Table of Contents

- [Introduction](#introduction)
- [What Does a Bariatric Surgeon Do?](#what-does-a-bariatric-surgeon-do)
- [Average Bariatric Surgeon Salary: A Deep Dive](#average-bariatric-surgeon-salary-a-deep-dive)
- [Key Factors That Influence a Bariatric Surgeon's Salary](#key-factors-that-influence-a-bariatric-surgeons-salary)
- [Job Outlook and Career Growth for Bariatric Surgeons](#job-outlook-and-career-growth-for-bariatric-surgeons)
- [How to Become a Bariatric Surgeon: Your Step-by-Step Guide](#how-to-become-a-bariatric-surgeon-your-step-by-step-guide)
- [Conclusion: Is a Career as a Bariatric Surgeon Worth It?](#conclusion-is-a-career-as-a-bariatric-surgeon-worth-it)
---
Introduction

Embarking on a career in medicine is a monumental decision, a commitment of time, intellect, and spirit. For those drawn to the intricate and life-altering field of surgery, choosing a specialty is the next critical juncture. If you're captivated by the prospect of performing procedures that not only address a specific ailment but fundamentally transform a patient's entire life, then the path of a bariatric surgeon might be your calling. This role is a unique fusion of advanced surgical skill, long-term patient care, and profound human impact.
Financially, the profession is among the most rewarding in any industry. A bariatric surgeon's salary reflects the extensive training, high-stakes responsibility, and specialized expertise required. On average, you can expect to earn a compensation package well into the six-figure range, often between $400,000 and $700,000 annually, with top earners in high-demand areas or private practice exceeding this significantly.
As a career analyst, I once had the privilege of interviewing a patient six months after her gastric sleeve surgery for a healthcare impact report. She spoke not just of the weight she'd lost, but of the life she'd gained—the ability to play with her children, the reversal of her type 2 diabetes, the newfound confidence that radiated from her. In that moment, the surgeon's role was crystallized for me; they are not just technicians of the body, but architects of a second chance at life. This guide is for those who aspire to be that architect. We will dissect every facet of a bariatric surgeon's career, from the granular details of their compensation to the long and demanding road it takes to get there.
---
What Does a Bariatric Surgeon Do?
A bariatric surgeon, also known as a metabolic surgeon, is a highly specialized general surgeon who focuses on surgical procedures to treat obesity and related metabolic diseases like type 2 diabetes, high blood pressure, and sleep apnea. Their work extends far beyond the operating room, encompassing a comprehensive, long-term commitment to their patients' health journey.
The core of their role involves performing weight-loss surgeries, most commonly:
- Sleeve Gastrectomy: A procedure where a large portion of the stomach is removed, leaving a smaller, banana-shaped "sleeve." This restricts food intake and influences gut hormones that affect hunger and satiety.
- Roux-en-Y Gastric Bypass: This procedure involves creating a small stomach pouch and rerouting a section of the small intestine to connect to it. This both restricts food intake and reduces the absorption of calories and nutrients.
- Adjustable Gastric Band: A silicone band is placed around the upper part of the stomach to create a small pouch, restricting food intake. This procedure is less common today.
- Biliopancreatic Diversion with Duodenal Switch (BPD/DS): A more complex procedure that involves a sleeve gastrectomy combined with a significant intestinal bypass, leading to high levels of malabsorption and weight loss.
- Revisional Surgery: Correcting or modifying previous weight-loss surgeries that may have led to complications or insufficient results.
However, the responsibilities of a bariatric surgeon are multidisciplinary and patient-centric. Their work is a blend of clinical consultation, surgical intervention, and postoperative management.
Typical Responsibilities and Daily Tasks:
- Patient Consultations: Conducting initial evaluations of potential surgical candidates to assess their medical history, psychological readiness, and understanding of the lifelong commitment required.
- Pre-Operative Planning: Collaborating with a multidisciplinary team, including dietitians, psychologists, cardiologists, and endocrinologists, to ensure a patient is fully optimized for surgery.
