For those with an unyielding ambition to mend the human body, a steady hand, and an intellect capable of navigating one of the most complex structures in anatomy, the career of a back surgeon represents a pinnacle of medical achievement. It’s a profession defined by profound impact—giving patients a second chance at a life free from debilitating pain and immobility. But alongside this immense responsibility comes one of the most lucrative compensation packages in the entire field of medicine. The path is extraordinarily long and demanding, but the rewards, both professional and financial, are equally immense. The average back surgeon salary isn't just a number; it's a reflection of over a decade of intense training, unparalleled expertise, and the daily pressure of holding a person's quality of life in your hands.
I still remember the hushed, anxious conversations in the hospital waiting room when a close family member was undergoing complex spinal fusion surgery. The surgeon, calm and confident, was more than just a doctor; he was a beacon of hope. Witnessing the transformation from agonizing pain to gradual, steady recovery instilled in me a profound respect for the skill and dedication this career demands. This guide is for anyone who feels that same pull—the desire to master this intricate field. It will demystify the numbers, illuminate the arduous but achievable path, and provide a comprehensive, data-backed look at what it truly means—and what it pays—to be a back surgeon.
### Table of Contents
- [What Does a Back Surgeon Actually Do?](#what-does-a-back-surgeon-actually-do)
- [Average Back Surgeon Salary: A Deep Dive](#average-back-surgeon-salary-a-deep-dive)
- [Key Factors That Influence a Back Surgeon's Salary](#key-factors-that-influence-a-back-surgeons-salary)
- [Job Outlook and the Future of Spine Surgery](#job-outlook-and-the-future-of-spine-surgery)
- [How to Become a Back Surgeon: The 15-Year-Plus Roadmap](#how-to-become-a-back-surgeon-the-15-year-plus-roadmap)
- [Is the Demanding Path Worth the Reward?](#is-the-demanding-path-worth-the-reward)
What Does a Back Surgeon Actually Do?

The term "back surgeon" is a colloquialism for a highly specialized physician who has completed either an orthopedic surgery or neurosurgery residency, followed by advanced fellowship training in spine surgery. This dual-pathway is critical to understand:
- Orthopedic Spine Surgeons: These surgeons come from an orthopedic background, which focuses on the musculoskeletal system (bones, joints, ligaments, tendons). They manage a wide range of spinal issues, from degenerative conditions and herniated discs to complex spinal deformities like scoliosis and kyphosis.
- Neurosurgical Spine Surgeons: These surgeons complete a neurosurgery residency, focusing on the central and peripheral nervous system (brain, spinal cord, nerves). While they also treat degenerative conditions and trauma, they have specific expertise in procedures involving the spinal cord and nerves themselves, such as tumor removal from within the spinal cord.
In practice, the skills of both specialties overlap significantly, and they often perform many of the same procedures. The choice of surgeon can depend on the specific condition, hospital affiliation, and patient preference.
Regardless of their initial training path, the core responsibilities of a spine surgeon are multifaceted and extend far beyond the operating room. Their work is a delicate balance of diagnostics, patient education, non-surgical management, and, when necessary, performing some of the most intricate procedures in medicine.
Core Responsibilities and Daily Tasks:
- Patient Consultation and Diagnosis: This is the foundation of their work. Surgeons meet with patients to understand their history of pain, weakness, or numbness. They conduct physical examinations to assess nerve function, reflexes, and range of motion.
- Interpreting Medical Imaging: Spine surgeons are experts at reading and interpreting complex imaging studies like X-rays, Computed Tomography (CT) scans, and Magnetic Resonance Imaging (MRI) scans to pinpoint the anatomical cause of a patient's symptoms.
- Developing Treatment Plans: Surgery is often the last resort. A significant part of the job involves recommending and overseeing conservative treatments first, including physical therapy, pain management injections, and medication.
