Introduction

Have you ever wondered about the professionals who dedicate their lives to solving the complex puzzles of the human immune system? From the child who can finally enjoy a birthday party without fear of a peanut allergy, to the adult who can breathe freely during pollen season, Allergists and Immunologists are the unsung heroes behind millions of success stories. If you are driven by a passion for science, a desire for direct patient impact, and are seeking a career that is both intellectually stimulating and financially rewarding, the field of Allergy and Immunology might be your perfect calling.
This specialty offers a remarkable combination of high earning potential, a favorable work-life balance compared to many other medical fields, and the deep satisfaction of drastically improving patients' quality of life. The national average allergy and immunology salary often surpasses $300,000, with top earners in high-demand areas or successful private practices earning well over $500,000 annually. I personally witnessed the life-changing impact of this profession when a close family member, after years of debilitating chronic hives and mysterious allergic reactions, was finally diagnosed and treated by a brilliant immunologist. Seeing their journey from constant discomfort and anxiety to a life of normalcy and control was a powerful testament to the value these specialists provide.
This guide is designed to be your definitive resource, whether you are a high school student exploring future careers, a medical student choosing a specialty, or a resident weighing your fellowship options. We will dissect every component of an Allergist/Immunologist's career, from their daily responsibilities to the intricate factors that determine their ultimate earning potential.
### Table of Contents
- [What Does an Allergist/Immunologist Do?](#what-they-do)
- [Average Allergy and Immunology Salary: A Deep Dive](#salary-deep-dive)
- [Key Factors That Influence Salary](#key-factors)
- [Job Outlook and Career Growth](#job-outlook)
- [How to Become an Allergist/Immunologist](#how-to-start)
- [Conclusion: Is This Career Right for You?](#conclusion)
What Does an Allergist/Immunologist Do?

An Allergist/Immunologist is a highly specialized physician who is an expert in diagnosing, treating, and managing conditions related to the immune system. Their scope is far broader than just seasonal allergies and includes a vast array of complex disorders. They are, in essence, detectives of the body's defense system, investigating when it overreacts (allergies, asthma), underreacts (immunodeficiency), or mistakenly attacks itself (autoimmune aspects).
The profession blends the intellectual rigor of internal medicine or pediatrics with the hands-on, procedural aspects of a specialist. They treat patients of all ages, from infants with severe food allergies to elderly patients with complex medication reactions, making every day unique and challenging.
Core Responsibilities and Daily Tasks:
An Allergist's work is typically centered in an outpatient clinic setting, which contributes to the more predictable schedules and better work-life balance associated with the specialty. Their primary duties include:
- Patient Consultation: Conducting thorough patient histories, listening carefully to descriptions of symptoms, triggers, and environmental factors. This is the cornerstone of their diagnostic process.
- Diagnostic Testing: Performing and interpreting a range of tests to pinpoint the cause of symptoms. This includes:
- Skin Prick Testing: Applying tiny amounts of common allergens to the skin to check for a reaction.
- Intradermal Testing: Injecting a small amount of allergen under the skin for more sensitive testing.
- Patch Testing: Applying patches with allergens to the skin to diagnose contact dermatitis.
- Blood Tests (e.g., IgE tests): Measuring the level of specific antibodies to allergens in the blood.
- Pulmonary Function Tests (Spirometry): Assessing lung function in patients with suspected asthma.
- Treatment and Management: Developing personalized treatment plans that may include:
- Pharmacotherapy: Prescribing medications like antihistamines, nasal corticosteroids, emergency epinephrine, and advanced biologic drugs for severe asthma or atopic dermatitis.
- Allergen Immunotherapy: Administering allergy shots or sublingual (under-the-tongue) tablets to desensitize the immune system to specific allergens over time.
- Oral Immunotherapy (OIT): A cutting-edge treatment for food allergies where patients consume gradually increasing amounts of an allergen under strict medical supervision.
- Patient Education: Teaching patients and their families how to avoid triggers, manage their conditions, and use medications correctly.
- Administrative Duties: Charting patient visits in Electronic Health Records (EHRs), communicating with referring physicians, handling insurance pre-authorizations, and managing clinic operations.
