For those called to a career that blends cutting-edge medical science with profound human compassion, few roles are as compelling or as critical as that of a neonatal nurse. These highly specialized professionals are the guardians of the most fragile patients in our healthcare system: newborns who are premature, critically ill, or born with congenital defects. It is a career demanding immense skill, emotional resilience, and a deep commitment to care. But beyond the profound intrinsic rewards, a career as a neonatal nurse offers significant financial stability and a robust professional trajectory. This guide will illuminate the financial landscape of this vital profession, exploring the average salary of a neonatal nurse and the many factors that shape it.
I once spoke with a veteran NICU (Neonatal Intensive Care Unit) nurse who had been in the field for over two decades. She told me, "You're not just taking care of a baby; you're holding a family's entire world in your hands. The salary allows me to live a comfortable life, but the real compensation is seeing a one-pound infant grow, thrive, and finally go home with their parents." This sentiment perfectly captures the dual nature of this career—it is both a calling and a highly respected profession with competitive earning potential.
This comprehensive guide will break down everything you need to know about neonatal nurse salaries, from national averages to the specific skills that can increase your pay. We will explore the career outlook, the steps required to enter the field, and how you can build a long and prosperous career at the forefront of neonatal care.
### Table of Contents
- [What Does a Neonatal Nurse Do?](#what-does-a-neonatal-nurse-do)
- [Average Neonatal Nurse Salary: A Deep Dive](#average-neonatal-nurse-salary-a-deep-dive)
- [Key Factors That Influence a Neonatal Nurse's Salary](#key-factors-that-influence-salary)
- [Job Outlook and Career Growth for Neonatal Nurses](#job-outlook-and-career-growth)
- [How to Become a Neonatal Nurse: Your Step-by-Step Guide](#how-to-get-started-in-this-career)
- [Conclusion: Is a Career as a Neonatal Nurse Right for You?](#conclusion)
---
What Does a Neonatal Nurse Do?

A neonatal nurse is a Registered Nurse (RN) who specializes in the care of newborn infants, typically up to the first 28 days of life. While this sounds straightforward, the reality of the role is complex and multifaceted, taking place almost exclusively within a hospital's Neonatal Intensive Care Unit (NICU). These units are categorized into different levels of care, which dictates the nurse's specific responsibilities:
- Level I (Well Newborn Nursery): Cares for healthy, full-term newborns. This is the least intensive level.
- Level II (Special Care Nursery): Cares for infants born prematurely (typically >32 weeks) or those with moderate health issues who require specialized monitoring, feeding support (like tube feedings), and intravenous therapy.
- Level III (Neonatal Intensive Care Unit - NICU): Cares for infants born at less than 32 weeks gestation or those of any gestational age with critical illnesses. These infants require high-tech support like ventilators, advanced respiratory support, and critical interventions. This is where the majority of specialized neonatal nurses work.
- Level IV (Regional NICU): The highest level of care, located in specialized children's hospitals. These units care for the most complex and critically ill infants, often those requiring surgical intervention for congenital heart defects or other severe conditions.
The daily work of a neonatal nurse is a high-stakes blend of meticulous technical tasks, critical thinking, and compassionate communication.
Core Responsibilities and Daily Tasks:
- Continuous Monitoring: Closely observing vital signs (heart rate, respiratory rate, blood pressure, temperature, oxygen saturation) using sophisticated monitoring equipment.
- Administering Medications: Calculating precise dosages and administering medications, often intravenously.
- Respiratory Support: Managing ventilators, CPAP (Continuous Positive Airway Pressure) machines, and other respiratory therapies.
- Nutritional Management: Providing nutrition through intravenous lines (TPN - Total Parenteral Nutrition), gavage (tube) feedings, or assisting mothers with breastfeeding or bottle-feeding fragile infants.
- Diagnostic Procedures: Assisting physicians with procedures such as intubation, placing central lines, or performing lumbar punctures.
- Developmental Care: Creating a low-stimulation environment that mimics the womb to promote healthy brain development. This includes managing light and sound levels, and practicing clustered care to allow for long periods of rest.
