Introduction

Have you ever envisioned a career that places you at the very heart of a community's well-being? A role where you are not just a clinician treating a symptom, but a trusted advisor, a health advocate, and a constant presence through every stage of a family's life? This is the profound reality of a Family Medicine Physician. It's a calling that demands immense dedication, empathy, and intellectual rigor, but it offers rewards that are both deeply personal and financially substantial. For those drawn to this path, a pressing question often arises: what is the average salary for family medicine? The answer is compelling, with most family doctors earning well into the six figures, typically ranging from $200,000 to over $300,000 annually, depending on a host of factors we will explore in detail.
The financial compensation is undeniably a significant aspect of this profession, reflecting the years of strenuous education and the critical responsibilities involved. I vividly recall my own childhood family doctor. He was a kind, patient man who not only diagnosed my ear infections but also took the time to ask about school and sports, subtly gauging my overall well-being. He was the first call my parents made for any health concern, big or small, a testament to the trust he had built. That relationship, that fusion of science and human connection, is the essence of family medicine and a core reason why, despite its challenges, the career remains one of the most respected and fulfilling in all of healthcare.
This guide is designed to be your definitive resource, whether you are a high school student dreaming of a white coat, a medical student choosing a specialty, or a practicing physician considering a career pivot. We will move beyond the simple averages to provide a granular, data-driven analysis of every facet of a career in family medicine. We will dissect compensation, explore the factors that drive salary higher, project the future of the profession, and lay out the complete step-by-step roadmap to becoming a board-certified Family Medicine Physician.
### Table of Contents
- [What Does a Family Medicine Physician Do?](#what-does-a-family-medicine-physician-do)
- [Average Family Medicine Physician Salary: A Deep Dive](#average-family-medicine-physician-salary-a-deep-dive)
- [Key Factors That Influence Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth](#job-outlook-and-career-growth)
- [How to Get Started in This Career](#how-to-get-started-in-this-career)
- [Conclusion](#conclusion)
---
What Does a Family Medicine Physician Do?

A Family Medicine Physician, often called a family doctor or general practitioner, is a medical specialist who provides comprehensive, continuous healthcare for individuals and families across all ages, genders, diseases, and parts of the body. They are the quintessential "front line" of medicine. Unlike other specialists who focus on a specific organ (like a cardiologist) or a specific patient population (like a pediatrician), a family physician's specialty is defined by the patient relationship.
Their scope of practice is exceptionally broad, encompassing pediatrics, adolescent medicine, adult medicine, and geriatrics. They are trained to manage a wide spectrum of acute, chronic, and preventative medical issues. The cornerstone of their practice is continuity of care—the process of building a long-term relationship with a patient to provide the most effective and personalized care over their lifetime. This longitudinal relationship allows them to understand a patient's history, family dynamics, and lifestyle, which is invaluable for both diagnosis and preventative health.
Core Responsibilities and Daily Tasks:
A family physician's duties are varied and require a versatile skill set. Their work can be broken down into several key areas:
- Diagnosis and Treatment of Acute Illnesses: This includes everything from the common cold, flu, and strep throat to infections, minor injuries, and rashes. They are often the first point of contact for any new, undiagnosed symptom.
- Management of Chronic Conditions: A significant portion of their work involves helping patients manage long-term health issues like hypertension (high blood pressure), diabetes, asthma, depression, anxiety, and heart disease. This includes regular check-ins, medication management, and lifestyle counseling.
- Preventative Care and Health Screenings: Family doctors are champions of preventative medicine. They perform annual physicals, well-child check-ups, and cancer screenings (e.g., Pap smears, mammogram referrals, colonoscopy referrals). They also administer vaccinations and provide guidance on diet, exercise, and smoking cessation.
- Patient Education: A crucial task is explaining complex medical information in an understandable way. They educate patients about their conditions, treatment options, and how to maintain a healthy lifestyle.