### A Day in the Life of an Allergist/Immunologist
To make this tangible, let's follow a day in the life of a fictional allergist, Dr. Anya Sharma, who works in a private group practice.
- 8:00 AM - 9:00 AM: Dr. Sharma arrives at the clinic, reviews her patient schedule for the day, and checks lab results and messages that came in overnight. She quickly huddles with her nursing staff to discuss the day's more complex cases, including a new patient with suspected immunodeficiency and a child starting oral immunotherapy for a peanut allergy.
- 9:00 AM - 12:00 PM: The first block of patients begins. She sees a mix of cases: a follow-up visit for a teenager whose asthma is now well-controlled with a new biologic medication, a new consultation for an adult with chronic sinus infections, and a series of patients receiving their weekly allergy shots from the nursing team, whom she briefly checks in on.
- 12:00 PM - 1:00 PM: Lunch break. Dr. Sharma uses this time to catch up on charting, return calls to other physicians, and review a new study on atopic dermatitis published in the *Journal of Allergy and Clinical Immunology*.
- 1:00 PM - 4:30 PM: The afternoon patient block. This includes a long appointment for a patient with a complex drug allergy history, performing skin prick testing on a young professional with environmental allergies, and counseling the parents of a toddler newly diagnosed with a milk allergy.
- 4:30 PM - 5:30 PM: After the last patient leaves, Dr. Sharma completes all her patient notes for the day, signs off on prescription refills, and prepares for the next day. Once a week, this time is used for a practice management meeting with the other partners to discuss finances, staffing, and marketing.
This structured, patient-focused day is typical for the specialty and is a major draw for physicians seeking a sustainable and rewarding long-term career.
Average Allergy and Immunology Salary: A Deep Dive
The financial compensation for Allergists and Immunologists is a significant incentive for many who undertake the long educational journey. The salary is consistently ranked in the upper-middle tier of physician specialties, offering a lucrative income without the extreme hours or high-stress, life-or-death pressures of fields like neurosurgery or cardiothoracic surgery.
It's important to understand that "salary" is a comprehensive package. It includes a base salary, but is often supplemented by productivity bonuses, benefits, and, for practice owners, a share of the profits.
National Averages and Salary Ranges
Different salary aggregators and industry reports use various methodologies, so it's wise to look at several sources to get a complete picture. As of 2023-2024, here's how the numbers break down:
- Medscape's 2023 Physician Compensation Report, a highly respected industry benchmark, places the average annual compensation for Allergists & Immunologists at $299,000. This report surveys thousands of physicians across the United States.
- Salary.com, which aggregates real-time HR-reported data, shows a slightly higher median salary for an Allergist/Immunologist in the United States at $311,749 as of early 2024. Their typical range falls between $269,637 and $376,571.
- Doximity's 2023 Physician Compensation Report, another key industry source, reports an average compensation of $329,463 for the specialty.
- The U.S. Bureau of Labor Statistics (BLS) groups allergists under the broad category of "Physicians and Surgeons, All Other," which has a median annual wage of $253,990. However, this category is very broad and includes many lower-paying non-surgical specialties, so specialty-specific reports like Medscape and Doximity are more accurate for this field.
Taking these sources together, a realistic national average salary for a practicing Allergist/Immunologist is in the $300,000 to $330,000 range.
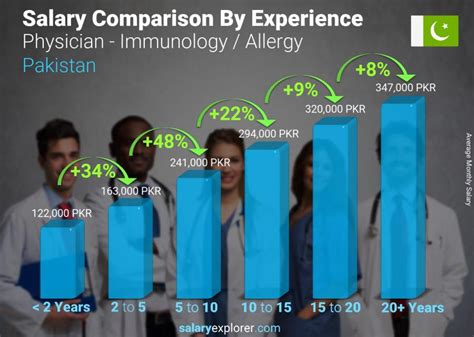
Salary Progression by Experience Level
Like any profession, compensation grows significantly with experience, skill, and reputation. Here is a typical trajectory:
| Career Stage | Years of Experience | Typical Annual Salary Range | Notes |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-2 Years | $220,000 - $275,000 | A physician who has just completed their fellowship. Salary is often a guaranteed base with smaller productivity bonuses as they build a patient panel. |
| Mid-Career | 3-10 Years | $280,000 - $350,000 | An established physician with a full patient load. Compensation is often heavily tied to productivity (RVUs). May have the opportunity for partnership in a private practice. |
| Senior/Experienced| 10+ Years | $350,000 - $500,000+ | A highly experienced physician, often a partner in a successful private practice or a senior physician in a large hospital network. May hold leadership or administrative roles. Top earners can exceed this range. |
*Source: Data synthesized from Salary.com, Medscape, and industry observations.*
Deconstructing the Compensation Package
An allergist's total earnings are more than just their paycheck. A comprehensive compensation package often includes:
- Base Salary: The guaranteed annual income. In hospital or academic settings, this is the bulk of the compensation. In private practice, it might be a lower number with a significant portion of income coming from bonuses.