- Family-Centered Care: This is a cornerstone of the role. Neonatal nurses are the primary educators and emotional support system for parents who are often terrified, overwhelmed, and grieving the loss of a "normal" birth experience. They teach parents how to care for their fragile infant, how to participate in their care (like kangaroo care/skin-to-skin contact), and provide updates on their child's condition.
### A Day in the Life of a NICU Nurse (Level III)
7:00 AM - Shift Handoff & Initial Assessment: The day begins with a detailed report from the night-shift nurse on the assigned infants (usually 1-3, depending on acuity). The nurse then performs a head-to-toe assessment on each baby, checking every system, evaluating lines and tubes, and reviewing the electronic health record for new orders.
9:00 AM - Rounds and Care Planning: The multidisciplinary team—including the neonatologist, residents, respiratory therapist, pharmacist, and social worker—conducts rounds. The nurse presents their infants' progress, advocates for their needs, and collaborates on the care plan for the next 24 hours.
11:00 AM - Medications and Feedings: The nurse meticulously prepares and administers scheduled medications. They manage complex IV drips and carry out the 11:00 AM feeding, which could be via a feeding tube or, if the baby is stable enough, by bottle.
1:00 PM - Family Interaction & Education: A baby's parents arrive. The nurse provides a gentle, honest update on their child's progress, explains the purpose of the various machines, and facilitates skin-to-skin contact, carefully moving the infant and all their attached lines and tubes onto the parent's chest.
3:00 PM - Responding to an Unplanned Event: An alarm sounds. An infant is experiencing apnea (a pause in breathing). The nurse immediately intervenes, providing gentle stimulation. When the baby doesn't respond, they begin bag-mask ventilation to support breathing until the infant stabilizes, all while calmly communicating the situation to the wider team.
5:00 PM - Documentation and Evening Care: The nurse meticulously documents every assessment, intervention, and patient response from the shift. They prepare for the next round of medications and feedings, change diapers, and reposition the infants to prevent pressure sores.
7:00 PM - Shift Handoff: The night-shift nurse arrives. The nurse provides a thorough, detailed report on each infant, ensuring a safe and seamless transition of care before finally heading home.
---
Average Neonatal Nurse Salary: A Deep Dive

The compensation for a neonatal nurse reflects the high level of skill, responsibility, and stress associated with the role. While salaries can vary significantly based on several factors, the profession offers a strong and competitive income.
According to data from Salary.com, updated in late 2023, the median annual salary for a Neonatal Nurse in the United States is $84,280. However, this is just the midpoint. The typical salary range for the role falls between $76,730 (25th percentile) and $95,361 (75th percentile). The top 10% of earners in the field can command salaries well over $105,790.
Other reputable sources provide similar figures, painting a consistent picture of the earning landscape:
- Payscale.com reports a slightly lower average base salary of approximately $71,500 per year, but with bonuses and overtime, the total pay often aligns with the higher figures. Their data shows a range from $54,000 to $99,000.
- Glassdoor.com aggregates user-submitted data and reports a total pay estimate (including base salary and additional compensation) of around $101,577 per year.
- The U.S. Bureau of Labor Statistics (BLS) does not track neonatal nurses as a separate category. However, they provide extensive data for Registered Nurses (RNs) as a whole, which serves as an excellent baseline. The median annual wage for RNs was $86,070 in May 2023. The specialized nature of neonatal nursing often places these professionals in the upper half of this general RN salary range.
