Introduction

In the high-stakes, meticulously controlled environment of the operating room, a symphony of professionals works in concert to ensure a patient's safety and comfort. Among these critical players is the Anesthesia Physician Assistant (PA), a highly skilled clinician who stands at the nexus of vigilance, pharmacology, and patient care. If you are drawn to a career that combines intellectual rigor, procedural skill, and profound human impact—all while offering exceptional financial rewards—then the path of an Anesthesia PA deserves your full attention. With average salaries often soaring well into the six-figure range, frequently between $140,000 and $200,000+ per year, this specialization represents one of the most lucrative and respected domains for a Physician Assistant.
I once had the opportunity to shadow an anesthesia care team during a complex cardiac surgery. Amidst the beeps of monitors and the quiet intensity of the surgeons, the Anesthesia PA was a pillar of calm, making micro-adjustments to medications and monitoring vital signs with an unwavering focus that was nothing short of awe-inspiring. It was a powerful reminder that behind every successful surgery is a guardian of the patient's stability, and in many hospitals, that guardian is a PA. This guide is designed to be your comprehensive roadmap, taking you from a nascent interest to a deep, authoritative understanding of what it truly means—and what it truly pays—to be an Anesthesia PA. We will dissect salary data, explore influencing factors, and chart a course for you to enter this elite and rewarding field.
### Table of Contents
- [What Does an Anesthesia PA Do?](#what-does-an-anesthesia-pa-do)
- [Average Anesthesia PA Salary: A Deep Dive](#average-anesthesia-pa-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
What Does an Anesthesia PA Do?
An Anesthesia Physician Assistant, often working as part of an Anesthesia Care Team (ACT) under the supervision of an anesthesiologist, is a licensed medical professional responsible for providing anesthesia and related care to patients before, during, and after surgical, therapeutic, or diagnostic procedures. Their role is multifaceted and demands a deep understanding of physiology, pharmacology, and critical care principles.
It is crucial to distinguish an Anesthesia PA from a Certified Anesthesiologist Assistant (CAA). While their day-to-day clinical duties are often very similar, their educational paths differ. A PA attends a generalist PA program and then specializes in anesthesia through on-the-job training or a post-graduate fellowship. A CAA attends a master's program specifically and solely focused on anesthesiology from the start. Both are vital members of the ACT, but this guide focuses on the PA path to this specialization.
The core responsibilities of an Anesthesia PA can be broken down by the phase of care:
1. Pre-Operative Phase:
Before a patient ever enters the operating room, the Anesthesia PA performs a crucial assessment. This includes:
- Patient Evaluation: Reviewing the patient's medical history, lab results, and surgical plan.
- Physical Examination: Conducting a focused physical exam, particularly of the airway, cardiovascular, and respiratory systems.
- Anesthetic Plan Development: Collaborating with the supervising anesthesiologist to formulate a tailored anesthetic plan. This involves selecting the appropriate type of anesthesia (general, regional, local, or sedation) based on the patient's health status and the nature of the procedure.
- Patient Education and Consent: Explaining the anesthetic plan, its risks, and its benefits to the patient and their family, answering questions, and obtaining informed consent.
2. Intra-Operative Phase:
This is the heart of the Anesthesia PA's role, where vigilance is paramount. During the procedure, they are responsible for:
- Induction and Maintenance: Administering anesthetic agents, whether through IV injection or inhalation, to induce and maintain the desired level of anesthesia.
- Airway Management: Securing and managing the patient's airway, which may involve intubation (placing a breathing tube), using a laryngeal mask airway (LMA), or other advanced techniques.
- Physiological Monitoring: Continuously monitoring the patient's vital signs, including heart rate and rhythm (ECG), blood pressure, oxygen saturation, carbon dioxide levels (capnography), and body temperature.
- Fluid and Blood Management: Administering IV fluids, blood products, and medications to maintain hemodynamic stability and replace any blood loss.
