Table of Contents

- [Introduction](#introduction)
- [What Does a Neonatologist Do?](#what-does-a-neonatologist-do)
- [Average Neonatologist Salary: A Deep Dive](#average-neonatologist-salary-a-deep-dive)
- [Key Factors That Influence a Neonatologist's Salary](#key-factors-that-influence-a-neonatologists-salary)
- [Job Outlook and Career Growth for Neonatologists](#job-outlook-and-career-growth-for-neonatologists)
- [How to Become a Neonatologist: Your Step-by-Step Guide](#how-to-become-a-neonatologist-your-step-by-step-guide)
- [Conclusion: Is a Career in Neonatology Right for You?](#conclusion-is-a-career-in-neonatology-right-for-you)
Introduction

Embarking on a career in medicine is a monumental decision, often driven by a deep-seated desire to heal and make a profound difference. For those drawn to the most fragile and vulnerable of patients, the field of neonatology represents one of the most challenging and rewarding paths available. A neonatologist is a highly specialized pediatrician who provides medical care to newborn infants, especially those who are born premature, critically ill, or with a birth defect. It's a career that operates at the very frontier of life, demanding extraordinary skill, unwavering compassion, and profound resilience.
Beyond the immense personal fulfillment, a career in neonatology also offers significant financial stability and a strong professional outlook. The answer to the query "what is a neonatologist salary?" reveals a compensation package that reflects the years of intensive training and the critical nature of the work. On average, a neonatologist in the United States can expect to earn a salary ranging from $250,000 to well over $400,000 annually, with top earners in high-demand areas or private practice exceeding this figure.
As a career analyst, I once had the privilege of interviewing a NICU (Neonatal Intensive Care Unit) director who described her role not as just a physician, but as a "guardian of possibilities." She spoke of the quiet moments at 3 a.m., adjusting a ventilator for a baby weighing less than a pound, and the overwhelming joy of seeing that same child go home with their parents months later. It is this unique intersection of cutting-edge science, intense human drama, and life-affirming outcomes that defines the world of a neonatologist.
This comprehensive guide will serve as your definitive resource, exploring every facet of a neonatologist's career. We will delve deep into salary benchmarks, dissect the factors that influence earnings, analyze the long-term job outlook, and provide a clear, step-by-step roadmap for those aspiring to enter this exceptional field. Whether you are a student mapping out your future or a medical professional considering a subspecialty, this article will provide the authoritative, data-driven insights you need to make an informed decision.
What Does a Neonatologist Do?

A neonatologist is far more than a "baby doctor." They are the intensive care specialists for the newborn population, possessing an expert understanding of the complex medical issues that can affect infants in the first few weeks and months of life. Their work is primarily based in the Neonatal Intensive Care Unit (NICU), a specialized ward equipped with advanced technology to support critically ill newborns.
The core responsibility of a neonatologist is to diagnose and treat medical conditions in newborns. These patients are often born prematurely, with low birth weights, or with complications such as congenital disorders (birth defects), infections, or breathing difficulties like respiratory distress syndrome. The neonatologist acts as the primary physician for these fragile infants, leading a multidisciplinary team of healthcare professionals.
Key Roles and Responsibilities:
- Diagnosis and Treatment: Identifying and managing a wide range of neonatal conditions, from jaundice and feeding problems to life-threatening heart defects and sepsis.
- Medical Procedures: Performing highly specialized procedures such as intubation (placing a breathing tube), inserting central venous and arterial lines for medication and monitoring, and managing advanced life support systems like ventilators and incubators.
- Team Leadership: Directing and collaborating with a team that includes neonatal nurses, respiratory therapists, pediatric surgeons, nutritionists, social workers, and other specialists to create and execute a comprehensive care plan for each infant.
- Prenatal Consultation: Consulting with obstetricians and expectant parents when a high-risk birth is anticipated. This involves counseling families about potential outcomes and preparing a plan for the infant's immediate care after delivery.
- Family Communication and Support: This is a cornerstone of the role. Neonatologists must compassionately and clearly communicate complex medical information, progress updates, and difficult prognoses to anxious and emotionally distressed parents.
- Research and Education: Many neonatologists, particularly those in academic medical centers, are involved in clinical research to advance the field and in teaching medical students, residents, and fellows.