### Salary Progression by Experience Level
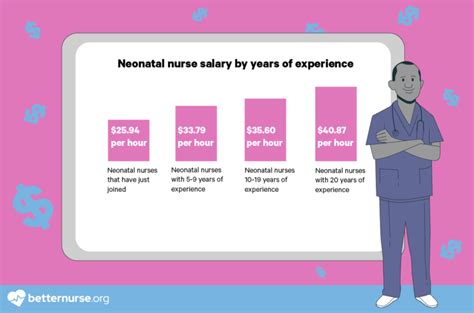
One of the most significant factors in salary is experience. A nurse's value, autonomy, and ability to handle high-acuity situations grow immensely over time, and compensation reflects this.
| Experience Level | Typical Salary Range (Annual) | Key Characteristics & Responsibilities |
| :--- | :--- | :--- |
| Entry-Level (0-2 Years) | $65,000 - $78,000 | Focus on foundational skills, often in a Level II NICU or with lower-acuity patients in a Level III. Requires close supervision and mentorship. Primary goal is competency and safety. |
| Mid-Career (3-9 Years) | $79,000 - $95,000 | Proficient and autonomous in caring for critically ill infants. Often takes on precepting/mentoring new nurses. May pursue certification (RNC-NIC) and take on charge nurse responsibilities. |
| Senior/Experienced (10-20 Years) | $96,000 - $115,000+ | Expert-level clinician. Manages the most complex patient assignments. Acts as a resource for the entire unit. Often involved in unit-based committees, quality improvement projects, or research. |
| Advanced Roles (15+ Years) | $110,000 - $140,000+ | Moves into leadership (Nurse Manager, Director), education (Clinical Nurse Specialist), or advanced practice (Neonatal Nurse Practitioner - NNP). *Note: NNP salaries are significantly higher.* |
*Source: Analysis of data from Salary.com, Payscale, and BLS, reflecting typical career progression.*
### A Closer Look at the Full Compensation Package
The base salary is only one part of the total compensation for a neonatal nurse. Due to the 24/7 nature of hospital care, additional pay and benefits form a substantial portion of total earnings.
- Shift Differentials: This is a critical component. Nurses who work evening shifts (typically 3 PM - 11 PM), night shifts (11 PM - 7 AM), or weekend shifts receive a significant hourly pay bump. This differential can range from $2 to $10+ per hour, adding thousands of dollars to an annual salary.
- Overtime Pay: Working more than 40 hours a week or extending a 12-hour shift results in overtime pay, typically calculated at 1.5 times the base hourly rate.
- On-Call Pay: Some roles, especially those related to transport teams, require nurses to be on-call. They receive a small hourly stipend for being available and their full hourly rate (or more) if they are called into work.
- Bonuses:
- Sign-On Bonuses: Hospitals facing staffing shortages often offer substantial sign-on bonuses, ranging from $5,000 to $25,000 or more, to attract experienced NICU nurses.
- Retention Bonuses: Awarded to nurses for staying with an employer for a specified period.
- Clinical Ladder Bonuses: Many hospitals have a "clinical ladder" program that financially rewards nurses for activities like earning a certification, leading a project, or presenting at a conference.
- Benefits: Comprehensive benefits packages are standard and add immense value. These typically include:
- Excellent health, dental, and vision insurance.
- Generous Paid Time Off (PTO).
- Retirement savings plans, such as a 401(k) or 403(b), often with employer matching.
- Tuition Reimbursement: Many hospital systems will pay for nurses to advance their education, such as completing a BSN or pursuing a Master's degree.
- Life and disability insurance.
When considering a job offer, it's crucial to evaluate the entire compensation package, as a lower base salary with excellent differentials, bonuses, and tuition reimbursement can be more valuable than a higher base salary with minimal perks.
---
Key Factors That Influence a Neonatal Nurse's Salary
While the national averages provide a useful benchmark, a neonatal nurse's actual salary is determined by a complex interplay of factors. Understanding these variables is key for new nurses seeking their first position and for experienced nurses looking to maximize their earning potential. This section provides an exhaustive breakdown of what truly drives compensation in this field.
###
Level of Education and Certification
Education is the foundation of a nursing career, and advancing your academic qualifications directly translates to higher earning potential and broader career opportunities.
- Associate Degree in Nursing (ADN): An ADN is the fastest path to becoming an RN. While it allows you to sit for the NCLEX-RN and enter the workforce, many major hospitals, particularly those with Magnet designation (a prestigious credential for nursing excellence), now require or strongly prefer a Bachelor of Science in Nursing (BSN). An ADN-prepared nurse might start at the lower end of the salary spectrum and may find it harder to secure positions in high-acuity Level III or IV NICUs.
