Introduction

Embarking on the path to becoming an anesthesiologist is a decision fueled by immense dedication, intellectual curiosity, and a profound desire to make a difference at the most critical moments in a patient's life. You have conquered the formidable challenges of undergraduate studies and the MCAT, navigated the rigors of medical school, and now stand at the threshold of residency—the intensive, hands-on training that will sculpt you into a skilled physician. But as the dream solidifies into a tangible career plan, a crucial practical question emerges: What is the reality of an anesthesiologist resident salary?
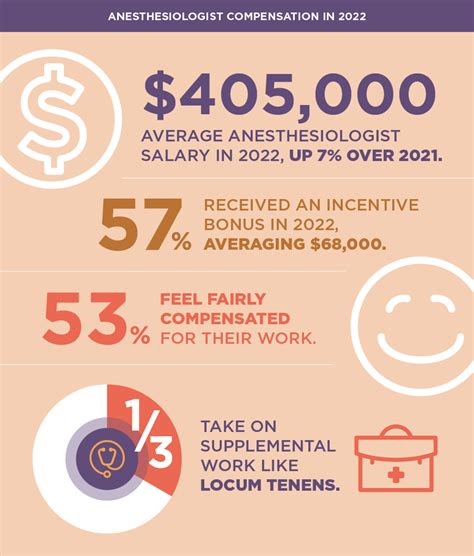
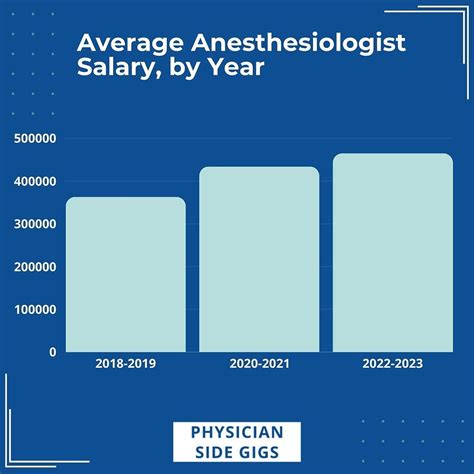
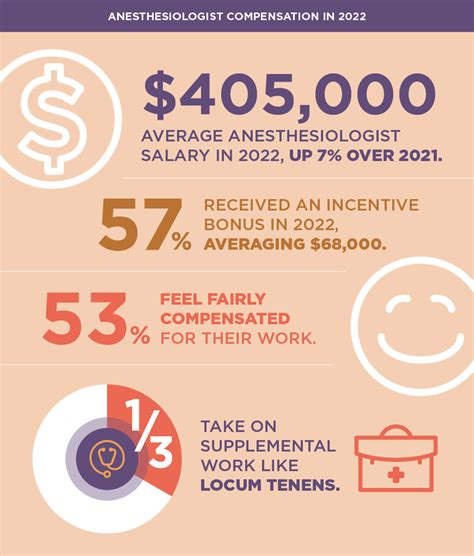
While the ultimate earning potential of an attending anesthesiologist is among the highest in medicine, with average salaries often exceeding $400,000 annually, the residency period is a different financial story. Anesthesiology residents, like all medical residents, earn a modest stipend that typically ranges from $60,000 to $85,000 per year, depending on the year of training and geographic location. This salary is not a reflection of the immense responsibility or the 80-hour workweeks, but rather a training wage funded primarily through a complex system of government and hospital financing.
I still vividly recall a conversation with a Chief Anesthesiology Resident during my time volunteering in a hospital. Amidst the controlled chaos of a pre-operative holding area, she spoke not of the long hours or the pay, but of the "sacred trust" of taking a patient safely through surgery and waking them up again. It's this profound purpose that grounds you through the financially lean years of training, a period of sacrifice that lays the foundation for an incredibly rewarding professional life.
This guide is designed to be your definitive resource on the financial realities and career landscape of anesthesiology residency. We will dissect every component of a resident’s compensation, explore the factors that dictate your pay, and map out the entire journey from medical student to attending physician.
### Table of Contents
- [What Does an Anesthesiologist Resident Do?](#what-does-an-anesthesiologist-resident-do)
- [Average Anesthesiologist Resident Salary: A Deep Dive](#average-anesthesiologist-resident-salary-a-deep-dive)
- [Key Factors That Influence an Anesthesiologist Resident's Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth for Anesthesiologists](#job-outlook-and-career-growth)
- [How to Become an Anesthesiologist](#how-to-get-started-in-this-career)
- [Conclusion: Is the Journey Worth the Reward?](#conclusion)
What Does an Anesthesiologist Resident Do?