- Problem Solving: Recognizing and rapidly responding to any adverse physiological changes or emergencies, such as an allergic reaction, change in heart rhythm, or blood pressure instability.
3. Post-Operative Phase:
The PA's care extends beyond the operating room into the Post-Anesthesia Care Unit (PACU).
- Emergence: Overseeing the patient's emergence from anesthesia, ensuring they wake up smoothly and comfortably.
- Pain Management: Assessing and managing post-operative pain with appropriate medications and techniques (e.g., nerve blocks).
- Nausea and Vomiting (PONV) Management: Treating and preventing one of the most common side effects of anesthesia.
- Handover and Discharge: Ensuring the patient is stable before transferring their care to the PACU nursing staff and providing a thorough report. For outpatient procedures, they clear the patient for discharge home when specific criteria are met.
### A Day in the Life of an Anesthesia PA
- 6:30 AM: Arrive at the hospital. Change into scrubs and review the day's surgical schedule. The first case is a knee replacement for a 68-year-old male with a history of hypertension.
- 7:00 AM: Meet the first patient in the pre-op holding area. Conduct a final check, confirm their medical history, perform an airway exam, explain the plan (a spinal anesthetic combined with light sedation), and place an IV line.
- 7:45 AM: Wheel the patient to the OR. Connect them to all standard monitors. With the anesthesiologist present, perform the spinal anesthetic. Once it has taken effect and the patient is comfortable and sedated, you confirm with the surgeon that they can begin.
- 8:00 AM - 9:30 AM: The surgery is underway. You monitor the patient's blood pressure, heart rate, and sedation level, making small adjustments to medications as needed. You chart everything meticulously in the electronic medical record.
- 9:30 AM: The surgery concludes. You transport the patient safely to the PACU, give a detailed report to the PACU nurse, and ensure the patient is comfortable before leaving.
- 9:45 AM: You quickly move to the next OR to help set up for a laparoscopic cholecystectomy (gallbladder removal). This will be a general anesthetic with intubation. You see the patient in pre-op and then proceed with the induction in the OR.
- 12:30 PM: Lunch break, if you're lucky. Often, it's a quick bite between cases.
- 1:00 PM - 4:00 PM: The afternoon might include a variety of cases: a pediatric patient for tonsillectomy, an orthopedic trauma case, or providing sedation for a colonoscopy in the endoscopy suite.
- 4:30 PM: Finish your last case. Complete all post-operative orders and charting. Check on the patients in the PACU to ensure they are recovering well.
- 5:00 PM: Handoff any remaining duties to the PA or anesthesiologist on call for the evening, and head home after a demanding but fulfilling day.
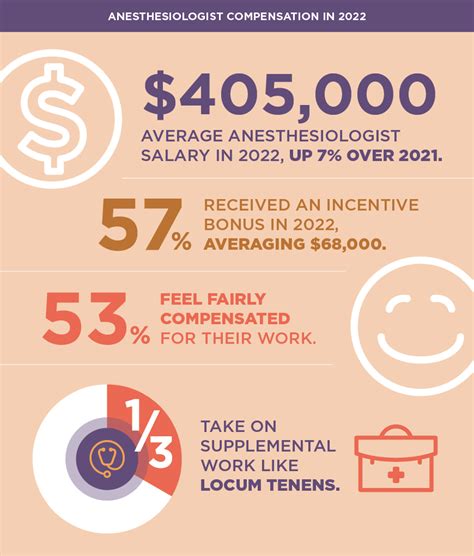
Average Anesthesia PA Salary: A Deep Dive
The specialization in anesthesia is one of the primary drivers of high earning potential within the Physician Assistant profession. The combination of advanced procedural skills, high-stakes decision-making, and the critical nature of the work places these professionals at the upper end of the PA salary spectrum.