- Coordination of Care: When a patient requires specialized care, the family physician acts as the central coordinator or "quarterback" of the healthcare team. They refer patients to specialists (like cardiologists, dermatologists, or surgeons) and communicate with them to ensure the patient's overall care plan is cohesive.
- Minor In-Office Procedures: Depending on their training and practice setup, many family doctors perform minor surgical procedures such as suturing lacerations, removing skin lesions, draining abscesses, and giving joint injections.
### A Day in the Life of a Family Medicine Physician
To make this tangible, let's walk through a typical day for a hospital-employed family physician:
- 7:30 AM - 8:30 AM: Arrive at the clinic. Log into the Electronic Health Record (EHR) system. Review lab results, imaging reports, and consultant notes that came in overnight. "Pre-chart" for the day's first few patients, reviewing their history and recent issues to be prepared.
- 8:30 AM - 12:00 PM: Patient appointments, typically scheduled in 15- to 20-minute slots. The morning might include a 6-month-old's well-child check, a 45-year-old with a new-onset back pain, a follow-up with a 68-year-old diabetic to review blood sugar logs, and an urgent visit for a 25-year-old with a sore throat and fever.
- 12:00 PM - 1:00 PM: A hurried lunch while catching up on "pended" charts—finishing notes from the morning's visits. Respond to urgent patient messages via the online portal and sign prescription refill requests.
- 1:00 PM - 4:30 PM: The afternoon patient schedule continues. This block could feature an annual physical for a healthy 30-year-old, a consultation for a teenager struggling with anxiety, a Medicare Wellness Visit for an 80-year-old patient, and a minor procedure to remove a suspicious mole.
- 4:30 PM - 6:00 PM (or later): "Desktop medicine" begins. This is dedicated time for administrative tasks. The physician finishes all patient notes for the day, makes phone calls to patients to discuss sensitive lab results, completes paperwork for insurance prior authorizations, and reviews and signs off on charts handled by their medical assistant or nurse. They might also have a quick meeting with the office manager about clinic logistics.
This schedule highlights the intense blend of direct patient interaction and demanding administrative work that defines the role. It is a career of constant context-switching, requiring deep medical knowledge, excellent communication skills, and remarkable efficiency.
---
Average Family Medicine Physician Salary: A Deep Dive
The financial compensation for family physicians is a direct reflection of their extensive education, rigorous training, and the critical role they play in the healthcare system. While they are not the highest-paid medical specialists (a title often held by surgical and procedural subspecialties like neurosurgery or cardiology), they earn a very competitive and substantial income. Understanding the average salary for family medicine requires looking at data from multiple authoritative sources, as methodologies and reported figures can vary slightly.
National Averages and Typical Salary Ranges
Let's examine the most recent data from leading industry reports:
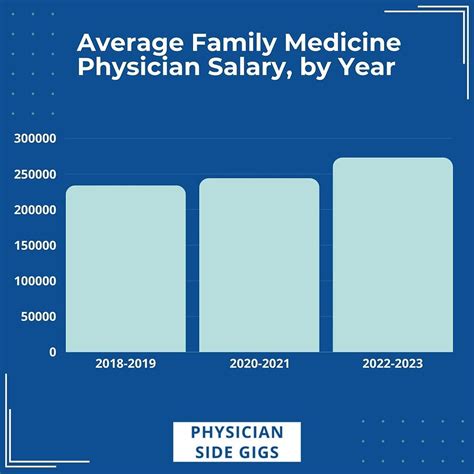
- Medscape Physician Compensation Report 2023: This is one of the most widely cited reports in the industry, based on a large survey of practicing physicians. It reports the average annual income for family physicians as $255,000. This figure includes salary, bonuses, and any profit-sharing contributions.
- Doximity 2023 Physician Compensation Report: Another highly respected source, Doximity's report places the average compensation for family medicine even higher, at $273,040. This highlights the upward trend in primary care compensation.