### A Day in the Life of a Neonatologist
To make the role more tangible, consider a typical (though no day is truly "typical") day for a neonatologist in a busy hospital NICU:
- 7:00 AM: Arrive at the hospital, receive a detailed "sign-out" from the on-call physician about events that occurred overnight. Review patient charts, lab results, and imaging studies for the day's caseload.
- 8:00 AM - 11:00 AM: Conduct morning rounds with the full NICU team. This involves going bed-to-bed, discussing each infant's status, assessing their progress, and making adjustments to the treatment plan. This is a highly collaborative process involving nurses, therapists, and pharmacists.
- 11:00 AM - 1:00 PM: Family meetings and procedures. This time might be spent meeting with parents to provide a detailed update or discuss a change in their baby's condition. It could also involve performing a necessary procedure, like placing an umbilical line or performing a lumbar puncture.
- 1:00 PM - 2:00 PM: Attend a high-risk delivery in the labor and delivery unit. The neonatologist leads the resuscitation team, ready to provide immediate, life-sustaining care the moment the baby is born.
- 2:00 PM - 4:00 PM: Administrative tasks, charting, and consultations. This includes meticulously documenting all patient encounters, ordering tests, and consulting with other specialists like pediatric cardiologists or geneticists.
- 4:00 PM - 5:00 PM: Evening rounds and sign-out. Conduct a final check on the most critical patients and provide a thorough handover to the incoming evening or on-call neonatologist, ensuring continuity of care.
- On-Call: The day may not end at 5:00 PM. Neonatologists work in shifts and take on-call duties, meaning they may need to return to the hospital or be available by phone overnight to manage emergencies.
This demanding schedule is balanced by the profound impact a neonatologist has, offering a fighting chance to infants who might not otherwise survive and guiding families through the most stressful and hopeful time of their lives.
Average Neonatologist Salary: A Deep Dive
The significant investment in education and training required to become a neonatologist is rewarded with a compensation package that places them among the higher-earning medical specialists. A neonatologist's salary is not a single, static number but rather a range influenced by a variety of factors, including total compensation structure.
According to the 2023 Medscape Physician Compensation Report, one of the most authoritative sources in the industry, pediatricians (the parent specialty of neonatology) have an average annual salary of approximately $251,000. However, subspecialists like neonatologists earn significantly more due to their additional fellowship training and the critical nature of their work.
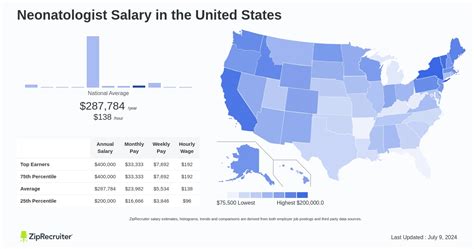
More specific data from leading salary aggregators provides a clearer picture of neonatologist earnings:
- Salary.com reports the median neonatologist salary in the United States as $283,293 as of late 2023, with a typical range falling between $242,912 and $339,715.
- Payscale.com indicates an average base salary of around $267,000 per year, with total pay packages reaching up to $350,000 or more when bonuses are included.
- Glassdoor data, which is based on user-submitted reports, shows an average salary of approximately $275,000 per year.
It's reasonable to conclude that the national average base salary for a neonatologist lies firmly in the $270,000 to $290,000 range, with the vast majority of practitioners earning somewhere between $240,000 and $350,000.
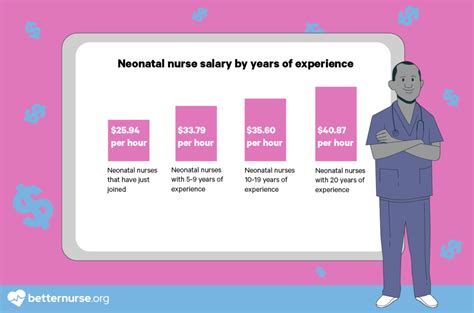
### Neonatologist Salary by Experience Level
Like most professions, compensation in neonatology grows significantly with experience. As physicians gain expertise, take on more responsibilities, and build a reputation for excellent outcomes, their earning potential increases.