First, it's essential to understand the baseline for all PAs. According to the U.S. Bureau of Labor Statistics (BLS), the median annual wage for Physician Assistants was $130,020 as of May 2023. The lowest 10 percent earned less than $87,030, and the highest 10 percent earned more than $176,140. Anesthesia PAs consistently fall into the upper portion of this range and often exceed it.
Specialty-specific data provides a much clearer picture. The 2023 American Academy of Physician Associates (AAPA) Salary Report is one of the most authoritative sources for this information. While it groups Anesthesiology with Critical Care and Emergency Medicine in some data sets, it provides clear indicators that these procedural, high-acuity specialties are the top earners.
Based on an analysis of data from the AAPA, Salary.com, Payscale, and real-world job postings, here is a comprehensive breakdown of what an Anesthesia PA can expect to earn.
National Average Anesthesia PA Salary:
- Median Base Salary: Approximately $155,000 - $175,000 per year.
- Typical Total Compensation Range (including bonuses, call pay, etc.): $165,000 - $210,000+ per year.
It's not uncommon for highly experienced Anesthesia PAs in high-demand locations or with significant overtime and call responsibilities to surpass $225,000 in total annual income.
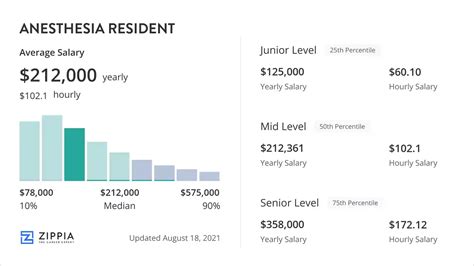
### Salary by Experience Level
Like any profession, compensation grows significantly with experience, autonomy, and skill refinement. Anesthesia requires a steep learning curve, and employers reward PAs who have mastered complex cases and can work with greater independence.
| Experience Level | Typical Years of Experience | Typical Base Salary Range | Typical Total Compensation Range | Key Attributes |
| :--- | :--- | :--- | :--- | :--- |
| Entry-Level / Fellow | 0-2 Years | $115,000 - $140,000 | $125,000 - $150,000 | Learning core procedures, closely supervised, may be in a fellowship program with a structured (and often lower) salary. |
| Mid-Career | 3-9 Years | $145,000 - $170,000 | $160,000 - $190,000 | Increased autonomy, manages a full slate of cases, proficient in common regional blocks, may begin precepting students. |
| Experienced / Senior | 10-19 Years | $165,000 - $190,000 | $185,000 - $220,000 | Manages the most complex cases (e.g., cardiac, trauma), proficient in advanced procedures, seen as a clinical leader. |
| Lead / Chief PA | 20+ Years or by role | $180,000 - $210,000+ | $200,000 - $250,000+ | Administrative duties, scheduling, team management, often still has clinical duties, top-tier clinical expert. |
*Sources: Data synthesized from the 2023 AAPA Salary Report, Payscale, Salary.com, and Glassdoor, adjusted for the Anesthesiology specialty.*
### Deconstructing the Compensation Package
The base salary is only one part of the equation. Anesthesia is a 24/7 field, and compensation structures are designed to reflect this. A comprehensive package for an Anesthesia PA often includes:
- Base Salary: The guaranteed annual pay for a standard workweek (e.g., 40 hours or four 10-hour shifts).
- Call Pay: This is a significant component. PAs are often required to be "on call" for nights, weekends, or holidays. This is typically compensated in two ways:
- Stipend: A flat fee simply for being available on call (e.g., $500 per weekend).
- Call-Back Pay: An hourly rate (often 1.5x the base hourly rate) for any time spent physically working in the hospital while on call.
- Overtime (OT): Pay for hours worked beyond the standard week. In a busy surgical service, OT can be a substantial income booster.
- Bonuses: These can come in several forms:
- Sign-On Bonus: Often offered to attract new talent, ranging from $5,000 to $25,000 or more, especially in underserved areas.
- Performance Bonus: Tied to departmental metrics, efficiency, or quality of care.