- Surgical Performance: Executing complex laparoscopic or robotic-assisted bariatric procedures with precision and care. This requires exceptional hand-eye coordination, spatial reasoning, and the ability to remain calm under immense pressure.
- Post-Operative Care: Managing patients immediately after surgery in the hospital, monitoring for complications like leaks, bleeding, or blood clots.
- Long-Term Follow-Up: Seeing patients for years after their surgery to monitor their weight loss, nutritional status, and resolution of comorbidities. This is a key differentiator from many other surgical specialties.
- Administrative & Academic Work: For those in private practice, this includes business management. For those in academic centers, it involves teaching residents and medical students, conducting research, and publishing findings.
### A Day in the Life of a Bariatric Surgeon
To make this tangible, a surgeon's week is often split between operating days and clinic days.
A Typical OR (Operating Room) Day:
- 6:30 AM: Arrive at the hospital, review the day's surgical list, and check on post-operative patients from the previous day (rounding).
- 7:30 AM: First surgery begins. The surgeon meets with the patient and their family one last time, then scrubs in. A sleeve gastrectomy might take 60-90 minutes.
- 9:30 AM: Between cases, the surgeon dictates operative notes, calls the family of the first patient with an update, and briefly confers with the anesthesiologist about the next case.
- 10:00 AM: The second surgery, perhaps a more complex gastric bypass, begins. This could take 2-3 hours.
- 1:00 PM: A quick lunch while reviewing patient charts and answering urgent pages from the hospital floor.
- 2:00 PM: The final scheduled surgery of the day, another sleeve gastrectomy.
- 4:00 PM: After the last case, the surgeon completes all paperwork, checks on the newly post-operative patients, and does a final round on other inpatients.
- 6:00 PM: Leave the hospital, but remain on call for any emergencies.
A Typical Clinic Day:
- 8:00 AM: Clinic begins. The first several appointments are new patient consultations, each lasting 30-45 minutes.
- 10:30 AM: A series of post-operative follow-up appointments. These can range from 2-week check-ins to 5-year annual visits.
- 12:30 PM: Lunch, often combined with a team meeting with the program's dietitian and psychologist to discuss complex patient cases.
- 1:30 PM: More follow-up appointments, reviewing lab work, adjusting vitamin regimens, and providing encouragement or addressing challenges.
- 4:00 PM: Time blocked for administrative tasks: reviewing patient referrals, responding to emails, and signing off on charts.
- 5:30 PM: Clinic day ends.
This dual structure highlights that a bariatric surgeon must be both a masterful technician in the OR and an empathetic, long-term guide in the clinic.
---
Average Bariatric Surgeon Salary: A Deep Dive
The financial compensation for a bariatric surgeon is substantial, commensurate with over a decade of post-secondary education and training, the high-stakes nature of their work, and the significant positive economic impact they have on the healthcare system by resolving costly chronic diseases.
Salary data can vary based on the source, reporting methodology (self-reported vs. employer-reported), and the components included (base salary vs. total compensation). To provide a comprehensive picture, we'll examine data from several authoritative sources.
National Averages and Ranges
- Medscape's 2023 Physician Compensation Report, a highly respected industry benchmark, places the average salary for general surgeons (the category under which bariatrics falls) at $412,000. However, specialists often earn more than the general category average. Bariatrics is one of the more procedurally intensive and thus higher-earning subspecialties.
- Salary.com provides more specific data, reporting the median salary for a Bariatric Surgeon in the United States as $462,912 as of late 2023. Their data typically shows a range from $391,339 to $545,862.
- Doximity's 2023 Physician Compensation Report indicates that surgical specialists, on average, earn significantly more than primary care physicians. While it doesn't break out bariatric surgery specifically, top surgical specialties like neurosurgery and thoracic surgery top the list, with general surgery being very well-compensated. Bariatric surgeons in busy practices often approach the compensation levels of higher-end surgical specialties.
- Payscale reports a slightly lower average base salary around $355,000, but this may not fully capture bonuses and incentives. They show a total pay range from $203,000 to $594,000+.