| Experience Level | Typical Years of Practice | Average Annual Salary Range | Key Responsibilities |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-3 years | $220,000 - $265,000 | Primarily clinical duties, learning institutional protocols, building speed and efficiency. |
| Mid-Career | 4-10 years | $265,000 - $320,000 | Proficient in all clinical duties, may take on teaching roles, lead quality improvement projects, or mentor fellows. |
| Senior/Experienced| 10-20+ years | $320,000 - $400,000+ | Often holds leadership positions (e.g., NICU Medical Director), involved in high-level administrative strategy, research, or runs a private practice. |
*Source: Data synthesized from Salary.com, Medscape, and industry reports.*
### Beyond the Base Salary: Understanding Total Compensation
A neonatologist's income is more than just their annual salary. The total compensation package is a critical component of their overall earnings and can add significant value.
- Bonuses: This is a major component of physician pay.
- Signing Bonus: Often offered to attract new talent, especially in less desirable locations or high-demand markets. These can range from $10,000 to $50,000 or more.
- Performance/Productivity Bonus: Increasingly common, this bonus is tied to metrics such as patient volume (Relative Value Units or RVUs), quality of care outcomes, or patient satisfaction scores. This can add 10-20% to the base salary.
- Retention Bonus: Offered to valued physicians to encourage them to stay with a hospital or practice group.
- Profit Sharing: This is more common in private practice groups than in large hospital systems. Partners in a successful practice may share in the annual profits, which can substantially increase their total income.
- Retirement Benefits: Strong retirement plans are a standard part of the compensation package. This typically includes a 401(k) or 403(b) plan with a generous employer match.
- Insurance: Comprehensive benefits are essential.
- Health, Dental, and Vision Insurance: Provided for the physician and often their family at a subsidized rate.
- Malpractice Insurance: This is a crucial and expensive necessity. The employer almost always covers the full cost of malpractice insurance, a benefit worth tens of thousands of dollars per year.
- Disability and Life Insurance: Employer-paid or subsidized policies are standard to protect the physician's income in case of illness, injury, or death.
- Allowances and Perks:
- Continuing Medical Education (CME): An annual stipend (e.g., $3,000 - $5,000) and paid time off to attend conferences and stay current with medical advancements.
- Relocation Assistance: A significant financial package to cover the costs of moving for a new job.
- Professional Dues and Licensing Fees: Employers typically cover the costs of state medical licenses, DEA licenses, and dues for professional organizations like the American Academy of Pediatrics (AAP).
When evaluating a job offer, it is vital for a neonatologist to look beyond the base salary and consider the full value of this comprehensive compensation structure.
Key Factors That Influence a Neonatologist's Salary

The wide salary range for neonatologists—spanning over $150,000 from entry-level to senior roles—is driven by a complex interplay of factors. Understanding these variables is crucial for anyone looking to maximize their earning potential in this field. This section provides an exhaustive breakdown of the primary drivers of neonatologist compensation.
###
Level of Education and Certification
In medicine, the educational path is rigorous and standardized, but certifications provide the key differentiator. For a neonatologist, the journey is non-negotiable and directly tied to employment and salary.
- The Foundational Path: The baseline for any practicing neonatologist is a Doctor of Medicine (M.D.) or Doctor of Osteopathic Medicine (D.O.) degree, followed by a three-year residency in Pediatrics, and then a three-year fellowship in Neonatal-Perinatal Medicine. This extensive training—a minimum of 10 years after an undergraduate degree—is the price of entry.
- Board Certification: The Gold Standard: While completing the fellowship makes one eligible, achieving board certification is what truly unlocks top-tier salaries. This is a two-step process:
1. American Board of Pediatrics (ABP) Certification: First, a physician must pass the examination to become a board-certified pediatrician.
2. Neonatal-Perinatal Medicine Subspecialty Certification: After completing the fellowship, they must then pass a separate, highly rigorous subspecialty board exam.
- Impact on Salary: A physician who is "board eligible" (finished training but not yet certified) will earn less than one who is "board certified." Virtually all reputable hospitals and practice groups require board certification for partnership, leadership roles, and their highest salary brackets. Maintaining this certification through ongoing education and re-examination is also required and is a factor in sustained high earnings.
###
Years of Experience
Experience is arguably the most straightforward driver of salary growth in neonatology. The progression is not merely about time served; it's about the accumulation of expertise, efficiency, and leadership capabilities.