- U.S. Bureau of Labor Statistics (BLS): The BLS provides robust government data. As of May 2022 (the most recent detailed data), the median annual wage for "Family and General Practitioners" was $224,460. The BLS provides a wide percentile range, which is extremely useful for understanding the full spectrum of earnings:
- Lowest 10%: earned less than $106,540
- Median (50%): earned $224,460
- Highest 90%: earned more than $239,000 (Note: The BLS often has a top-end wage cap in its public data, which can underrepresent the highest earners).
- Salary.com: This aggregator provides real-time employer-reported data. As of late 2023, it shows the median salary for a Family Practice Physician in the U.S. is $226,390, with a typical range falling between $199,444 and $259,578.
Synthesizing the Data:
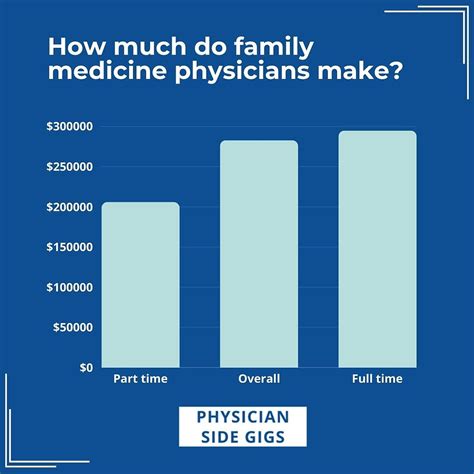
By triangulating these sources, we can confidently state that the national average salary for a family medicine physician in the United States is between $240,000 and $270,000 per year. The typical salary range for an established physician is broad, generally spanning from $200,000 to over $320,000. Physicians just starting their careers after residency will be at the lower end of this range, while highly experienced physicians, practice owners, or those in high-demand locations can easily exceed the upper end.
### Compensation by Experience Level
Salary in medicine grows predictably with experience. As a physician builds a patient base, becomes more efficient, and potentially takes on leadership roles or ownership, their compensation increases.
| Experience Level | Typical Annual Salary Range | Key Characteristics |
| :--- | :--- | :--- |
| Entry-Level (0-3 Years Post-Residency) | $190,000 - $235,000 | Just completed 3-year residency. Often on a guaranteed salary for the first 1-2 years before moving to a production-based model. Focused on building a patient panel. |
| Mid-Career (4-10 Years) | $235,000 - $285,000 | Has an established and full patient panel. Highly efficient with clinical and administrative tasks. Often earning significant production bonuses. May begin taking on leadership roles. |
| Senior/Experienced (11-20+ Years) | $260,000 - $350,000+ | Deeply established in the community. Potentially a partner or owner of a private practice, sharing in profits. May hold significant administrative titles like Medical Director. Peak earning years. |
### Breakdown of a Total Compensation Package
A family physician's income is rarely just a flat salary. The total compensation package is a complex mix of components designed to reward productivity, quality, and long-term commitment.
1. Base Salary: This is the guaranteed, fixed portion of a physician's pay. In employed models (e.g., hospital-owned clinics), this might be the entire compensation for the first 1-2 years to provide stability while the physician builds their practice. In private practice or mature employed roles, the base salary might be lower, with a greater emphasis on bonuses.
2. Production Bonuses (RVU-Based): This is the most common form of incentive compensation.
- What is an RVU? A Relative Value Unit (RVU) is a standardized measure of value used by Medicare to determine physician payment. Every patient encounter and procedure is assigned an RVU value based on the time, skill, and intensity required.
- How it Works: A physician is often given an RVU target for the year. If they exceed this target, they receive a bonus payment for each additional RVU generated. For example, a contract might state a bonus of $50 for every wRVU (work RVU) generated over a threshold of 4,500 per year. This model directly rewards seeing more patients or performing more complex services.
3. Quality & Performance Bonuses: With the shift towards value-based care, many compensation models now include bonuses tied to quality metrics rather than just volume. These can include:
- Achieving certain levels of patient satisfaction scores.