- Bachelor of Science in Nursing (BSN): The BSN is considered the gold standard for professional nursing. It includes a more comprehensive curriculum covering nursing research, leadership, and public health. A BSN is often a prerequisite for advancement into roles like charge nurse, manager, or educator. Nurses with a BSN typically earn more than their ADN-prepared colleagues—an analysis by Payscale suggests a BSN can lead to an average salary that is 5-10% higher.
- Master of Science in Nursing (MSN) / Doctor of Nursing Practice (DNP): This is the pathway to becoming an Advanced Practice Registered Nurse (APRN), such as a Neonatal Nurse Practitioner (NNP) or a Clinical Nurse Specialist (CNS). This represents a monumental leap in both responsibility and salary. NNPs have a greatly expanded scope of practice, including diagnosing conditions, prescribing medications, and performing advanced procedures. Consequently, their salaries are substantially higher. According to the BLS, the median salary for all Nurse Practitioners was $126,260 in May 2023, with experienced NNPs in high-demand areas earning well over $150,000.
- Specialty Certifications: Obtaining a professional certification is one of the most direct ways for a staff-level neonatal nurse to increase their value and pay. The premier certification is the RNC-NIC (Neonatal Intensive Care Nursing) offered by the National Certification Corporation (NCC). Earning this credential requires a minimum of 2 years and 2,000 hours of specialized experience and passing a rigorous exam. It demonstrates a high level of knowledge and commitment. Many hospitals offer a direct salary increase or an annual bonus (often $1,000-$3,000) for certified nurses. Other valuable certifications include the CCRN (Neonatal) from the American Association of Critical-Care Nurses.
###
Years of Experience
As detailed in the previous section, experience is a powerful driver of salary growth. Here’s a more granular look at the trajectory:
- Novice to Competent (Years 0-2): A new graduate nurse or a nurse new to the NICU is in a learning phase. Their salary reflects their entry-level status. Pay increases are typically modest annual cost-of-living adjustments.
- Proficient (Years 3-5): By this stage, the nurse is comfortable with a wide range of patient conditions and technologies. They are a reliable team member and can act as a preceptor for new nurses. This is often when nurses achieve certification, leading to a noticeable salary jump.
- Expert (Years 5-15): The expert nurse is a unit leader, whether in a formal or informal capacity. They can handle the most critically unstable infants with confidence and often take on charge nurse duties. Their deep experience makes them invaluable, and their salary reflects this. They can command top-tier pay for their clinical skills.
- Veteran/Leadership (Years 15+): After decades of bedside experience, many nurses transition into formal leadership (manager, director), education, or advanced practice. This path provides the highest earning potential outside of becoming an NNP.
###
Geographic Location
Where you work is arguably the most significant factor influencing your salary. Pay scales are adjusted to reflect the local cost of living, demand for nurses, and the prevalence of unions.
Highest-Paying States for Registered Nurses (and thus, Neonatal Nurses):
According to 2023 BLS data for all Registered Nurses, these states offer the highest average annual salaries:
1. California: $137,690
2. Hawaii: $129,590
3. Oregon: $115,440
4. Washington: $113,630
5. Alaska: $110,670
Highest-Paying Metropolitan Areas:
Salaries can be even higher in specific metro areas within these states:
1. San Jose-Sunnyvale-Santa Clara, CA: $180,010
2. San Francisco-Oakland-Hayward, CA: $174,160
3. Vallejo-Fairfield, CA: $166,460
4. Napa, CA: $159,380
5. Salinas, CA: $154,670
It is crucial to note that these astronomical salaries are offset by an extremely high cost of living. A $150,000 salary in San Francisco may offer a similar quality of life to an $85,000 salary in the Midwest.
Lowest-Paying States:
Conversely, states with a lower cost of living tend to have lower average nursing salaries:
1. South Dakota: $68,770
2. Arkansas: $70,830
3. Alabama: $71,110
4. Mississippi: $72,670
5. Iowa: $73,150
Why the Discrepancy?
