Table of Contents

- [Introduction](#introduction)
- [What Does a Physician Actually Do?](#what-does-a-physician-do)
- [Average Physician Salary: A Deep Dive into the Data](#average-physician-salary-a-deep-dive)
- [The Key Factors That Influence Physician Salary](#key-factors-that-influence-salary)
- [Physician Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Become a Physician: A Step-by-Step Guide](#how-to-get-started)
- [Conclusion: Building a Financially and Personally Rewarding Career](#conclusion)
Introduction

For every student doctor navigating the grueling demands of medical school—the late-night study sessions fueled by caffeine, the weight of a growing debt burden, and the emotional toll of clinical rotations—the question of future compensation is not just a curiosity; it's a critical component of long-term financial planning. You've likely heard whispers of six-figure salaries and seen impressive numbers associated with the medical profession. You may have even come across the term "MGMA salary data" as the gold standard for physician compensation. But what does it all mean for you, right now, as you work towards your M.D. or D.O.?
Let’s be crystal clear from the outset: student doctors do not earn a salary. The role is one of intensive, full-time training. The "salary data" from prestigious sources like the Medical Group Management Association (MGMA) doesn't apply to students or even residents in the traditional sense. Instead, it represents the light at the end of the tunnel—the earning potential you will unlock once you are a licensed, practicing physician. Understanding this data *now* is one of the most powerful financial moves you can make. It transforms an abstract future into a tangible goal, helping you strategize your specialty choice, negotiate your first contract, and manage your educational debt with confidence.
I remember mentoring a third-year medical student who was overwhelmed by her $250,000 in loans. Looking at the MGMA data for her desired specialty, family medicine, wasn't about greed; it was about empowerment. Seeing the concrete salary progression, bonus structures, and regional differences allowed her to map out a realistic 10-year plan to become debt-free, turning her anxiety into a focused strategy.
This guide is designed to be that mentor for you. We will demystify the numbers and provide a comprehensive, authoritative breakdown of physician compensation. We will explore what the data means, the powerful factors that shape your future income, the outlook for the profession, and the concrete steps to get there. Consider this your definitive resource for translating today's sacrifice into tomorrow's success.
What Does a Physician Actually Do?

Before we dive into the intricate details of compensation, it's crucial to have a clear, holistic understanding of the profession you are entering. Being a physician is far more than just a "job"; it is a vocation that blends scientific expertise, deep-seated empathy, and complex problem-solving. While your medical school rotations provide a glimpse into various specialties, the day-to-day reality of a practicing physician encompasses a wide spectrum of responsibilities.
### An Overview of Core Responsibilities
At its heart, a physician's role is to diagnose and treat human disease, injury, and other physical and mental impairments. They are the leaders of the healthcare team, responsible for the ultimate well-being of their patients. Key responsibilities include:
- Patient Examination and History: Conducting thorough physical exams and taking detailed medical histories to understand a patient's health status.
- Diagnosis: Ordering, performing, and interpreting diagnostic tests (like lab work, X-rays, and MRIs) to identify the root cause of symptoms.
- Treatment Planning: Developing and implementing treatment plans, which may include prescribing medication, providing therapies, referring to other specialists, or performing surgical procedures.
- Patient Counseling: Educating patients and their families about diseases, prognoses, and treatment options, as well as promoting general health and wellness through preventive care.
- Collaboration: Working closely with a team of other healthcare professionals, including nurses, physician assistants, medical assistants, pharmacists, and other specialists, to ensure coordinated and effective care.
- Administrative Duties: Meticulously documenting patient encounters in Electronic Health Records (EHRs), handling insurance paperwork, and managing the business aspects of a practice.
- Continuing Medical Education (CME): Engaging in lifelong learning to stay abreast of the latest medical advancements, treatment guidelines, and technologies, a requirement for maintaining medical licensure.
### A "Day in the Life" of a Family Medicine Physician
To make this tangible, let's walk through a typical day for Dr. Anya Sharma, a Family Medicine physician in a suburban private group practice.
- 7:30 AM - 8:00 AM: Dr. Sharma arrives at the clinic. She grabs a coffee and logs into the EHR system. She spends 30 minutes reviewing lab results and imaging reports that came in overnight, making notes to discuss with patients and signing off on prescription refills.
- 8:00 AM - 12:00 PM: Morning clinic begins. She sees a steady stream of patients, with appointments booked every 15-20 minutes. Her morning includes a well-child check for a 2-year-old, managing hypertension in a 65-year-old patient, diagnosing an acute case of strep throat in a teenager, and conducting a sensitive mental health screening for a patient with anxiety. Between each visit, she rapidly documents her notes in the EHR.
- 12:00 PM - 1:00 PM: Lunch is often a working hour. She catches up on "in-basket" messages from patients and staff, returns urgent phone calls, and consults with a cardiologist over the phone about a shared patient with complex needs.