- Meeting targets for preventative care (e.g., percentage of diabetic patients with controlled A1c levels, percentage of eligible patients receiving cancer screenings).
- Efficiently managing healthcare costs for their patient population.
4. Sign-On Bonus: To attract physicians, especially in underserved areas, health systems and practices often offer a significant one-time payment upon signing a contract. These can range from $10,000 to $50,000 or more, but they almost always come with a commitment to stay for a certain period (e.g., 2-3 years).
5. Profit Sharing & Partnership Track (Private Practice): For physicians in private groups, the ultimate financial goal is often partnership. After a few years as an employee, a physician may be offered the opportunity to "buy-in" to the practice. As a partner, they receive a share of the practice's overall profits in addition to their own clinical earnings, which can significantly increase their total income.
6. Comprehensive Benefits: The value of the benefits package should not be underestimated and can be worth an additional $40,000-$60,000 per year. Standard physician benefits include:
- Health, Dental, and Vision Insurance: For the physician and their family.
- Malpractice Insurance: Typically a "claims-made" or "occurrence" policy, paid for by the employer. This is a massive expense and a critical benefit.
- Retirement Savings Plans: 401(k) or 403(b) plans, often with a generous employer match.
- Continuing Medical Education (CME) Allowance: An annual stipend (e.g., $3,000 - $5,000) and paid time off to attend conferences and maintain medical knowledge.
- Paid Time Off (PTO): Usually 4-6 weeks per year for vacation and sick leave.
- Licensing and Dues: Reimbursement for state medical license fees, DEA license, and membership in professional societies like the American Academy of Family Physicians (AAFP).
---
Key Factors That Influence Salary

The national average salary for a family medicine physician provides a useful benchmark, but an individual's actual earnings are determined by a complex interplay of factors. Location, practice type, and specific skills can create salary variations of over $100,000 per year. Understanding these variables is critical for anyone planning their career and negotiating their compensation.
###
Geographic Location: The Power of Place
Geography is arguably the single most significant factor influencing a physician's salary. The dynamics of supply and demand create vast disparities in compensation between different states and between urban, suburban, and rural areas.
State-by-State Variations:
Contrary to what many might assume, the highest-paying states are often not those with the highest cost of living. Instead, they are frequently states in the Midwest and Southeast that are actively recruiting physicians to meet the needs of their populations.
- Highest-Paying States for Family Medicine (Average Annual Salary):
1. Wisconsin: ~$310,000
2. Indiana: ~$305,000
3. Georgia: ~$301,000
4. Alabama: ~$298,000
5. Oklahoma: ~$295,000
*(Source: Aggregated data from Doximity and Medscape 2023 reports)*
- Lowest-Paying States for Family Medicine (Average Annual Salary):
1. Maryland: ~$220,000
2. Massachusetts: ~$235,000
3. District of Columbia: ~$238,000
4. Rhode Island: ~$240,000
5. New York: ~$245,000
*(Source: Aggregated data from Doximity and Medscape 2023 reports)*
The stark difference is clear: a physician in Wisconsin may earn nearly $90,000 more per year than one in Maryland for performing the exact same job. This is often due to a higher concentration of physicians and academic centers in the Northeast, leading to more competition for positions.
Rural vs. Urban Divide:
The need for primary care is particularly acute in rural America. To attract physicians to these underserved communities, hospitals and clinics offer significantly higher salaries, generous sign-on bonuses, and sometimes even student loan repayment assistance.
- Rural/Underserved Areas: A family physician might be offered a starting salary of $275,000 or more, with a $50,000 sign-on bonus and a loan repayment program through the National Health Service Corps (NHSC). The trade-off is often a more demanding call schedule and fewer local amenities.
- Major Metropolitan Areas (e.g., New York City, San Francisco, Boston): Salaries here are often lower than the national average, despite the extremely high cost of living. The abundance of training programs creates a large supply of physicians who want to stay in these desirable urban centers, which suppresses wages.