An anesthesiology residency is a four-year postgraduate training program that a physician completes after graduating from medical school. The first year, known as the internship or PGY-1 (Post-Graduate Year 1), is typically a transitional or preliminary year in internal medicine, surgery, or a combination. The subsequent three years (PGY-2 through PGY-4) are dedicated to clinical anesthesiology (CA-1 through CA-3).
An anesthesiologist resident is, in essence, a physician in training, learning the art and science of anesthesiology under the direct supervision of attending physicians. Their role is far more than simply "putting patients to sleep." They are perioperative physicians, responsible for the safety and well-being of a patient before, during, and after a surgical procedure.
Core Responsibilities Include:
- Preoperative Evaluation: Meeting with patients before surgery to review their medical history, conduct a physical exam, discuss the anesthetic plan, and obtain informed consent. This involves assessing risk and optimizing the patient's condition for surgery.
- Anesthetic Plan Development: Creating a tailored anesthetic plan based on the patient's health status, the nature of the surgery, and the surgeon's requirements. This includes choosing the specific anesthetic agents, techniques (e.g., general, regional, local), and necessary monitoring equipment.
- Intraoperative Management: This is the heart of the role. The resident is responsible for inducing anesthesia, managing the patient's airway (often through intubation), and continuously monitoring vital signs (heart rate, blood pressure, oxygen saturation, temperature). They administer anesthetic gases, intravenous drugs, fluids, and blood products to maintain a stable state of anesthesia and physiological homeostasis throughout the entire procedure.
- Procedural Skills: Mastering critical, hands-on procedures such as endotracheal intubation, placing central venous lines, arterial lines for continuous blood pressure monitoring, and performing regional anesthesia techniques like epidurals, spinal blocks, and peripheral nerve blocks, often using ultrasound guidance.
- Postoperative Care: Managing the patient's immediate recovery from anesthesia in the Post-Anesthesia Care Unit (PACU). This includes managing pain, nausea, and any postoperative complications, and ensuring a safe transition to the hospital ward or discharge home.
- Pain Management: Participating in acute and chronic pain management services, consulting on patients with complex pain issues throughout the hospital.
- Emergency Response: Acting as a critical member of the hospital's emergency response teams, such as the "code blue" team (for cardiac arrest) and the rapid response team, due to their expertise in airway management and resuscitation.
- Didactics and Education: Attending daily lectures, grand rounds, journal clubs, and simulation labs to build their foundational knowledge. They are also responsible for teaching medical students.
---
### A Day in the Life of a CA-1 (PGY-2) Anesthesiology Resident
To make this tangible, let's walk through a typical day for a second-year resident on a general surgery rotation.
- 5:30 AM - Arrive at the Hospital: The day begins before sunrise. The first task is to check the operating room (OR) schedule. The resident is assigned to a complex abdominal surgery case and a shorter laparoscopic procedure. They head to their assigned OR to perform a thorough machine check, ensuring the anesthesia machine, monitors, and airway equipment are all functioning perfectly. They draw up all the anticipated emergency and standard medications for the day.
- 6:15 AM - Pre-Op Holding: The resident meets their first patient in the preoperative area. They review the patient's chart, confirm their medical history, explain the anesthetic plan in simple terms, answer any last-minute questions, and obtain consent. They place an IV line and administer any pre-medication as needed.
- 7:30 AM - Wheels In: The patient is brought into the OR. The resident, along with the attending anesthesiologist, connects the patient to standard monitors (ECG, pulse oximeter, blood pressure cuff).
- 7:45 AM - Induction: This is a critical moment. Under the attending's direct supervision, the resident administers intravenous induction agents. Once the patient is unconscious, they manage the airway, intubating the patient to secure a breathing passage, and connect them to the ventilator. They confirm proper placement and begin administering anesthetic gas.
- 8:00 AM - 1:00 PM - Intraoperative Management: The surgery begins. For the next five hours, the resident's focus is solely on the patient. They are charting vital signs every few minutes, adjusting anesthetic depth, administering fluids and medications to keep blood pressure stable, and communicating with the surgical team. They might place an arterial line for more accurate blood pressure monitoring.
- 1:00 PM - Emergence & Extubation: As the surgery concludes, the resident begins to lighten the anesthesia. Once the patient is breathing on their own and meeting specific criteria, the breathing tube is removed (extubation).