- Productivity Bonuses (RVU-Based): Many employers, especially large group practices and hospitals, use a model based on Relative Value Units (RVUs). An RVU is a measure of value used by Medicare that factors in the time, skill, and intensity required for a patient service. Physicians are often paid a certain dollar amount per RVU they generate above a certain threshold. This directly rewards harder work and efficiency.
- Profit Sharing / Partnership Track: In private practices, a major financial goal is becoming a partner. After a few years as an employee, a physician may be offered the chance to "buy in" to the practice. As a partner, they receive a share of the practice's total profits in addition to their clinical salary, which can significantly increase total compensation.
- Benefits and Perks: These are non-salary benefits that have significant monetary value:
- Health, Dental, and Vision Insurance: Comprehensive family plans are standard.
- Malpractice Insurance: Typically covered by the employer, a significant expense that can cost $5,000-$15,000+ per year.
- Retirement Accounts: Generous 401(k) or 403(b) plans with employer matching contributions.
- Continuing Medical Education (CME) Allowance: An annual stipend (e.g., $2,000 - $5,000) to cover costs for conferences and courses needed to maintain medical licensure.
- Paid Time Off (PTO): Typically 4-6 weeks of vacation and sick leave.
- Relocation Allowance / Signing Bonus: Often offered to new physicians to attract them to a practice, which can be $10,000 to $30,000 or more.
When evaluating a job offer, it's crucial to look at this entire package, not just the base salary, to understand the true value of the position.
Key Factors That Influence Allergy and Immunology Salary

While the national averages provide a solid baseline, an individual allergist's salary can vary dramatically based on a confluence of factors. Understanding these levers is key to maximizing your earning potential throughout your career. This section will provide an exhaustive breakdown of the most influential variables.
###
Geographic Location: Where You Practice Matters Most
Geography is arguably the single most powerful determinant of a physician's salary. This is driven by supply and demand, local cost of living, and the reimbursement rates set by local insurance carriers and Medicare. The differences can be staggering, with salaries in some states being 20-30% higher than in others for the exact same work.
Top-Paying States and Regions:
Historically, states in the Southeast and Midwest tend to offer higher compensation for specialists. This is often because there is a higher demand and a lower supply of physicians compared to the more saturated coastal markets. These areas may also have a lower cost of living, making a high salary go even further.
According to various reports, including Doximity and Medscape, states consistently ranking high for physician compensation include:
- Kentucky
- Tennessee
- Alabama
- Florida
- Oklahoma
- Indiana
For instance, an allergist in a mid-sized city in Kentucky might earn $350,000, while their counterpart with the same experience in a major coastal city might earn $280,000.
Lower-Paying States and Regions:
Conversely, states in the Northeast and on the West Coast often have lower average salaries for physicians. This is a classic supply-and-demand issue. These regions have a high concentration of academic medical centers and are often seen as highly desirable places to live, leading to an oversupply of specialists willing to accept lower pay for the location.
States that tend to be on the lower end of the compensation spectrum include:
- Maryland
- Massachusetts
- New York
- California
It's a trade-off: a lower salary in Boston or San Francisco might be balanced by cultural amenities and proximity to prestigious institutions, but from a purely financial perspective, the Midwest and Southeast often offer a greater return.
Metropolitan vs. Rural Areas:
Within a state, salaries also differ between urban and rural settings. Rural and underserved areas often have to offer higher salaries and significant loan repayment incentives to attract physicians. An allergist willing to work in a smaller community an hour or two outside a major metropolitan area may find their compensation package is significantly higher than one in the heart of the city.