- Surgical Planning: When surgery is necessary, the surgeon meticulously plans the procedure. This involves choosing the right approach (e.g., anterior, posterior, lateral), selecting the appropriate implants (screws, rods, cages), and using sophisticated software to model the surgery for complex deformity cases.
- Performing Surgery: This is the most visible part of the job. Common procedures include:
- Discectomy: Removing a herniated portion of a disc that is pressing on a nerve.
- Laminectomy: Removing a small portion of a vertebra (the lamina) to relieve pressure on the spinal cord or nerves (spinal stenosis).
- Spinal Fusion: Fusing two or more vertebrae together with bone grafts and instrumentation (screws and rods) to eliminate painful motion or stabilize the spine.
- Artificial Disc Replacement: Replacing a damaged degenerative disc with a prosthetic implant designed to preserve motion.
- Deformity Correction: Complex, hours-long surgeries to correct severe curvatures of the spine like scoliosis.
- Post-Operative Care: The surgeon's responsibility doesn't end when the patient leaves the O.R. They closely monitor patients' recovery in the hospital and through follow-up clinic appointments for months or even years.
- Administrative and Academic Work: Many surgeons are also involved in research to advance the field, teaching medical students and residents, and handling the administrative duties of running a practice.
### A Day in the Life: Clinic Day vs. O.R. Day
To make this more tangible, a spine surgeon's week is often split into distinct types of days.
A Typical Clinic Day:
- 7:30 AM: Arrive at the office, review the day's patient list and their corresponding imaging studies with a physician assistant (PA) or nurse practitioner (NP).
- 8:00 AM - 12:00 PM: See patients in 15-20 minute intervals. This is a rapid-fire mix of new patient consultations, post-operative follow-ups, and pre-operative appointments to finalize surgical plans. For every new patient, the surgeon must quickly build rapport, perform a focused exam, review complex MRIs, and clearly explain a diagnosis and treatment options.
- 12:00 PM - 1:00 PM: A hurried lunch, often while reviewing more scans, answering emails, and returning urgent calls from the hospital.
- 1:00 PM - 5:00 PM: The afternoon session continues. The surgeon might see a 6-week post-op patient who is doing fantastic, followed immediately by a complex case with a long history of failed treatments, requiring a difficult conversation about the high risks of a revision surgery.
- 5:00 PM - 7:00 PM+: "Clinic" is over, but the work isn't. This time is dedicated to dictating patient notes, reviewing all the imaging from the day in detail, responding to non-urgent messages, and preparing for the next day's surgeries.
A Typical O.R. Day:
- 6:30 AM: Arrive at the hospital, change into scrubs. Meet with the anesthesiologist and the surgical team to review the day's cases, confirming patient details, surgical plans, and any potential challenges.
- 7:00 AM: Meet the first patient in the pre-op area, provide reassurance, answer last-minute questions, and mark the surgical site.
- 7:30 AM - 11:00 AM: Case 1: Lumbar Discectomy. A relatively straightforward, one-hour procedure. The surgeon makes a small incision, carefully dissects through muscle, and uses a microscope to remove the disc fragment pressing on a nerve root.
- 11:00 AM - 11:30 AM: Speak with the patient's family, dictate the operative note, and prepare for the next case while the O.R. team "turns over" the room.
- 11:30 AM - 4:30 PM: Case 2: Two-Level Posterior Lumbar Fusion. A much more complex and lengthy surgery. This involves placing multiple pedicle screws, removing degenerative discs, inserting cages into the disc space, and securing rods to create a rigid, stable construct. This requires intense focus, physical stamina, and precision.
- 4:30 PM - 6:00 PM: The surgery is complete. The surgeon dictates the extensive operative note, writes post-operative orders, and checks on the patient in the recovery room.
- 6:00 PM+: Before heading home, they will often "round" on any other inpatients, checking their progress and making adjustments to their care plans. The day often ends late, filled with both physical and mental exhaustion.