- 1:00 PM - 4:30 PM: Afternoon clinic. This session brings more variety: a patient requiring stitches for a minor laceration, a pre-operative clearance for a patient scheduled for knee surgery, and a long, complex visit with an elderly patient who has multiple chronic conditions.
- 4:30 PM - 5:30 PM (or later): "Pajama Time." This is the physician slang for the administrative work that happens after the last patient has left. Dr. Sharma finishes her charts, reviews the next day's schedule, addresses any outstanding lab reports, and completes any necessary prior authorization forms for medications or procedures. She might not leave the office until 6:00 PM or later, depending on the day's complexity.
This example highlights the intense blend of clinical acumen, time management, and administrative resilience required in the medical profession. The work is demanding, but the opportunity to build long-term relationships with patients and make a direct impact on their lives is what draws so many to the field.
Average Physician Salary: A Deep Dive into the Data
Now we arrive at the core of your query: the numbers. For an aspiring physician, understanding the financial landscape is not just motivating; it's essential for making informed career decisions. Physician compensation is complex, with significant variations, but we can establish a clear baseline by examining data from the most reputable sources in the industry.
It is critical to note that the most detailed data, particularly from the MGMA (Medical Group Management Association), is proprietary and often published in comprehensive reports available to member organizations. However, key findings are frequently reported by reputable industry publications, and we can supplement this with excellent public data from other sources.
### National Averages and Ranges: Primary Care vs. Specialists
The single biggest determinant of a physician's salary is their chosen specialty. For this reason, compensation data is almost always split into two main categories: Primary Care (e.g., Family Medicine, Internal Medicine, Pediatrics) and Specialists (e.g., Cardiology, Orthopedic Surgery, Anesthesiology).
Here’s a look at the national averages from several key 2023 and 2024 reports:
- Doximity 2023 Physician Compensation Report: This report, based on data from over 190,000 U.S. physicians, found the average compensation for all physicians to be $501,459.
- Average for Primary Care Physicians: $346,929
- Average for Specialists: $549,992
- Medscape Physician Compensation Report 2023: Medscape's survey of over 10,000 physicians provides similar insights.
- Average for Primary Care Physicians: $265,000
- Average for Specialists: $382,000
- MGMA Data Dive Provider Compensation Report (based on 2022 data): As reported by sources like *Physicians Thrive*, the MGMA data, which surveys over 190,000 providers, shows:
- Median Total Compensation for Primary Care Physicians: $291,155
- Median Total Compensation for Specialists: $528,095
Why the differences? Each report uses slightly different methodologies, sample sizes, and definitions of "compensation" (e.g., some may more heavily weigh bonuses and incentives). The key takeaway is consistency in the trend: specialists, on average, earn significantly more than primary care physicians due to factors like longer training, procedural focus, and supply-and-demand dynamics.
### Salary Progression by Experience Level
Physician income is not static; it grows with experience, efficiency, and in many cases, a move toward partnership. While "entry-level" isn't a perfect term for a doctor who has completed 7-12 years of higher education and training, we can look at compensation in the early years post-residency versus later in one's career.
| Career Stage | Typical Years of Experience | Estimated Salary Range (Primary Care) | Estimated Salary Range (Specialist) | Key Drivers |
| :--- | :--- | :--- | :--- | :--- |
| Early Career | 1-5 years post-residency | $200,000 - $280,000 | $350,000 - $500,000 | Often a guaranteed base salary. Focus is on building a patient panel and becoming efficient with clinical workflows and EHRs. |
| Mid-Career | 6-15 years | $260,000 - $350,000 | $450,000 - $650,000 | Transition to productivity-based pay (RVUs). May become a partner in a private practice, increasing income potential. Reputation is established. |
| Senior/Late Career | 16+ years | $280,000 - $400,000+ | $500,000 - $750,000+ | Maximized productivity, potential ownership/partnership income. May transition to part-time, administrative, or teaching roles, which can affect income. |
*Note: These ranges are estimates compiled from industry observations and compensation reports. Actual figures can vary significantly based on the factors discussed in the next section.*
### Beyond the Base Salary: Understanding Total Compensation
A physician's "salary" is often just one piece of a much larger financial picture. Understanding the full compensation package is crucial when evaluating a job offer.
- Base Salary: The guaranteed, fixed amount you are paid. This provides stability, especially in the first 1-2 years of a new job.
- Productivity Bonuses (RVU-Based): This is the most common form of incentive pay. An RVU (Relative Value Unit) is a measure used by Medicare to determine the value of a physician's services. Each procedure, visit, and service is assigned an RVU value. Many contracts state that once a physician generates a certain threshold of RVUs, they will receive a bonus for each additional RVU generated. This directly rewards physicians for being busy and efficient.