###
Practice Setting: Who You Work For
The type of organization an allergist works for has a profound impact on their salary structure, autonomy, and work-life balance.
- Private Practice (Physician-Owned): This setting traditionally offers the highest earning potential.
- Solo Practice: A single physician owns the entire practice. The potential for reward is unlimited, but so is the risk and administrative burden. Every aspect of the business, from billing to HR, falls on the owner.
- Single-Specialty Group: A group of allergists band together. This is a very common and lucrative model. It allows for shared overhead costs, better call schedules, and collective bargaining power with insurers. After becoming a partner, physicians share in the practice's profits. This is where salaries often climb into the $400,000 - $500,000+ range.
- Multi-Specialty Group: A large group of physicians from different specialties (e.g., primary care, ENT, dermatology, allergy) work together. This model provides a built-in referral base, which can be very stable and financially rewarding.
- Hospital or Health System Employment: This is an increasingly common model. The allergist is a direct employee of a hospital or a large healthcare network.
- Pros: Highly stable, predictable salary. The hospital handles all administrative and business aspects (billing, staffing, marketing). Excellent benefits packages and no personal financial risk.
- Cons: Lower ceiling on earning potential. Salaries are typically based on a set scale or RVU model with less upside than practice ownership. Less autonomy over practice decisions, scheduling, and staffing. The average salary in this setting often aligns with the national medians, around $280,000 - $350,000.
- Academic Medical Center: Working for a university-affiliated hospital. This path involves a three-part mission: clinical care, teaching, and research.
- Pros: Intellectually stimulating environment, opportunities to teach medical students and residents, ability to conduct cutting-edge research, and treating the most complex and rare cases.
- Cons: This is almost always the lowest-paid setting. A significant portion of time is dedicated to non-revenue-generating activities like teaching and research. Salaries are often 15-25% lower than in private practice, potentially in the $220,000 - $280,000 range. The trade-off is prestige and the unique opportunities of an academic career.
- Government/VA: Working for the Department of Veterans Affairs (VA) or other government entities.
- Pros: Exceptional job security, excellent federal benefits (including a pension), and a potentially lower-stress environment with a manageable patient load.
- Cons: Compensation is generally lower than in the private sector and is set by government pay scales. There can be more bureaucracy and less flexibility.
###
Years of Experience and Reputation
As detailed in the salary progression table, experience is a linear driver of income. However, it's not just about time served; it's about building a reputation.
- Early Career (Years 0-5): The focus is on building a patient base. Your schedule is filled by the practice, and you are proving your clinical skills and efficiency.
- Mid-Career (Years 5-15): You have a full and stable patient panel. Your reputation is established, and you receive consistent referrals from primary care physicians in the community who trust your work. This is when productivity-based bonuses become highly lucrative. If in private practice, this is the prime window for making partner.
- Late Career (Years 15+): You are a recognized expert. You may take on leadership roles within your practice or hospital, serve on committees for national organizations like the AAAAI or ACAAI, or reduce clinical hours to focus on administration. As a senior partner in a thriving practice, this is the period of peak earnings.
###
Board Certification and Subspecialization
For an Allergist/Immunologist, the educational path is fixed: medical school, a 3-year residency in Internal Medicine or Pediatrics, and a 2-year fellowship in Allergy & Immunology.
- Board Certification: After fellowship, passing the certification exam administered by the American Board of Allergy and Immunology (ABAI) is essential. While you can practice without it, being "Board Certified" is the gold standard. It is required by virtually all hospitals and insurance networks for credentialing. Lacking board certification would severely limit job opportunities and earning potential. Maintaining certification through continuous learning and periodic exams is also required.
- Subspecialization: While Allergy & Immunology is itself a specialty, some physicians develop a niche *clinical focus* that can enhance their reputation and draw complex referrals, indirectly boosting income. Examples include:
- Severe Asthma Centers: Becoming an expert in the use of new, expensive biologic therapies.
- Food Allergy Institutes: Specializing in oral immunotherapy (OIT), a complex and time-intensive service.
- Complex Immunodeficiency: Focusing on rare genetic disorders of the immune system, often in an academic setting.