- Cost of Living: Employers must offer higher wages in expensive areas to attract talent.
- Nurse Unions: States like California, Oregon, and Washington have strong nursing unions (e.g., California Nurses Association) that negotiate for high wages, mandated nurse-to-patient ratios, and excellent benefits.
- Supply and Demand: Areas with nursing shortages may offer higher pay and sign-on bonuses to fill positions.
###
Facility Type and Size
The type of institution you work for also plays a major role in your compensation.
- Large, Urban, University-Affiliated Teaching Hospitals: These facilities, especially Magnet-designated ones, typically offer the highest salaries. They are often unionized, handle the most complex (Level IV NICU) cases, and have the budgets to support competitive pay and benefits. They also offer the most opportunities for education and career advancement.
- Private Non-Profit Hospitals: These are the most common type of hospital in the U.S. Salaries are generally competitive but may be slightly lower than large academic centers.
- For-Profit Hospital Systems: Compensation can be more variable. Some systems offer competitive pay to attract talent, while others may prioritize cost-cutting, potentially impacting staffing levels and salaries.
- Government/State Facilities: Nurses working in state, county, or city hospitals often have strong union representation and excellent government benefits and pension plans, though base salaries might be slightly less than top-tier private hospitals.
- Travel Nursing: For experienced NICU nurses (typically with at least 2 years of experience), travel nursing offers the highest earning potential by far. Agencies place nurses in short-term contracts (usually 13 weeks) at hospitals experiencing critical staffing shortages. These contracts include a high hourly wage plus tax-free stipends for housing and meals. A travel NICU nurse can easily earn $3,000 - $5,000+ per week, which translates to an annual income of over $150,000 - $200,000. However, this path lacks the stability and long-term benefits of a permanent position.
###
Area of Specialization (Level of Care and Sub-Specialty)
Within neonatal nursing, further specialization impacts pay.
- Level of Care: As acuity increases, so do the required skills and, often, the pay. A nurse in a high-acuity, 40-bed Level IV NICU will generally earn more than a nurse in a 10-bed Level II special care nursery within the same hospital system, often due to a "critical care differential."
- Neonatal Transport Team: These highly specialized nurses are responsible for stabilizing and transporting critically ill infants from community hospitals to a higher-level NICU. This role requires immense autonomy, advanced skills (like intubation in some regions), and the ability to perform under extreme pressure. Due to the on-call nature and advanced skillset, transport nurses often earn a premium salary.
- ECMO Specialist: ECMO (Extracorporeal Membrane Oxygenation) is a heart-lung bypass machine used for infants in severe cardiorespiratory failure. Nurses who receive specialized training to manage the ECMO circuit are considered elite specialists and receive a significant pay differential when performing this duty.
###
In-Demand Skills That Boost Your Salary
Beyond formal credentials, a portfolio of specific, high-value skills can make you a more attractive candidate and command a higher salary.
- Technical Proficiency: Mastery of NICU technology, including high-frequency oscillatory ventilators, nitric oxide therapy, and therapeutic hypothermia (cooling therapy for brain injury).
- Precepting and Mentoring: A willingness and ability to train new nurses is highly valued by managers and is often a prerequisite for the clinical ladder and promotion.
- Charge Nurse Experience: Taking on the responsibility of managing the unit flow, patient assignments, and staffing for a shift demonstrates leadership potential and is a stepping stone to management.
- Bilingualism: In many parts of the country, fluency in a second language (especially Spanish) is a major asset for communicating with diverse patient families and may come with a pay differential.
- Emotional Intelligence and Communication: While a "soft skill," the ability to communicate with empathy and clarity to distressed parents is a core competency that differentiates good nurses from great ones and is highly sought after by employers.
---
Job Outlook and Career Growth

For anyone considering this demanding career, the long-term prospects are exceptionally bright. The demand for skilled neonatal nurses is strong and projected to grow, ensuring robust job security and ample opportunities for professional advancement for the foreseeable future.
### Strong Job Growth Projections
The U.S. Bureau of Labor Statistics (BLS) projects that employment for Registered Nurses (