- Early Career (Years 0-3): An entry-level neonatologist is clinically competent but is still learning the specific systems of their employer, building relationships within the hospital, and refining their clinical judgment. Their salary is competitive but sits at the lower end of the spectrum, typically in the $220,000 - $265,000 range. They are focused on direct patient care and do not yet have significant administrative or teaching responsibilities.
- Mid-Career (Years 4-10): By this stage, the neonatologist is a seasoned clinician. They can handle the most complex cases with confidence and efficiency. This is often when they begin to take on additional roles that increase their value and, consequently, their salary. This may include serving on hospital committees, mentoring fellows, or leading quality improvement initiatives. Their salary moves into the $265,000 - $320,000 range.
- Senior/Leadership (Years 10+): With a decade or more of experience, a neonatologist is an expert in their field. Many transition into leadership roles, such as the Medical Director of the NICU. This position comes with significant administrative responsibilities, including managing budgets, overseeing staffing, setting clinical protocols, and representing the department at a hospital-wide level. These roles command the highest salaries, often pushing well into the $320,000 to $400,000+ bracket. Their reputation can also make them a key asset in a hospital's prestige and ability to attract patients.
###
Geographic Location
Where a neonatologist chooses to practice has a profound impact on their salary. This variation is driven by state and local economies, cost of living, and the regional supply and demand for medical subspecialists.
- High-Paying States and Regions: States with a high cost of living, large metropolitan areas, or a shortage of specialists often offer the highest salaries to attract talent. According to various data sources, states like California, Texas, Florida, and New York are often cited as having high demand and competitive salaries. Interestingly, some less populous states in the Midwest and South may also offer very high salaries to compensate for being in a less desirable or more rural location. A hospital in rural North Dakota might offer a salary competitive with one in Los Angeles to fill a critical need.
- Lower-Paying States and Regions: Conversely, areas with a lower cost of living or a high concentration of academic medical centers (which can sometimes suppress salaries due to a surplus of physicians willing to work for prestige) may have slightly lower average salaries. Some areas in the Northeast and parts of the Southeast fall into this category.
- Urban vs. Rural Divide: A significant salary differential often exists between urban and rural settings. While major cities have a high cost of living, they also have a higher concentration of physicians. Rural or underserved areas often struggle to recruit specialists and therefore offer lucrative financial packages, including higher base salaries and loan repayment assistance programs, to attract neonatologists.
Illustrative Salary Variation by Metropolitan Area (Median Salary):
| Metropolitan Area | Representative Median Salary | Commentary |
| :--- | :--- | :--- |
| San Francisco, CA | ~$325,000 | Very high cost of living drives up salaries. |
| Dallas, TX | ~$295,000 | Strong economy and high demand for specialists. |
| New York, NY | ~$310,000 | High cost of living and major academic centers. |
| Miami, FL | ~$280,000 | Growing population and demand for healthcare. |
| St. Louis, MO | ~$270,000 | Lower cost of living, but still competitive pay. |
*Source: Synthesized data from Salary.com's location-based salary calculator.*
###
Practice Setting (Type of Employer)
The type of organization a neonatologist works for is a critical determinant of both salary structure and overall career experience.
- Academic Medical Centers: These are university-affiliated hospitals.
- Salary: Often on the slightly lower end of the scale for purely clinical work. A portion of the neonatologist's time is "protected" for research, teaching medical students and residents, and other academic pursuits, which may not be compensated at the same rate as clinical productivity.
- Pros: Prestige, cutting-edge research opportunities, intellectually stimulating environment, strong benefits.
- Cons: Potentially lower pure-cash compensation, pressure to "publish or perish."
- Large Hospital Systems (Private or Non-Profit): This is the most common employment model.
- Salary: Highly competitive base salaries combined with robust productivity bonuses (RVU-based). These systems are focused on clinical efficiency and patient volume.
- Pros: High earning potential, stability, excellent benefits, access to extensive resources.
- Cons: Can be bureaucratic, less autonomy than private practice.
- Private Practice Groups: A group of neonatologists who contract their services to one or more hospitals.
- Salary: Highest income potential. After an initial period as an employee, a physician may be offered partnership. Partners share in the practice's profits, which can lead to incomes well in excess of $400,000 - $500,000 in a successful group.