Cost of Living Consideration:
It's crucial to analyze salary in the context of the local cost of living. A $250,000 salary in Omaha, Nebraska, provides a much higher standard of living than a $260,000 salary in San Diego, California. Aspiring physicians should use cost-of-living calculators to compare the real-world value of job offers in different locations.
###
Practice Setting & Ownership Model
Where a physician chooses to work has a profound impact on their work-life balance, autonomy, and earning potential.
- Private Practice (Physician-Owned): This setting offers the highest earning potential but also the most risk and administrative burden.
- Associate: A physician starts as a salaried employee.
- Partner: After 2-3 years, they may be offered partnership. This involves "buying in" to the practice, making them a part-owner. As a partner, they share in the practice's profits, which can lead to incomes well over $350,000-$400,000. However, they are also responsible for the business side of medicine: managing staff, payroll, billing, and overhead.
- Hospital or Health System-Employed: This is now the most common employment model. The hospital system owns the clinic, employs the staff, and handles all administrative tasks.
- Pros: Predictable salary, robust benefits, no business-related headaches, built-in referral network.
- Cons: Less autonomy over scheduling, staffing, and clinical practices. Earning potential is generally capped lower than that of a private practice owner. The average salary often aligns closely with the national figures of $250,000-$280,000.
- Academic Medical Centers: Physicians at university-affiliated hospitals split their time between seeing patients, teaching medical students and residents, and conducting research.
- Compensation: Salaries are consistently lower than in private or hospital-employed settings, often by 10-20%. A typical academic salary might be in the $200,000 - $230,000 range.
- Benefits: The rewards are non-monetary: the prestige of an academic title, the intellectual stimulation of teaching and research, and often excellent institutional benefits.
- Urgent Care Centers: These facilities bridge the gap between primary care and the emergency room.
- Compensation: Pay is often hourly (e.g., $100-$130/hour) or a fixed salary. Full-time annual compensation is competitive, often ranging from $220,000 to $260,000. The work is fast-paced and shift-based, which can be appealing for those seeking a predictable schedule with no long-term patient management.
- Direct Primary Care (DPC): This is a newer, innovative model where physicians opt out of the insurance system. Patients pay a monthly membership fee (e.g., $75-$150) for direct, unlimited access to their doctor.
- Income: A DPC physician with a full panel of 500-600 patients can generate a gross revenue of $450,000-$600,000 per year. After covering much lower overhead (no billing staff), their take-home pay can be very competitive, while allowing for longer appointment times and a better work-life balance.
###
Sub-Specialization and Procedural Skills (Fellowships)
While family medicine is a broad specialty, physicians can pursue an additional year of fellowship training to gain expertise in a specific area. This can enhance job prospects and increase earning potential.
- Family Medicine with Obstetrics (FM-OB): Physicians who complete an OB fellowship are trained to provide prenatal care and perform vaginal deliveries and C-sections. This is a highly sought-after skill, especially in rural areas, and can add $30,000 to $70,000 to a physician's annual salary due to the increased workload, call schedule, and procedural component.
- Sports Medicine: A sports medicine fellowship prepares a physician to manage non-operative musculoskeletal injuries. They often work in specialized orthopedic clinics or serve as team physicians. This can lead to salaries in the $280,000 to $350,000 range.
- Geriatrics: With an aging population, geriatricians are in high demand. While a fellowship doesn't always lead to a massive salary jump, it opens doors to leadership roles in nursing homes, long-term care facilities, and specialized geriatric clinics.
- Palliative and Hospice Medicine: This fellowship focuses on managing symptoms and improving the quality of life for patients with serious illnesses. It leads to roles as a Hospice Medical Director or palliative care consultant, with salaries comparable to general family medicine but with a different practice focus.
###
Years of Experience and Board Certification
As detailed in the salary deep-dive section, experience is a linear driver of income. A physician's efficiency, patient panel size, and value to an organization grow over time, and compensation follows