###
In-Demand Skills and Procedural Proficiency
Beyond foundational knowledge, certain high-value skills and procedures can translate directly to higher productivity and income.
- Proficiency with Biologics: The treatment landscape for severe asthma, atopic dermatitis (eczema), and chronic hives has been revolutionized by biologic medications. Physicians who are experts in prescribing and managing these complex and expensive therapies are highly sought after.
- Oral Immunotherapy (OIT): As mentioned, OIT for food allergies is a specialized service that not all allergists offer. It requires specific protocols and a high level of patient monitoring. Practices that successfully implement OIT programs can open up a significant new revenue stream.
- Business Acumen: For those in private practice, understanding the business of medicine is paramount. Skills in financial management, billing and coding optimization, staff management, and marketing can directly increase a practice's profitability and, therefore, a partner's take-home pay.
- Efficiency with Electronic Health Records (EHRs): In a volume-based world, the ability to see patients and complete documentation efficiently is crucial. A physician who can navigate their EHR system quickly can see more patients or finish their day earlier, directly impacting their RVU generation and work-life balance.
Job Outlook and Career Growth

For those investing the better part of a decade in training, the long-term career outlook is a critical consideration. The future for Allergists and Immunologists is exceptionally bright, driven by powerful environmental and public health trends.
Projected Job Growth
The U.S. Bureau of Labor Statistics (BLS) projects that employment for all physicians and surgeons will grow by 3% from 2022 to 2032, which is about as fast as the average for all occupations. While the BLS doesn't provide a specific growth rate for allergists, the underlying factors suggest that demand for this specialty will likely outpace the average. The Association of American Medical Colleges (AAMC) consistently projects a significant overall physician shortage in the coming years, particularly in specialties.
Why is the Demand for Allergists So Strong?
Several key trends are fueling the need for more allergy and immunology specialists:
1. The "Hygiene Hypothesis" and Rising Allergy Rates: There is a growing prevalence of allergic diseases worldwide, including food allergies, asthma, and environmental allergies. One theory is that modern, cleaner lifestyles have left our immune systems "bored" and more prone to overreacting to harmless substances. More allergies mean more patients in need of specialized care.
2. Increased Public Awareness: Awareness of the seriousness of food allergies and asthma is at an all-time high. Schools, restaurants, and the public are more educated, leading more people to seek formal diagnosis and treatment rather than just "living with it."
3. Climate Change: Longer and more intense pollen seasons due to climate change are worsening symptoms for millions of people with hay fever and allergic asthma, driving them to seek specialist care.
4. Advancements in Treatment: The explosion of new and effective treatments, especially biologic drugs and OIT, means that allergists can now offer real hope for conditions that were once poorly managed. This transforms the field from one of mere symptom control to one of disease modification, making it a more attractive and impactful specialty.
5. An Aging Population: As people age, their immune systems can change, leading to new allergies or complex drug reactions that require an allergist's expertise.
Future Challenges and Staying Relevant
Despite the positive outlook, the profession is not without its challenges. To thrive, allergists must be prepared to adapt.
- Administrative Burden: The time spent on EHR documentation and battling with insurance companies for pre-authorizations is a major source of physician burnout across all specialties.
- Reimbursement Pressures: Medicare and private insurance companies are constantly seeking to control costs, which can lead to stagnant or declining reimbursement rates for certain services.
- Competition from Other Providers: Otolaryngologists (ENTs), pulmonologists, and even primary care providers may manage less complex allergic conditions. The key for allergists is to position themselves as the definitive experts for moderate-to-severe and complex cases.
How to Future-Proof Your Career:
- Embrace Lifelong Learning: The field of immunology is one of the fastest-moving areas of medicine. Staying current on new research and treatments through CME is not just a requirement—it's a career-long necessity.
- Adopt New Technology: Integrating telehealth for follow-up visits, using patient portals effectively, and staying abreast of diagnostic innovations will be crucial for running an efficient and modern practice.
- Develop a Niche: As mentioned earlier, becoming the local "go-to" expert for a specific area like food allergy or severe asthma can create a strong, defensible referral base.
- Get Involved in Advocacy: Participating in professional organizations like the AAAAI and ACAAI allows physicians to have a voice in shaping healthcare policy, advocating for fair reimbursement, and defining the future of their specialty.