- Pros: Maximum autonomy, direct financial reward for hard work.
- Cons: Involves business risk, responsibility for overhead and administration, less stability.
- *Locum Tenens* (Temporary Work): Working as an independent contractor to fill temporary vacancies.
- Salary: Very high daily or weekly rates (e.g., $1,500 - $2,500+ per day) to compensate for the lack of benefits and instability.
- Pros: Flexibility, high hourly pay, opportunity to travel and experience different practice settings.
- Cons: No job security, no benefits (have to buy own health and malpractice insurance), constant travel.
###
Area of Specialization or Niche Expertise
While neonatology is already a subspecialty, developing a further niche within the field can lead to leadership opportunities and higher compensation. This isn't a formal "specialization" but rather a recognized area of expert focus. Examples include:
- Neonatal Neurology: Expertise in managing brain injuries and neurological conditions in newborns.
- Neonatal Cardiology/Pulmonology: Deep knowledge in managing complex congenital heart and lung diseases.
- ECMO (Extracorporeal Membrane Oxygenation): Expertise in managing this advanced form of life support.
- Neonatal Nutrition: Focus on the complex dietary needs of premature and sick infants.
A neonatologist who becomes the go-to expert in one of these areas is more likely to be appointed as a program director or sought after by high-acuity NICUs, both of which correlate with higher pay.
###
In-Demand Skills (Clinical and Non-Clinical)
Beyond core clinical competence, certain skills dramatically increase a neonatologist's market value.
- Advanced Procedural Skills: Proficiency in the most complex and high-risk procedures makes a candidate more attractive to Level IV NICUs (the highest level).
- Leadership and Administrative Skills: The ability to manage budgets, lead teams, and develop clinical programs is the primary path to the highest-paying non-private practice jobs, such as NICU Medical Director or Chief of Pediatrics.
- Telemedicine and Informatics: As telehealth becomes more integrated into medicine, proficiency in virtual consultations and using electronic health records (EHR) efficiently is a valuable skill.
- Communication and Empathy: While a "soft skill," the ability to communicate effectively and compassionately with families is highly prized. Hospitals track patient satisfaction scores, and physicians who excel in this area are considered major assets.
Job Outlook and Career Growth for Neonatologists

For those investing over a decade in training, the long-term viability of their chosen career is a paramount concern. Fortunately, the job outlook for neonatologists is strong and stable, driven by persistent medical needs and evolving healthcare trends.
The U.S. Bureau of Labor Statistics (BLS) projects the employment of physicians and surgeons, in general, to grow by 3% from 2022 to 2032. While this is about the average for all occupations, the demand for specialists like neonatologists is expected to be more robust due to several key factors specific to the field.
Key Drivers of Demand for Neonatologists:
1. Advances in Medical Technology: The single greatest driver is the continued advancement in neonatal care. Technologies like advanced ventilators, surfactant therapy, and therapeutic hypothermia are allowing smaller and more premature infants to survive. These infants require prolonged, intensive care, directly fueling the need for neonatologists to manage their complex health issues.
2. Stable Prematurity Rates: Despite advances in prenatal care, the rate of premature births in the United States has remained relatively stable. According to the CDC, the preterm birth rate was 10.4% in 2022. This consistent patient population ensures a steady need for NICU services.
3. Increase in High-Risk Pregnancies: Trends such as delayed childbearing (older maternal age) and rising rates of maternal health conditions like obesity and diabetes contribute to a higher number of high-risk pregnancies, which in turn increases the likelihood of an infant requiring neonatal intensive care.
4. Aging Workforce and Retirement: A significant portion of the current neonatologist workforce is approaching retirement age. As these experienced physicians leave the field, it will create substantial job openings for newly trained fellows, ensuring a healthy job market for the next generation.
5. Regionalization of Care: There is a growing trend to centralize high-risk infant care in well-equipped, high-level (Level III and IV) NICUs. While this may concentrate jobs in certain urban or regional centers, it also increases the demand for highly skilled neonatologists to staff these advanced units.
### Emerging Trends and Future Challenges
The field of neonatology is not static. Aspiring and practicing physicians must be aware of the trends and challenges that will shape the profession in the coming years.
- The Rise of Tele-Neonatology: Telemedicine is making significant inroads into the NICU. This allows neonatologists at