- Retention Bonus: Offered to tenured PAs to encourage them to stay.
- Profit Sharing: More common in private anesthesiology groups than in large hospital systems. PAs may be eligible for a share of the practice's profits after a certain number of years.
- Continuing Medical Education (CME) Allowance: A yearly stipend (typically $1,500 - $3,500) and paid time off to attend conferences and maintain certification.
- Retirement Benefits: Typically a 401(k) or 403(b) plan with an employer match. The quality of the match can vary significantly.
- Other Benefits: Comprehensive health, dental, and vision insurance; life and disability insurance; and coverage for licensure fees, DEA registration, and professional association dues.
When evaluating a job offer, it is absolutely essential to look at the total compensation package, not just the base salary. A job with a slightly lower base salary but generous call pay, a strong retirement match, and excellent benefits may be far more lucrative in the long run.
Key Factors That Influence Anesthesia PA Salary
An Anesthesia PA's salary isn't a single, fixed number; it's a dynamic figure shaped by a powerful combination of personal qualifications, market forces, and job-specific variables. Understanding these factors is the key to maximizing your earning potential throughout your career. This section provides an exhaustive breakdown of the elements that have the most significant impact on your paycheck.
###
Level of Education and Advanced Certification
While all practicing PAs must graduate from an accredited master's degree program, further education and certification in the specialty of anesthesia can provide a substantial salary advantage.
- Standard Master's Degree (MPAS, MHS, MSc): This is the mandatory entry point. Graduating from PA school and passing the PANCE (Physician Assistant National Certifying Examination) to earn your PA-C credential is the baseline. At this stage, your salary will be in the entry-level bracket.
- Post-Graduate Anesthesia Fellowship/Residency: This is a game-changer. These are 12-18 month intensive training programs offered by hospitals or academic centers. While you earn a stipend during the fellowship (often lower than a starting salary, e.g., $60,000 - $80,000), you graduate with a level of skill and confidence that is equivalent to several years of on-the-job training. Employers recognize this advanced training and are willing to pay a premium. A fellowship-trained PA can often bypass the typical "entry-level" salary and start directly in the mid-career range. It demonstrates a deep commitment to the specialty and proficiency in advanced techniques like regional anesthesia and critical care management right from day one.
- Certificate of Added Qualifications (CAQ) in Anesthesiology: The NCCPA offers the CAQ as a way for PAs to demonstrate their advanced knowledge and experience in a specialty. To earn the CAQ in Anesthesiology, a PA must meet requirements for experience (at least 3,000 hours in anesthesia), have a supervising anesthesiologist's attestation of their skills, and pass a specialty exam. Holding a CAQ is a formal credential that validates your expertise. While it may not always come with an automatic, contractual raise, it makes you a far more competitive candidate for higher-paying jobs and leadership positions. It signals to employers that you are a top-tier clinician, which translates to greater trust, more responsibility, and, consequently, higher compensation.
- Doctor of Medical Science (DMSc): While not specific to anesthesia, a DMSc degree can impact salary, particularly for those aspiring to leadership, administrative, or academic roles. A PA with a DMSc who becomes the Chief PA of an Anesthesiology department may be able to negotiate a higher salary based on their advanced education in healthcare leadership and administration.
###
Years of Experience
Experience is arguably the single most powerful driver of salary growth in this field. Anesthesia is a profession built on pattern recognition and muscle memory developed over thousands of cases.
- 0-2 Years (The Learning Phase): New graduates are a known quantity: they are intelligent and well-trained but lack real-world, high-pressure experience. Their first few years are an intense period of learning under close supervision. They learn the flow of the OR, master basic airway skills, and become comfortable with common anesthetic agents. Their salary reflects this training period.
- *Salary Impact:* You'll start at the bottom of the pay scale for the specialty but can expect annual raises of 3-5% as you gain competence.