- Quality Bonuses: Increasingly common with the shift to "value-based care." These bonuses are tied to specific quality metrics, such as patient satisfaction scores, adherence to preventive care guidelines (e.g., cancer screenings), or effective management of chronic diseases like diabetes (e.g., A1c levels).
- Signing Bonus: A one-time, lump-sum payment offered to entice a physician to join a practice or hospital, particularly in high-need specialties or locations. These can range from $10,000 to over $100,000.
- Partnership/Ownership Track: In private practice, physicians may be offered a track to become a partner after a few years. As a partner, you share in the practice's profits, which can substantially increase your total income beyond what you could earn as an employee.
- Call Pay: Compensation for being "on-call" for the hospital or practice after hours or on weekends. This can be a daily stipend or an hourly rate for any work performed.
- Benefits Package: The value of this should not be underestimated. It includes:
- Health, Dental, and Vision Insurance: For you and your family.
- Retirement Plans: 401(k) or 403(b) plans, often with a generous employer match.
- Malpractice Insurance: Typically covered by the employer, a significant expense.
- CME Allowance: An annual stipend (e.g., $3,000-$5,000) to cover the cost of conferences, journals, and other required educational activities.
- Loan Repayment Assistance: Some employers, especially in underserved areas, offer significant student loan repayment programs, which can be worth tens of thousands of dollars per year.
When you're a resident preparing to enter the job market, you must learn to evaluate the *entire* offer, not just the base salary. A lower base salary with a strong productivity bonus structure and excellent benefits could ultimately be far more lucrative than a high base salary with no upside.
The Key Factors That Influence Physician Salary

While specialty choice is the primary driver of income potential, a multitude of other factors create a complex matrix of physician compensation. For a student doctor planning their future, understanding these variables is like having a roadmap to maximize earning potential and find the career path that best aligns with your financial and lifestyle goals. This section will provide an exhaustive breakdown of the elements that will shape your paystub.
### 1. Area of Specialization and Sub-Specialization
This is, without question, the most significant factor. The gap between the highest and lowest-paying specialties can be more than $500,000 per year. This disparity is driven by years of training, the procedural nature of the work, the acuity of the patient population, and market demand.
Here is a look at compensation across various specialties, with data aggregated from the Doximity and Medscape 2023 reports to show a representative range.
#### Top-Earning Specialties:
These are almost exclusively procedure-heavy surgical and medical sub-specialties.
| Specialty | Average Annual Compensation | Notes |
| :--- | :--- | :--- |
| Neurosurgery | $750,000 - $950,000+ | Requires the longest residency; highly complex procedures. |
| Thoracic Surgery | $700,000 - $900,000 | Operates on the heart, lungs, and other chest organs. |
| Orthopedic Surgery | $600,000 - $750,000 | High volume of lucrative procedures like joint replacements. |
| Plastic Surgery | $570,000 - $700,000 | A mix of reconstructive and cosmetic (often cash-pay) procedures. |
| Cardiology (Invasive/Interventional) | $550,000 - $700,000+ | Specialists who perform procedures like stenting and catheterizations. |
#### Mid-Range Specialties:
This group includes many hospital-based specialties and non-invasive medical sub-specialties.
| Specialty | Average Annual Compensation | Notes |
| :--- | :--- | :--- |
| Gastroenterology | $490,000 - $570,000 | High volume of procedures like colonoscopies and endoscopies. |
| Radiology | $480,000 - $550,000 | Diagnostic imaging interpretation; high demand. |
| Urology | $460,000 - $540,000 | Mix of clinical and surgical work. |
| Anesthesiology | $450,000 - $520,000 | Crucial hospital-based role with high liability. |
| Dermatology | $440,000 - $500,000 | High patient demand, mix of medical and cosmetic procedures. |
#### Lower-Earning Specialties (Cognitive-Focused):
These are typically primary care and other non-procedural, "cognitive" specialties that form the bedrock of the healthcare system.
| Specialty | Average Annual Compensation | Notes |
| :--- | :--- | :--- |
| Emergency Medicine | $350,000 - $410,000 | Shift work, high-stress environment. |
| Internal Medicine (General) | $260,000 - $290,000 | Primary care for adults. |
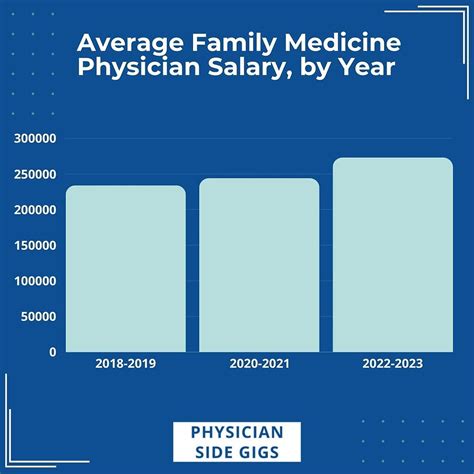
| Family Medicine | $250,000 - $280,000 | Cares for patients of all ages; broad scope of practice. |
| Pediatrics (General) | $240,000 - $270,000 | Primary care for children; generally has the lowest reimbursement rates. |
| Preventive Medicine | $230,000 - $260,000 | Focus on public health and population wellness. |
The Power of Sub-Specialization (Fellowships): Within a single specialty, pursuing a fellowship (1-3+ additional years of training) can dramatically impact income. A general cardiologist might earn around $450,000. But an *interventional cardiologist* who completes a fellowship to perform complex procedures can easily earn over $650,000. Similarly, within orthopedic surgery, a sub-specialist in spine surgery will typically out-earn a general orthopedist.