- 1:15 PM - PACU Handoff: The resident transports the patient to the Post-Anesthesia Care Unit (PACU) and gives a detailed handoff report to the PACU nurse, outlining the surgery, anesthetic course, and potential recovery issues. They write postoperative orders for pain and nausea management.
- 1:45 PM - Quick Lunch & Prep for Case 2: A brief 15-minute break for food before preparing for the next case.
- 2:30 PM - 5:00 PM - Second Case: The process repeats for a shorter laparoscopic cholecystectomy, which presents its own unique challenges.
- 5:30 PM - Sign-Out: After handing off the second patient to the PACU, the resident checks on their first patient and ensures all tasks are complete. They then find the on-call resident to give a thorough sign-out on their patients for the night.
- 6:00 PM - Didactics/Study: The resident might attend an evening lecture or head to the hospital library to read up on a complex case for the next day.
- 7:00 PM - Head Home: After a 13.5-hour day, the resident heads home to eat, study, and get enough sleep to do it all over again.
This demanding schedule underscores why residency is a period of intense learning and personal sacrifice, supported by a modest but essential stipend.
Average Anesthesiologist Resident Salary: A Deep Dive
An anesthesiologist resident's salary is not determined by performance or the number of procedures performed but is a fixed stipend based on their Post-Graduate Year (PGY) level. This compensation structure is standard across all medical residencies in the United States.
The primary and most authoritative source for this data is the Association of American Medical Colleges (AAMC), which conducts an annual survey of resident/fellow stipends. According to the AAMC's 2023 Report on Resident/Fellow Stipends and Benefits, the national average stipend for a first-year resident (PGY-1) was $63,013. This figure increases incrementally with each year of training.
Other data aggregators provide similar figures. For example, Medscape's 2023 Resident Salary & Debt Report found the average resident salary across all specialties and years to be $67,400.
Here's a detailed breakdown of how salary progresses through the typical four-year anesthesiology residency track.
| Post-Graduate Year (PGY) | Anesthesiology Title | National Average Salary (AAMC 2023) | Typical Salary Range |
| :--- | :--- | :--- | :--- |
| PGY-1 | Intern | $63,013 | $58,000 - $70,000 |
| PGY-2 | CA-1 Resident | $65,309 | $60,000 - $75,000 |
| PGY-3 | CA-2 Resident | $67,737 | $63,000 - $78,000 |
| PGY-4 | CA-3 Resident (Chief) | $70,266 | $65,000 - $85,000 |
*Source: AAMC Survey of Resident/Fellow Stipends and Benefits, 2023. Ranges are estimates based on geographic and institutional variations.*
It's important to note that a PGY-4 resident who serves as a Chief Resident often receives an additional stipend, typically ranging from $1,500 to $5,000 per year, in recognition of their added administrative and leadership responsibilities.
For residents who choose to pursue further subspecialty training through a one-year fellowship after residency (e.g., in Cardiac Anesthesiology, Pediatric Anesthesiology, or Pain Medicine), they would be considered a PGY-5. The average salary for a PGY-5 fellow, according to the AAMC, is approximately $72,693.
### Deconstructing the Full Compensation Package
While the base stipend is the headline number, the total compensation package for a resident is more comprehensive. Residency programs compete for the best applicants, and benefits are a key part of the offering. These are often valued at an additional $15,000 to $25,000 per year.
Common Components of a Resident's Compensation Package:
- Health Insurance: Comprehensive health, dental, and vision insurance for the resident and often for their family at a heavily subsidized rate. This is a significant financial benefit.
- Malpractice Insurance: Professional liability insurance is fully covered by the hospital. This protects the resident from the financial risk of litigation related to the care they provide under supervision.
- Disability and Life Insurance: Programs typically provide both short-term and long-term disability insurance, as well as a basic life insurance policy. This provides a crucial safety net.
- Retirement Savings Plans: Access to hospital-sponsored retirement plans, such as a 403(b) or 401(k). Many institutions offer a matching contribution (e.g., matching 50% of contributions up to 6% of salary), which is essentially free money and a critical tool for starting long-term savings.
- Paid Time Off (PTO): Residents typically receive 3 to 4 weeks of paid vacation per year. This is scheduled carefully to not interfere with clinical rotation requirements.