This dual rhythm of intense clinical problem-solving and technically demanding surgery defines the profession. It requires a unique blend of intellectual rigor, technical mastery, physical endurance, and deep-seated empathy.
Average Back Surgeon Salary: A Deep Dive
The compensation for a spine surgeon is among the highest in any profession, a direct reflection of the extensive training, high-stakes nature of the work, and the significant revenue they generate for hospitals and practices. While figures vary, spine surgeons consistently rank in the top tier of physician earners.
It is crucial to note that salary data for such a specific sub-specialty is often blended within broader categories like "Orthopedic Surgery" or "Neurosurgery" in government statistics. Therefore, the most accurate data comes from physician-specific compensation surveys from organizations like Medscape, Doximity, and Merritt Hawkins.
National Averages and Salary Ranges
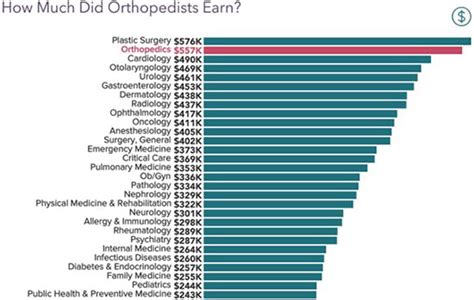
According to the 2023 Medscape Physician Compensation Report, which surveys thousands of physicians across the United States, the specialties that lead to a career as a back surgeon are at the top of the earnings list:
- Orthopedics: Average annual compensation of $573,000.
- Neurosurgery: While not always broken out separately, it's widely recognized to be even higher, often cited as the #1 or #2 highest-paid specialty.
However, these are averages for the entire specialty. Surgeons who sub-specialize in the spine typically earn significantly more. Data from multiple sources, including physician recruiting firm reports and specialized salary aggregators, place the average spine surgeon salary much higher.
- Overall Average Spine Surgeon Salary: $849,000 - $985,000+ per year.
- Typical Salary Range: A newly minted spine surgeon starting out might earn between $450,000 and $650,000 in their first couple of years. A highly experienced surgeon in a productive private practice can easily exceed $1,500,000 to $2,000,000 annually.
As reported by Salary.com (as of late 2023), the median salary for a "Spine Surgeon" in the United States is $785,714, with a typical range falling between $515,699 and $1,085,255. This wide range highlights the significant impact of the factors we will discuss in the next section.
### Salary by Experience Level
The salary trajectory for a spine surgeon is not a gradual climb; it's a steep ascent after completing their fellowship, followed by continued strong growth as they build their practice and reputation.
| Career Stage | Years of Experience (Post-Fellowship) | Typical Annual Salary Range | Key Notes |
| :--- | :--- | :--- | :--- |
| Early Career | 0 - 5 Years | $450,000 - $750,000 | Often starts with a guaranteed salary for the first 1-2 years before transitioning to a productivity-based model. Focus is on building a patient base. |
| Mid-Career | 6 - 15 Years | $750,000 - $1,200,000+ | Reputation is established, referral patterns are strong. Surgeon is highly efficient in the O.R. and clinic. May be taking on leadership roles. |
| Senior/Late Career | 16+ Years | $900,000 - $2,000,000+ | Peak earning years. Often a partner in a private practice with significant ownership equity. May slow down clinically but have high income from ancillary services. |
*Sources: Data compiled and synthesized from Medscape, Doximity, Merritt Hawkins reports, and Salary.com (2023-2024).*
### Deconstructing the Compensation Package
A spine surgeon's income is rarely just a flat salary. The total compensation package is a complex mix of components designed to incentivize productivity and align the surgeon's goals with the practice or hospital.
- Base Salary: This is the guaranteed portion of the surgeon's income. In the early years, especially in a hospital-employed model, this might be the largest component. Private practices may offer a lower base salary, with a much higher potential for bonuses.
- Productivity Bonus (RVU-Based): This is the most significant driver of income for most established surgeons. Compensation is tied to Relative Value Units (RVUs), a standardized measure used by Medicare to value the work involved in a physician's service. Every procedure, clinic visit, and test interpretation is assigned an RVU value. Surgeons are often paid a certain dollar amount per RVU generated above a certain threshold. A complex spinal fusion can generate a high number of RVUs, directly rewarding surgeons who perform more intricate and time-consuming procedures.
- Sign-On Bonus: To attract top talent out of fellowship, practices and hospitals offer substantial sign-on bonuses, often ranging from $50,000 to $150,000 or more.
- Call Pay: Surgeons are paid a stipend for being "on call" for hospital emergencies (e.g., spinal trauma from a car accident). This can be a significant income source, often paid per diem or as an annual stipend.
- Profit Sharing / Partnership Equity: This is the primary driver of the highest incomes and is typically available only in private practice. After a few years, a surgeon may be offered the chance to "buy in" to the practice, becoming a partner. As a partner, they share in the overall profits of the group, which can include revenue from ancillary services like physical therapy, imaging (MRI), and ambulatory surgery centers (ASCs).
- Other Benefits: The package is rounded out by a comprehensive benefits suite, which is critically important given the nature of the job:
- Malpractice Insurance: Absolutely essential, with annual premiums that can exceed $100,000, typically paid for by the employer.
- Health, Dental, and Vision Insurance.
- Generous Retirement Plans: 401(k) with employer matching, and sometimes pension or profit-sharing plans.
- Continuing Medical Education (CME) Allowance: Funds to attend conferences and courses to stay up-to-date.
- Relocation Assistance.
Understanding this structure is key. A surgeon considering two job offers—one with a $650,000 guaranteed salary and another with a $450,000 base plus a favorable RVU bonus structure—must carefully calculate their potential earnings based on their expected surgical volume. The latter often provides a much higher long-term ceiling.
Key Factors That Influence a Back Surgeon's Salary
While the baseline salary for a spine surgeon is exceptionally high, the difference between earning $600,000 and $2,000,000 per year is determined by a confluence of critical factors. Aspiring surgeons and those in their early careers must understand these variables to strategically guide their training and career choices.
###
1. Practice Setting: The Single Biggest Influencer
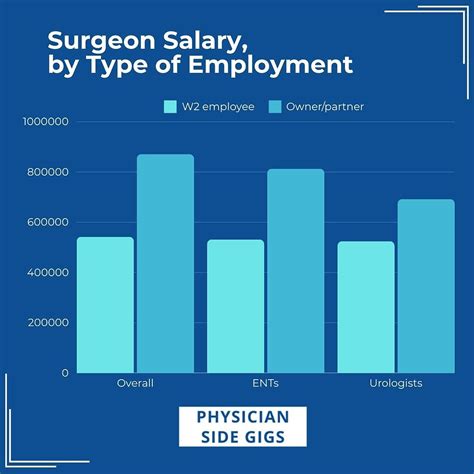
Where a surgeon chooses to work is arguably the most dominant factor in determining their earning potential and work-life balance.
- Private Practice (Single-Specialty or Multi-Specialty Group):
- Earning Potential: Highest. This setting offers a direct path to partnership and a share in the practice's total profits. Successful partners in established orthopedic or neurosurgery groups are the top earners in the field.
- Why? In addition to their own surgical productivity, partners earn from the group's "ancillary services." If the practice owns its own MRI scanner, physical therapy center, or, most lucratively, an Ambulatory Surgery Center (ASC), the partners share in the revenue generated by these profitable ventures. This can add hundreds of thousands of dollars to their annual income.
- The Trade-off: This model comes with the responsibilities of a business owner. Surgeons must participate in administrative decisions, manage staff, worry about overhead costs (rent, salaries, insurance), and handle the complexities of billing and collections. The financial risk is higher, but so is the reward.
- Hospital or Health System Employment:
- Earning Potential: Moderate to High. This is an increasingly common model. The surgeon is a direct employee of the hospital.
- Why? This model offers stability and predictability. Hospitals typically provide a competitive, guaranteed base salary plus a productivity bonus. They handle all administrative overhead, billing, staffing, and malpractice insurance, allowing the surgeon to focus purely on clinical medicine.
- The Trade-off: The ultimate income ceiling is lower than in private practice because the surgeon does not share in ancillary revenue. The hospital keeps that profit. There is also less autonomy; surgeons may be subject to hospital policies, required to use specific implants, and have less control over their schedules and staff.
- Academic Medical Center:
- Earning Potential: Lowest. Surgeons at university hospitals and academic centers are on the lower end of the spine surgeon pay scale.
- Why? Compensation is often traded for other benefits. The core mission is tripartite: clinical care, research, and education. A significant portion of the surgeon's time is dedicated to teaching medical students and residents and conducting research, which does not generate the same revenue as performing surgery.
- The Trade-off and Benefits: While the pay is lower, these positions offer immense prestige, the opportunity to work on cutting-edge and complex cases, dedicated research support, and the deep satisfaction of training the next generation of surgeons. For those passionate about advancing the science of spine surgery, this is the ideal environment.
###
2. Geographic Location: The Laws of Supply and Demand
Where a practice is located has a profound impact on salary, often in ways that seem counterintuitive. It's not always the major coastal cities that pay the most.
- Highest Paying Regions: According to the 2023 Doximity Physician Compensation Report, the metropolitan areas with the highest average physician compensation are often in the Midwest and Southeast. States like Wisconsin, Indiana, Georgia, and the Carolinas frequently appear at the top.
- Why? It's a classic case of supply and demand. These regions may be perceived as less "desirable" to live in than, say, San Francisco or New York City. To attract a scarce resource—a fellowship-trained spine surgeon—hospitals and practices in these areas must offer significantly higher compensation packages. A lower cost of living in these areas further amplifies the take-home pay.
- Lower Paying Regions: Major metropolitan areas in the Northeast and on the West Coast (e.g., Boston, NYC, Los Angeles, San Francisco) often have lower average physician salaries.
- Why? These areas have a high density of academic medical centers and are highly desirable places to live, resulting in a surplus of surgeons competing for positions. With more supply, practices don't need to offer top-tier salaries to attract talent. Furthermore, these regions often have higher overhead costs and less favorable reimbursement rates from insurance payers.
Example Salary Variation by Metro Area (Illustrative):
| Metro Area | Relative Compensation Level | Estimated Average Salary | Rationale |
| :--- | :--- | :--- | :--- |
| Charlotte, NC | High | ~$1,100,000 | High demand, large health systems, favorable payer mix. |
| Milwaukee, WI | High | ~$1,050,000 | Strong private practice market, need to attract talent to the region. |
| Dallas, TX | High | ~$980,000 | Pro-business environment, large population, competitive hospital systems. |
| San Francisco, CA | Moderate | ~$850,000 | High desirability, saturated market, very high cost of living. |
| Boston, MA | Lower | ~$790,000 | Dominated by academic centers, high physician density. |
*Data synthesized from market analysis and reports like Doximity and Merritt Hawkins.*
###
3. Initial Training Pathway: Neurosurgery vs. Orthopedic Surgery
While both paths lead to becoming a spine surgeon, the initial residency training can influence earning potential, particularly early in a surgeon's career.
- Neurosurgery: Neurosurgeons consistently rank at or near the very top of all physician specialties for compensation. This is partly due to the length and rigor of their training (7 years of residency) and their unique ability to operate on intradural pathologies (inside the lining of the spinal cord), such as spinal cord tumors. This can lead to a case mix that includes highly complex, well-reimbursed procedures.
- Orthopedic Surgery: While also a top-earning specialty, the overall average for orthopedics is slightly below neurosurgery. However, an orthopedic surgeon who completes a spine fellowship and focuses on complex cases, particularly adult deformity, can easily match or even exceed the income of a neurosurgeon.
Ultimately, once a surgeon is established, their income is driven more by their practice setting, surgical volume, and case complexity than by their original residency training.
###
4. Sub-Specialization and Case Mix
Not all spine surgery is the same. A surgeon's focus within the field can dramatically affect their productivity and, consequently, their income.
- Complex Deformity and Revision Surgery: Surgeons who specialize in correcting severe scoliosis, kyphosis, or fixing previously failed surgeries perform some of the longest and most technically demanding procedures. These cases generate very high RVUs and are reimbursed at a high rate, leading to greater income. However, they also carry the highest risk and stress levels.
- Minimally Invasive Surgery (MIS): Surgeons who are experts in MIS techniques are in high demand. These procedures often allow for faster patient recovery and can be performed in an outpatient setting (like an ASC), which can be very profitable for a private practice.
- "Bread and Butter" Spine Surgery: A practice focused primarily on more routine, albeit still complex, procedures like lumbar discectomies and single-level fusions will have a high volume. While each case is reimbursed less than a major deformity surgery, the sheer number of cases can lead to a very high income.
A surgeon's "payer mix" is also critical. A practice that sees a high percentage of patients with private insurance or worker's compensation plans will have much higher revenue than a practice that primarily sees patients with lower-reimbursing Medicare or Medicaid plans.
###
5. Years of Experience and Reputation
As detailed in the salary table, experience is a powerful driver of income, but it's not just about time served. It's about the reputation built over that time.
- Early Career (Years 1-5): The focus is on building a practice. Surgeons work to establish relationships with referring physicians (primary care doctors, physiatrists, chiropractors) in the community. They must demonstrate excellent clinical judgment and surgical outcomes to earn trust and a steady stream of patients.
- Mid-Career to Senior Career (Years 6+): A surgeon with a stellar reputation becomes a regional resource. They receive the most complex and challenging referral cases from other doctors. This reputation directly translates into higher surgical volume, a more complex case mix, and, therefore, higher compensation. This is when surgeons often become senior partners in their groups, maximizing their income through both clinical work and practice ownership.
Job Outlook and the Future of Spine Surgery

For those willing to undertake the arduous training, the career outlook for spine surgeons is exceptionally strong and stable. The demand for their specialized skills is projected to grow steadily, driven by powerful demographic and technological trends.
Official Projections and Data
The U.S. Bureau of Labor Statistics (BLS) projects the overall employment for "Physicians and Surgeons" to grow by 3 percent from 2022 to 2032, which is about as fast as the average for all occupations. This will result in about 24,000 openings each year, on average, over the decade, primarily due to the need to replace workers who retire or exit the occupation.
However, this broad statistic doesn't capture the full picture for a high-demand sub-specialty like spine surgery. The true drivers of demand are more specific:
1. The Aging of the Global Population: This is the single most significant tailwind for the profession. As the massive Baby Boomer generation ages, the incidence of degenerative spine conditions—such as spinal stenosis, degenerative disc disease, and spondylolisthesis—is increasing dramatically. These are the primary conditions treated by spine surgeons. This demographic shift creates a constantly expanding pool of potential patients, ensuring a high demand for spine care for decades to come.
2. Technological Advancements and Innovation: The field of spine surgery is in a constant state of evolution. These advancements not only improve patient outcomes but also expand the range of conditions that can be treated surgically, further fueling demand. Key trends include:
- Robotics and Surgical Navigation: Robotic-assisted systems (like Mazor X or Globus ExcelsiusGPS) and advanced navigation platforms allow for more precise placement of spinal instrumentation (screws and rods), potentially reducing complication rates and improving outcomes. Surgeons skilled in these technologies are highly sought after.
- **Minimally