### 2. Geographic Location
Where you choose to practice has a profound impact on your salary. This often works in a counter-intuitive way: areas with the highest cost of living (e.g., New York City, San Francisco) do *not* always have the highest physician salaries. This is due to high physician saturation and dominant academic medical centers, which tend to pay less than private groups.
Conversely, less "desirable" or more rural areas often have to offer higher salaries and better incentives to attract and retain physicians.
- According to the U.S. Bureau of Labor Statistics (BLS) May 2022 data for Physicians and Surgeons, All Other, the top-paying states include:
1. Montana: Average Annual Mean Wage: $341,960
2. South Dakota: $323,230
3. Wyoming: $312,850
4. Indiana: $311,960
5. Wisconsin: $299,610
- States that tend to be on the lower end of the compensation spectrum often include those in the Northeast, like Maryland, Massachusetts, and New Jersey, along with areas with a high density of physicians.
- The Rural vs. Urban Divide: A family physician in rural Nebraska might be offered a starting salary of $300,000 with a $50,000 signing bonus and loan repayment, while a classmate taking a job in Boston might start at $220,000. The rural practice is competing for talent, while the urban one has a surplus of applicants. When considering location, you must weigh the higher salary against lifestyle preferences, cultural amenities, and opportunities for your spouse and family.
### 3. Practice Setting and Ownership Model
The type of organization you work for is another critical variable. Each model has distinct trade-offs between autonomy, administrative burden, and compensation structure.
- Physician-Owned Private Practice (Solo or Group): This model offers the highest income potential. After a 2-3 year partnership track, physicians become owners and share in the practice's profits. This comes with the highest autonomy but also the responsibility of running a business—managing staff, billing, and overhead. An orthopedic surgeon in a private group can easily earn over $1 million annually as a senior partner.
- Hospital or Health System-Employed: This is now the most common employment model. Physicians are employees of the hospital. This model offers greater stability, predictable hours, and freedom from administrative burdens. Compensation is typically a base salary plus productivity bonuses. While the ceiling is lower than private practice ownership, the floor is higher and more secure.
- Academic Medical Center: Working for a university hospital involves a three-part mission: clinical care, teaching, and research. Compensation is almost always lower than in private or hospital-employed settings. The trade-off is the prestige, intellectual stimulation, opportunities for cutting-edge research, and teaching the next generation of doctors. An academic cardiologist might earn $350,000, while their private practice counterpart earns $600,000.
- Government/Federal: Physicians working for organizations like the Department of Veterans Affairs (VA) or the Indian Health Service (IHS). Pay is typically lower and determined by federal pay scales. However, these roles come with outstanding federal benefits, loan forgiveness programs (like Public Service Loan Forgiveness - PSLF), and often a better work-life balance with less pressure on productivity.
### 4. Years of Experience and Reputation
As detailed in the previous section, salary grows with experience. This is not just about automatic annual raises. It's about a confluence of factors:
- Clinical Efficiency: An experienced physician can see more patients and perform procedures more efficiently, directly boosting productivity-based income.
- Building a Patient Panel: Over time, a physician builds a large and loyal base of patients, ensuring a full schedule.
- Reputation: A strong reputation leads to more referrals from other doctors, further driving volume.
- Partnership: As mentioned, achieving partner status in a private group is the single largest jump in mid-career income.
### 5. In-Demand Skills and Procedural Abilities
In medicine, "skills" directly translate to procedural capabilities and niche expertise. A physician's value is enhanced by their ability to perform specific, high-demand, and well-reimbursed services.
- Advanced Procedural Skills: In almost every specialty, there are advanced techniques that command higher pay. Examples include robotic surgery for urologists and general surgeons, complex ablation techniques for electrophysiologists, or performing Transcatheter Aortic Valve Replacement (TAVR) for interventional cardiologists.
- Leadership and Administrative Roles: Physicians who take on leadership roles—such as a Medical Director, Department Chair, or Chief Medical Officer (CMO)—receive an administrative stipend