- 3-9 Years (The Competent Professional): This is where significant salary growth occurs. By this point, the PA is autonomous in straightforward cases, proficient in a range of procedures (e.g., placing arterial lines, central lines, and some regional blocks), and can be trusted to manage their own OR. They are a reliable and efficient member of the team.
- *Salary Impact:* This is the period of the steepest salary increase. PAs often see their base salary increase by $30,000 to $50,000 or more from their starting point. Job-hopping after 3-5 years can often lead to a significant salary bump.
- 10+ Years (The Expert Clinician): With a decade or more of experience, the PA has seen almost everything. They are the go-to person for difficult airways, complex trauma cases, and sick patients. They are often proficient in advanced techniques like ultrasound-guided nerve blocks or managing cardiac and neurosurgical cases.
- *Salary Impact:* Earnings begin to plateau but at a very high level. Further significant increases are often tied to taking on new roles. Experienced PAs command top-tier salaries and are highly sought after. They can often negotiate for better call schedules, more CME funding, or other quality-of-life perks.
- 20+ Years (The Leader/Mentor): After two decades, many PAs transition into formal or informal leadership. They may become the Lead or Chief PA, responsible for scheduling, training new hires, and managing the team of PAs and CRNAs.
- *Salary Impact:* Moving into a leadership role comes with an administrative stipend or a higher base salary, pushing total compensation to the very top of the range, often exceeding $220,000 - $250,000.
###
Geographic Location
Where you practice has a monumental impact on your salary. This is influenced by a combination of local market demand, cost of living, and state-level scope of practice laws.
- High-Paying States and Regions: Generally, states with a high cost of living, large urban centers, and high demand for surgical services offer the highest salaries.
- Top Tier States: California, New York, Washington, Alaska, Connecticut, and Oregon often lead the pack. Anesthesia PAs in major metropolitan areas like New York City, Los Angeles, San Francisco, or Seattle can command base salaries well above $180,000.
- Rural and Underserved Areas: Paradoxically, some of the highest salaries can be found in less desirable or remote rural areas. Hospitals in these locations must offer significant financial incentives, including high salaries, large sign-on bonuses, and loan repayment programs, to attract qualified providers. A PA willing to work in rural Texas, North Dakota, or parts of the Midwest might find a total compensation package that rivals those in major cities.
- Lower-Paying States and Regions: States with a lower cost of living and a higher concentration of PA training programs or anesthesiology providers tend to have more saturated markets and lower salaries.
- Example Regions: The Southeast (e.g., Alabama, South Carolina) and some parts of the Midwest can have salaries that are 10-20% lower than the national average, although this is offset by a significantly lower cost of living.
- Urban vs. Suburban vs. Rural:
- Urban: Highest absolute salaries but also highest cost of living. Intense, high-volume work environment.
- Suburban: Often the "sweet spot." Salaries remain very competitive, often close to urban levels, but the cost of living (especially housing) can be substantially lower.
- Rural: Variable. Can be lower than average or extremely high if the facility is desperate to recruit. The lifestyle and scope of practice can be very different.
###
Practice Setting and Employer Type
The type of facility you work for dramatically shapes your compensation structure and overall earning potential.
- Large Academic Medical Center:
- *Salary:* Base salaries are often moderate to good but may not be the absolute highest.
- *Pros:* Excellent benefits, including robust retirement/pension plans, generous paid time off, and strong CME support. Exposure to cutting-edge procedures, complex cases, and teaching opportunities. Great for resume-building.
- *Cons:* Can be bureaucratic and less flexible. Salary growth may be tied to rigid institutional pay scales.
- Private Anesthesiology Group:
- *Salary:* This is where the highest income potential often lies.
- *Structure:* PAs typically start as employees. After a few years, they may be offered a path to partnership. As a partner, they receive a share of the group's profits in addition to their salary.
- *Pros:* Total compensation for partners can be extremely high, well over $250,000. More autonomy and a direct link between work ethic and financial reward.
- *Cons:* Benefits might be less comprehensive than at a large hospital. Less job security if the group loses its hospital contract. Call responsibilities can be very demanding.
- Community Hospital (Directly Employed):
- *Salary:* Highly variable, but often very competitive as they compete with private groups for talent.
- *Pros:* Often a good balance of interesting cases and work-life balance. Less bureaucracy than a major academic center. May offer excellent sign-on bonuses and retention packages.
- *Cons:* May lack the resources or case complexity of a university hospital.
- Outpatient Surgery Center (Ambulatory Surgical Center - ASC):
- *Salary:* Base salaries can be slightly lower than in a hospital setting.
- *Pros:* The major benefit is lifestyle. Typically no nights, no weekends, no holidays, and no call. This predictable schedule is highly attractive.
- *Cons:* Cases are generally healthier, "bread and butter" procedures. Less opportunity to use advanced critical care skills. Total compensation is almost always lower due to the lack of call and overtime pay.
###
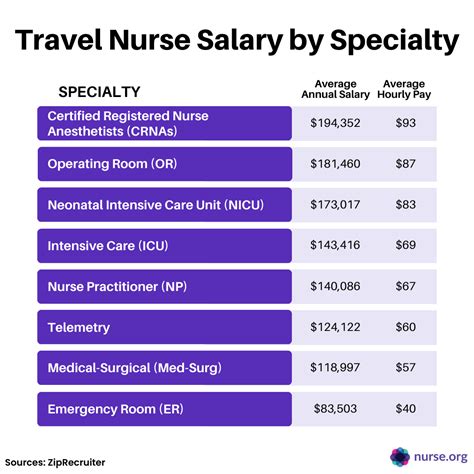
Area of Sub-Specialization
Just as PAs can specialize in anesthesia, they can further sub-specialize within the field. Mastering a high-acuity sub-specialty makes you a more valuable asset and a higher earner.
- Cardiac Anesthesia: This is often considered the pinnacle of the specialty. PAs assist in open-heart surgeries, valve replacements, and other complex cardiac procedures. It requires expertise in advanced monitoring (e.g., transesophageal echocardiography - TEE), and managing complex hemodynamics. This sub-specialty commands one of the highest salaries.
- Pediatric Anesthesia: Working with children, especially infants, requires a unique skill set and pharmacology knowledge. PAs specializing in pediatrics are highly sought after and well-compensated.
- Obstetric (OB) Anesthesia: Providing epidurals, spinals for C-sections, and managing laboring patients 24/7. This is a high-demand, high-stress field that often involves significant call pay.
- Pain Management: Some Anesthesia PAs work in pain clinics, performing interventional procedures like epidural steroid injections, joint injections, and nerve blocks. This can be a very lucrative, often outpatient-based career path.
- Critical Care (ICU): Some PAs split their time between the OR and the Surgical ICU. This dual skill set in anesthesiology and critical care makes them extremely valuable and can lead to higher pay.
###
In-Demand Skills
Beyond general competence, possessing specific, high-value procedural skills can directly translate to a higher salary or make you a more attractive candidate for top-paying jobs.
- Ultrasound-Guided Regional Anesthesia: Proficiency in performing nerve blocks (e.g., interscalene, femoral, popliteal) under ultrasound guidance is perhaps the single most valuable clinical skill for an Anesthesia PA today. It's crucial for modern, opioid-sparing pain management protocols. PAs who are experts in regional anesthesia are in high demand.
- Advanced Airway Techniques: Expertise with fiberoptic intubation, video laryngoscopy, and other difficult airway management tools.
- Point-of-Care Ultrasound (POCUS): Using ultrasound at the bedside for tasks like assessing cardiac function or guiding central line placement.
- Leadership and Administrative Skills: As mentioned, the ability to manage a team, create schedules, and handle departmental administration is a clear path to a higher salary via a Chief or Lead PA role.
- Efficiency and OR Turnover: In many settings, efficiency is king. A PA who can safely and efficiently