good to High | Saturated market, more academic positions. High cost of living can erode purchasing power. |
| Mid-Sized City (e.g., Indianapolis, St. Louis) | Very High | Strong demand, less competition, lower cost of living. Often a financial "sweet spot." |
| Large Suburban Health System | High to Very High | Caters to an affluent population, high demand for services, competitive compensation to draw talent from cities. |
| Academic Hub (e.g., Boston, Baltimore) | Good | Dominated by university hospitals with traditionally lower, more fixed salary structures. |
### ### 4. Practice Setting and Employment Type
The type of organization a surgeon works for is arguably the most significant determinant of their earning potential and work-life balance.
- Academic Medical Centers: These are university-affiliated hospitals.
- Salary: Generally the *lowest* starting point, but still substantial (e.g., $550k - $750k). Compensation is more structured and less dependent on raw surgical volume.
- Pros: Opportunities for teaching medical students and residents, dedicated research time and resources, access to cutting-edge technology, strong benefits, and often better work-life balance. Prestige and intellectual stimulation are high.
- Cons: Lower ceiling on income potential compared to private practice due to bureaucratic salary bands and non-clinical duties.
- Private Practice (Physician-Owned Group): A group of surgeons who own their own practice.
- Salary: The *highest* earning potential. Senior partners in successful private practice groups can earn well over $1.5 million to $2 million annually. Income is almost entirely based on productivity.
- Pros: Maximum autonomy, direct control over business decisions, highest income ceiling.
- Cons: Significant administrative and business responsibilities (hiring, billing, marketing), financial risk, and pressure to maintain high surgical volume. This model is becoming less common as hospitals acquire private groups.
- Hospital-Employed (Private or Non-Profit): This is now the most common employment model. The surgeon is a direct employee of a hospital or large health system.
- Salary: A hybrid model, offering strong compensation that is often higher than academia but lower than a private practice partner (e.g., $700k - $1.2M+).
- Pros: Stable salary with productivity bonuses, no administrative burden of running a business, strong malpractice coverage and benefits, access to hospital resources.
- Cons: Less autonomy than private practice, beholden to hospital administration and policies.
- Locum Tenens: Temporary work, filling in for other surgeons on leave or in understaffed hospitals.
- Salary: Paid a very high daily or weekly rate (e.g., $3,000 - $5,000+ per day), but this does not include benefits, malpractice "tail" coverage, or retirement contributions.
- Pros: Flexibility, high short-term pay, ability to travel and experience different practice environments.
- Cons: Lack of stability, no benefits, constant travel, can be professionally isolating.
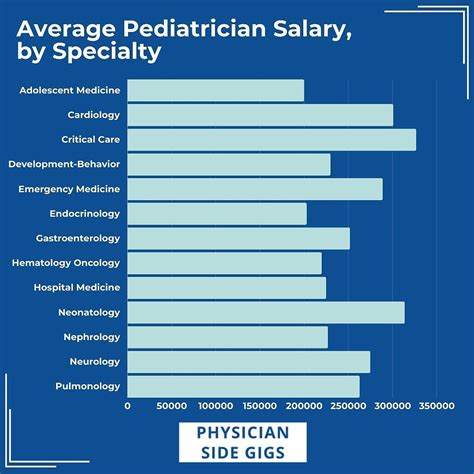
### ### 5. Area of Sub-specialization
Even within the niche of pediatric neurosurgery, further sub-specialization can enhance a surgeon's expertise and value, leading to higher compensation, particularly through directing specialized centers.
- Pediatric Neuro-Oncology: Focusing exclusively on brain and spinal tumors. These surgeons are critical members of cancer centers and command high salaries for their ability to perform the most complex resections.
- Pediatric Epilepsy Surgery: Specializing in procedures to cure or mitigate epilepsy.