- Educational Stipend/Fund: An annual allowance, often ranging from $500 to $2,500, to be used for educational expenses. This can cover the cost of textbooks, medical equipment (like stethoscopes), board exam fees (e.g., the USMLE Step 3), or travel to academic conferences.
- Meal Allowance/Stipend: Many hospitals provide a meal card or stipend for use in the hospital cafeteria, especially when residents are on call.
- Licensing and Certification Fees: The program often covers the cost of state medical license fees and DEA registration fees.
- Other Perks: Depending on the program, other benefits can include free parking, gym memberships, lab coats/scrubs, and wellness resources or counseling services.
When evaluating residency programs, it is critical to look beyond the base salary and consider the total value of the benefits package. A program with a slightly lower stipend but an excellent health insurance plan and a generous 403(b) match may be a financially superior choice in the long run.
Key Factors That Influence an Anesthesiologist Resident's Salary
While the resident salary structure appears straightforward, several factors create significant variation in the actual dollar amount a resident earns. Understanding these nuances is key to managing financial expectations and making informed decisions when ranking residency programs. This section, the most detailed in our guide, will break down every element that shapes your income during training.
---
### `
` Post-Graduate Year (PGY) Level: The Primary Determinant
As established, the single most significant factor dictating a resident's salary is their year of training. This is a non-negotiable, standardized system within every single residency program. Your PGY level is a direct proxy for your experience and level of responsibility.
- PGY-1 (Intern Year): This is your first year out of medical school. You are learning the fundamentals of patient care and the hospital system. The salary is at its lowest point. For anesthesiology, this year is often spent in internal medicine or surgery. Average Stipend: ~$63,000.
- PGY-2 (CA-1 Year): This is your first year of dedicated clinical anesthesiology training. You are learning the basics of the operating room, airway management, and pharmacology. The learning curve is steep. You receive a pay bump to reflect your progression. Average Stipend: ~$65,000.
- PGY-3 (CA-2 Year): You are now a senior resident. You are expected to handle more complex cases, manage sicker patients, and begin to work with more autonomy (always under supervision). You start rotating through subspecialties like cardiac, obstetrics, and pediatrics. Your salary increases accordingly. Average Stipend: ~$67,500.
- PGY-4 (CA-3 Year): In your final year, you are functioning at a near-attending level. You take on the most challenging cases, lead teams, and are heavily involved in teaching junior residents and medical students. Many residents serve as Chief Resident during this year, earning an additional stipend for their leadership duties. This year commands the highest salary of residency. Average Stipend: ~$70,000+.
The year-over-year increase is typically around 3-5%. This is not a "raise" in the traditional sense; it's a pre-determined step-up in the pay scale that acknowledges your increasing value and contribution to the hospital.
---
### `
` Geographic Location: The Cost-of-Living Equalizer
After PGY level, geographic location is the most powerful influencer of resident salaries. A PGY-2 resident in New York City will earn significantly more in nominal dollars than a PGY-2 in rural Arkansas. However, this difference is almost entirely driven by Cost of Living Adjustments (COLAs).
Hospitals in high-cost-of-living areas (HCOL) must offer higher salaries to attract residents who can afford to live there. Conversely, programs in low-cost-of-living (LCOL) areas can offer lower nominal salaries that still provide comparable, or even superior, purchasing power.
Let's examine some real-world examples to illustrate this disparity:
High-Cost-of-Living Programs (2023-2024 Academic Year Data):
- Stanford University (Palo Alto, CA): PGY-1: $83,720; PGY-2: $86,403; PGY-3: $90,438. Includes an additional housing stipend.
- NYP Hospital (Columbia/Weill Cornell, New York, NY): PGY-1: $78,500; PGY-2: $81,200; PGY-3: $86,800. Also includes a housing stipend.
- Massachusetts General Hospital (Boston, MA): PGY-1: $75,600; PGY-2: $77,900; PGY-3: $80,500.
Mid- to Low-Cost-of-Living Programs (2023-2024 Academic Year Data):
- University of Alabama Medical Center (Birmingham, AL): PGY-1: $60,278; PGY-2: $62,025; PGY-3: $64,289.
- The University of Texas Health Science Center at Houston: PGY-1: $61,500; PGY-2: $63,500; PGY-3: $65,500.
- University of Nebraska Medical Center (Omaha, NE): PGY-1: $62,359; PGY-2: $64,528; PGY-3: $66,739.