Synthesizing this data, a realistic expectation for a bariatric surgeon's total annual compensation is:
- Median National Salary: Approximately $450,000 - $500,000
- Typical Salary Range: $375,000 (for those starting out or in lower-paying academic roles) to $750,000+ (for experienced surgeons in productive private practices or high-demand regions).
### Salary by Experience Level
Like any profession, compensation grows significantly with experience, reputation, and efficiency. In surgery, experience leads to faster operative times, lower complication rates, and a stronger referral network, all of which drive income.
| Career Stage | Years of Experience | Typical Annual Compensation Range | Notes |
| :--- | :--- | :--- | :--- |
| Entry-Level | 0-3 years post-fellowship | $350,000 - $450,000 | Often starts with a guaranteed salary for the first 1-2 years while building a practice. May have a lower initial bonus structure. |
| Mid-Career | 4-10 years post-fellowship| $450,000 - $650,000 | Transitioned to a productivity-based model. Has an established reputation and steady stream of patient referrals. |
| Senior/Late-Career| 11+ years post-fellowship| $600,000 - $800,000+ | Highly efficient in the OR, performing a high volume of cases. May hold leadership roles (e.g., Medical Director) and have ownership in a private practice or surgery center. |
*Source: Analysis synthesized from Salary.com, Medscape, and industry recruitment data.*
### Deconstructing the Compensation Package
A bariatric surgeon's salary is rarely just a flat number. It's a package composed of several key elements:
1. Base Salary: This is the guaranteed portion of pay. In hospital-employed settings, this might make up the majority of the income initially. In private practice, it may be a more modest figure, with the bulk of earnings coming from productivity.
2. Productivity Bonuses (RVU-Based Compensation): This is the most significant variable component for most surgeons. Compensation is tied to the volume and complexity of the work they do, measured in Relative Value Units (RVUs). Every medical procedure is assigned an RVU value by Medicare. The surgeon earns a negotiated dollar amount per RVU generated, often after meeting a certain threshold. A high-volume bariatric surgeon can generate a massive number of RVUs, leading to very high income potential. For example:
- A laparoscopic sleeve gastrectomy might be worth ~22 RVUs.
- A laparoscopic gastric bypass might be worth ~30 RVUs.
- At a rate of $60 per RVU, a single gastric bypass could contribute $1,800 to the surgeon's productivity bonus.
3. Performance & Quality Bonuses: Many hospital systems and large groups are moving towards value-based care. Surgeons may receive bonuses tied to quality metrics such as:
- Low complication rates
- Low readmission rates
- Positive patient satisfaction scores
- Achieving program accreditation (e.g., from the MBSAQIP)
4. On-Call Pay: Surgeons are often paid a stipend for being on call for the emergency department or for the practice, typically calculated as a per diem (daily) rate.
5. Sign-On Bonus: To attract top talent, especially in underserved areas, hospitals and practices often offer substantial sign-on bonuses, which can range from $25,000 to $100,000+.
6. Other Benefits and Perks:
- Health, Dental, and Vision Insurance: Comprehensive plans for the surgeon and their family.
- Retirement Plans: Access to 401(k) or 403(b) plans, often with a generous employer match.
- Malpractice Insurance: Fully paid "claims-made" or "occurrence" policies. The latter is more valuable as it covers incidents indefinitely, even after the surgeon leaves the practice.
- Continuing Medical Education (CME) Allowance: An annual stipend ($5,000 - $15,000) to cover costs for conferences, journals, and maintaining licensure.
- Relocation Assistance: A one-time payment to help with the cost of moving.
- Loan Repayment Assistance: Some positions, particularly in non-profit or rural settings, offer assistance in paying down student loan debt, which can be a significant financial benefit given the high cost of medical education.
Understanding this complete picture is crucial. A job offer with a lower base salary but a highly achievable productivity bonus and excellent benefits might be far more lucrative than one with a high base salary alone.
---
Key Factors That Influence a Bariatric Surgeon's Salary
The wide salary ranges presented above are not arbitrary. A surgeon's earning potential is a complex equation influenced by a multitude of professional and environmental factors. For anyone aspiring to this career, understanding these levers is key to maximizing long-term financial success.
###
Level of Education and Advanced Training
The educational journey is the non-negotiable foundation of a surgeon's career, and each stage is a prerequisite for the next. While the base degrees (MD or DO) are universal, the specialized training is what unlocks the high earning potential.
1. Undergraduate Degree (4 years): No direct impact on salary, but a strong academic record in a pre-med track is essential for medical school admission.
2. Medical School (4 years): Earning a Doctor of Medicine (MD) or Doctor of Osteopathic Medicine (DO) degree. Again, this is a baseline requirement.
3. General Surgery Residency (5-7 years): This is where the core surgical skills are developed. A surgeon's salary as a resident is modest, typically ranging from $60,000 to $80,000 annually, set by the institution.
4. Bariatric Surgery Fellowship (1-2 years): This is the single most important educational step for salary potential. Completing a fellowship accredited by the Fellowship Council signifies the highest level of specialized training. Surgeons who are "fellowship-trained" are far more marketable and command significantly higher starting salaries than a general surgeon who performs bariatric procedures occasionally. This training provides expertise in advanced laparoscopic and robotic techniques, management of complex cases, and revisional surgery.
5. Board Certification: After residency, surgeons must become board-certified by the American Board of Surgery (ABS). While not technically "education," maintaining this certification through continuous learning is critical. Lack of board certification would be a major red flag and severely limit employment and salary prospects.
6. Robotic Surgery Training: Proficiency with robotic platforms like the da Vinci Surgical System is increasingly becoming a desired skill. Surgeons with extensive robotic experience may be more attractive to well-equipped, modern hospitals and can sometimes negotiate for higher compensation or have access to a case mix that generates more RVUs.
###
Years of Experience
Experience is arguably the most powerful driver of salary growth after the initial training period. This is not simply about longevity; it's about the tangible benefits that experience brings.
- Early Career (0-3 Years): As mentioned, surgeons often start on a guaranteed salary. Their focus is on building a patient base, honing their surgical skills, and becoming efficient in the operating room. Their RVU production is typically lower as they ramp up. Salary: $350,000 - $450,000.
- Mid-Career (4-10 Years): By this stage, the surgeon has an established reputation in the community. Primary care physicians know to refer patients to them. They have likely transitioned to a full productivity-based compensation model. They are faster in the OR, handle more complex cases, and have lower complication rates, all of which boost their RVU generation. Salary: $450,000 - $650,000.
- Senior/Peak Career (11+ Years): These are the masters of their craft. They are often the go-to surgeons for the most challenging revisional cases. Their efficiency allows them to handle a high volume of surgeries. They may also take on lucrative leadership roles, such as the Medical Director of a Bariatric Surgery Center of Excellence, which comes with an additional stipend. If in private practice, they are likely senior partners with significant equity. Salary: $600,000 - $800,000+, with the ceiling being very high for practice owners.
###
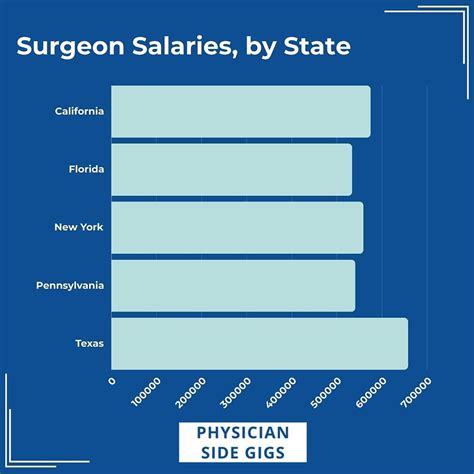
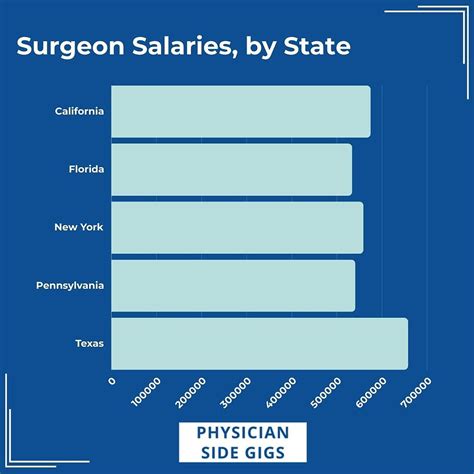
Geographic Location
"Location, location, location" is as true for surgeon salaries as it is for real estate. Compensation varies dramatically by state, region, and even between urban and rural settings. This is driven by local market demand, cost of living, and, most importantly, the reimbursement rates from private insurers and Medicare/Medicaid in that area.
High-Paying States/Regions:
Data from various physician compensation reports consistently points to certain areas as being more lucrative. These are often in the Midwest, Southeast, and non-coastal West, where demand may outstrip the supply of specialists.
- Top-Tier States: States like Alabama, Kentucky, Oklahoma, Indiana, and Missouri often appear in the top 10 for physician compensation. A bariatric surgeon in these states could potentially earn 10-20% above the national average.
- Example: A surgeon in Indianapolis might earn $550,000, while a surgeon with a similar practice in Boston might earn $475,000.
Lower-Paying States/Regions:
Conversely, areas with a high concentration of surgeons, numerous academic medical centers, and lower insurance reimbursement rates tend to have lower salaries. These are often in the Northeast and parts of the West Coast.
- Lower-Tier States: States like Maryland, Massachusetts, New York, and California often report salaries closer to or slightly below the national median.
- The Urban vs. Rural Dynamic: While major metropolitan areas have a high volume of patients, they also have more competition. A surgeon in a rural or underserved community might be the only bariatric specialist for hundreds of miles. To attract them, local hospitals often offer very high guaranteed salaries, loan repayment, and sign-on bonuses. This can make a rural position one of the most financially attractive options, especially early in a career.
###
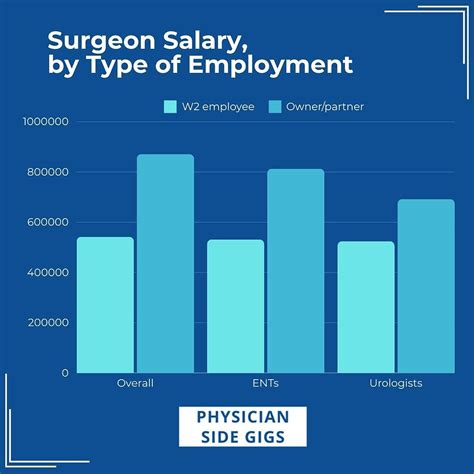
Practice Type & Size
The setting in which a surgeon works is a fundamental determinant of their compensation structure and earning potential.
- Private Practice (Solo or Small Group): This model offers the highest income potential. The surgeons are business owners. They collect revenue directly from insurers and patients and, after paying overhead (staff, rent, malpractice, etc.), the remaining profit is their income. A successful private practice bariatric surgeon can easily earn over $750,000 or even $1,000,000 annually. However, this comes with the greatest risk and administrative burden. They are responsible for marketing, billing, hiring, and all other aspects of running a business.
- Hospital or Health System Employment: This is the most common model today. The surgeon is an employee of the hospital. This provides greater stability, predictable income, and excellent benefits. The hospital handles all administrative overhead. The trade-off is a lower ceiling on income. Compensation is typically a base salary plus a productivity bonus, but the dollar-per-RVU rate may be lower than what one could generate in private practice. This is an excellent option for those who want to focus purely on clinical medicine.
- Academic Medical Center: Surgeons at university hospitals typically have the lowest base salaries. Their compensation is balanced by other responsibilities and benefits. A significant portion of their time is dedicated to teaching medical students and residents, and conducting clinical research. While their direct pay may be lower, they often have exceptional benefits, a strong pension plan, and the prestige associated with an academic appointment. Their work-life balance may also be more structured.
- Multi-Specialty Group: Joining a large group that includes primary care, endocrinology, cardiology, and other specialties can be highly beneficial. It creates a built-in referral network, ensuring a steady stream of patients. Compensation is often similar to a hospital-employed model, combining a base salary with productivity incentives.
###
Area of Specialization (Procedural Mix)
While "bariatric surgery" is the specialty, a surgeon's specific procedural expertise can influence income.
- Complex Revisional Surgery: Surgeons who specialize in fixing or revising failed surgeries from other institutions are in high demand. These procedures are more complex, take longer, and have higher RVU values, thus generating more revenue. Building a reputation as a "go-to" for revisions can significantly boost income.
- Robotic Surgery: As mentioned, expertise in robotic surgery can be a differentiator. Hospitals that have invested millions in a robotic system need surgeons who can use it effectively. This can provide leverage in negotiations.
- Metabolic Surgery Focus: Some surgeons brand themselves specifically as "metabolic surgeons," focusing on the resolution of type 2 diabetes. While the procedures are the same, this focus can attract a specific patient population and may be a focus of academic research, enhancing a surgeon's profile.
###
In-Demand Skills (Beyond the OR)
A surgeon's value is not solely determined by their hands. A set of professional skills can directly and indirectly lead to higher compensation.
- Business Acumen: For private practitioners, understanding finance, marketing, and management is paramount to maximizing profit.
- Leadership and Administrative Skills: Taking on roles like Department Chair, Chief of Surgery, or Medical Director of a bariatric program comes with a stipend and increased influence. These roles are awarded to surgeons who demonstrate leadership, good judgment, and the ability to manage teams.
- Patient Communication & Bedside Manner: In the age of online reviews and patient satisfaction scores (which can be tied to bonuses), excellent communication skills are invaluable. A surgeon who builds trust and rapport with patients will have a better reputation, more referrals, and higher satisfaction scores.
- Research and Publication: In academia, a strong research portfolio is essential for promotion and tenure, which leads to salary increases. In any setting, being a published author or a speaker at national conferences elevates a surgeon's professional standing and can lead to more referrals and consulting opportunities.
---
Job Outlook and Career Growth for Bariatric Surgeons

For those investing the 15+ years required to enter this field, the long-term career outlook is a critical consideration. The prospects for bariatric surgeons are exceptionally strong, driven by powerful and persistent public health trends.
Projected Job Growth
The U.S. Bureau of Labor Statistics (BLS) projects employment for all physicians and surgeons to grow 3 percent from 2022 to 2032, which is about as fast as the average for all occupations. However, this general statistic doesn't fully capture the high-demand nature of specific specialties. The outlook for bariatric surgeons is significantly more robust due to one overwhelming factor: the ongoing obesity epidemic.
- According to the Centers for Disease Control and Prevention (CDC), the U.S. adult obesity prevalence was 41.9% in March 2020, with severe obesity at 9.2%. These numbers have been steadily rising for decades.
- This creates a vast and growing population of potential candidates for bariatric surgery. As the efficacy and safety of these procedures become more widely recognized, the demand for qualified surgeons is expected to increase substantially.
Therefore, while the overall number of surgeons may grow modestly, the demand within the bariatric subspecialty is poised for much more rapid expansion. Hospitals are increasingly establishing or expanding "Bariatric Centers of Excellence" as a key service line, creating a consistent stream of job openings across the country.
Emerging Trends and Future Opportunities
The field of bariatric surgery is not static. Several key trends are shaping its future and presenting new opportunities for career growth.
1. The Rise of Metabolic Surgery: There is a major paradigm shift occurring, re-branding bariatric surgery as "metabolic surgery." The focus is moving beyond simple weight loss to the powerful effect these operations have on metabolic diseases. The American Diabetes Association now includes metabolic surgery in its standards of care for certain patients with type 2 diabetes. This medical validation will continue to drive patient volumes and insurance coverage.
2. Integration with New Medical Therapies: The emergence of highly effective anti-obesity medications