The Crucial Analysis: A resident at Stanford earns over $20,000 more per year than a resident at the University of Alabama. However, the median rent for a one-bedroom apartment in Palo Alto is over $3,000, while in Birmingham it's closer to $1,100. When you factor in taxes, food, and transportation, the resident in Alabama may have more disposable income at the end of the month.
Actionable Advice: Do not be swayed by a high nominal salary alone. When comparing programs, use a cost-of-living calculator to compare the salaries. A higher salary in an expensive city may actually represent a net financial loss compared to a lower salary in an affordable one.
---
### `
` Institution Type and Funding Source
The type of hospital or medical center hosting the residency program can also influence salary and benefits. This is often tied to the institution's funding model, prestige, and whether its residents are unionized.
- Major Academic Medical Centers (e.g., Johns Hopkins, UCSF, Mayo Clinic): These institutions are often the leaders in research and education. They tend to offer highly competitive salaries and robust benefits packages to attract top-tier applicants. They are often, but not always, the highest-paying programs, especially those in HCOL areas.
- State University Hospitals: These are public institutions funded by the state. Salaries are often very competitive and transparent, set by the university system. They may offer additional benefits like tuition remission for spouses or access to state pension plans.
- Community Hospital Programs: These programs may be university-affiliated or independent. Their salaries can be more variable. Some larger, well-funded community programs in affluent suburbs may offer excellent salaries to compete with academic centers. Smaller or more rural programs may offer lower stipends that are still very competitive relative to the local cost of living.
- Government/VA Hospitals: Residents rotating through Veterans Affairs (VA) hospitals are part of programs affiliated with a university, but the funding for their positions comes directly from the federal government's Graduate Medical Education (GME) budget. Salaries are typically aligned with their sponsoring academic institution.
The Role of GME Funding: The majority of resident salaries are funded by Medicare through GME payments to teaching hospitals. This system is complex, and the amount a hospital receives is based on a formula that has been largely frozen for decades. This is why resident salaries have not kept pace with inflation or the value residents provide.
The Impact of Unionization: A growing trend in residency is the formation of resident unions, such as the Committee of Interns and Residents (CIR-SEIU). In unionized hospitals, resident salaries, benefits, and working conditions are subject to collective bargaining. This often results in higher base salaries, guaranteed annual raises, and better benefits (e.g., larger educational funds, better parental leave policies) compared to non-unionized programs in the same region. When considering a program, checking if they have an active resident union can be a significant factor.
---
### `
` The Influence of Future Specialization (Fellowship)
While a resident's current salary is standardized by PGY level, the *choice* of residency program can be heavily influenced by one's future earning potential in a subspecialty. Anesthesiology offers several highly sought-after, one-year fellowships that lead to dramatically different career paths and compensation levels *after* residency. A program with a strong track record of placing residents into competitive fellowships is highly desirable.
The salary during the fellowship year itself (as a PGY-5) will only be a few thousand dollars higher than the final year of residency. The real financial impact is on the attending salary that follows.
Major Anesthesiology Fellowships and Their Impact on Future Attending Salary:
- Pain Medicine: This is one of the most competitive and lucrative fellowships. Pain medicine specialists can work in a variety of settings and have significantly higher earning potential, often in the $500,000 to $750,000+ range.
- Cardiac Anesthesiology: Specialists who provide anesthesia for complex cardiac surgeries like bypass grafts and valve replacements. This demanding field commands a premium salary, typically $450,000 to $650,000.
- Pediatric Anesthesiology: Providing anesthesia for children, from newborns to teenagers, requires specialized skills and knowledge. Attending salaries are very strong, often in the $425,000 to $600,000 range.
- Critical Care Medicine: A fellowship in critical care allows an anesthesiologist to work as an intensivist in the ICU. This dual certification is highly valuable. Earning potential is robust, typically $400,000 to $550,000.
- Obstetric Anesthesiology: Focusing on pain relief (epidurals) and anesthetic management for labor and delivery, including high-risk pregnancies. Salaries are comparable to general anesthesiologists, often $400,000 to $550,000.
A residency program that has its own competitive fellowship programs or is known as a "feeder" program into top fellowships across the country can be a strategic choice, even if its resident stipend is not the absolute highest.
---
### `
` High-Value Skills and Competencies
During residency, you are not just working; you are building a portfolio of skills. While these skills don't directly increase your resident salary, they make you a more competent physician and a more competitive candidate for fellowships and future attending positions (which is the ultimate financial goal).
Skills That Increase Your Long-Term Value: