Welcome to the Sunshine State—a place known not only for its beautiful beaches and vibrant culture but also for its rapidly expanding healthcare sector. If you're an analytical, detail-oriented individual looking for a stable, in-demand, and rewarding career, you may have found your calling in medical billing and coding. But what does that career actually look like in Florida? More specifically, what can you expect to earn?
This guide is designed to be your single, most authoritative resource on the topic. We're going to move beyond simple salary numbers and delve into the *why* behind them. We will explore the nuances of the Florida job market, the critical factors that can dramatically increase your earning potential, and a step-by-step roadmap to launch or advance your career. My first brush with the importance of this field wasn't in a classroom, but in trying to decipher a complex hospital bill for a family member. It was a maze of codes and jargon, and I remember thinking, "There has to be a highly skilled professional behind this, translating a medical event into a financial one." That professional is a medical biller and coder, the unsung hero of the healthcare revenue cycle.
This is a career with a robust future, especially in a state like Florida with its growing and aging population. According to the U.S. Bureau of Labor Statistics, the field is projected to grow significantly faster than the average for all occupations. The average billing and coding salary in Florida is competitive, often ranging from $45,000 to over $75,000 annually, depending on a multitude of factors we will dissect in detail.
This is more than just a job; it's a gateway to a lifelong profession in the dynamic world of healthcare. Let's decode your future.
### Table of Contents
- [What Does a Medical Biller and Coder in Florida Actually Do?](#what-they-do)
- [Average Medical Billing and Coding Salary in Florida: A Deep Dive](#salary-deep-dive)
- [Key Factors That Influence Your Salary](#key-factors)
- [Job Outlook and Career Growth in Florida](#job-outlook)
- [How to Get Started in a Medical Billing and Coding Career](#how-to-get-started)
- [Conclusion: Is a Medical Billing and Coding Career in Florida Right for You?](#conclusion)
What Does a Medical Biller and Coder in Florida Actually Do?
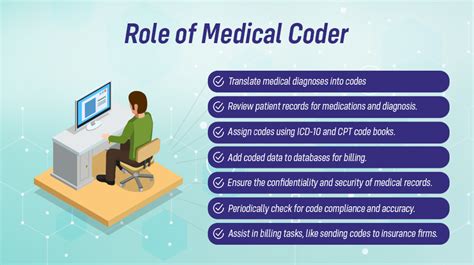
At its core, medical billing and coding is the process of translating healthcare services into a language that insurance companies and payers can understand. These professionals are the critical link between healthcare providers, patients, and insurance companies. Without their expertise, providers wouldn't get paid for their services, and the entire healthcare system would grind to a halt.
Let's break down the two distinct, yet interconnected, roles:
Medical Coding: This is the translation part of the job. A medical coder's primary responsibility is to meticulously review patient records, including physician's notes, lab results, and radiologic reports. From this documentation, they abstract the relevant information and assign standardized alphanumeric codes. These codes represent every diagnosis, procedure, service, and piece of equipment used during a patient's encounter.
The main code sets they use are:
- ICD-10-CM (International Classification of Diseases, 10th Revision, Clinical Modification): These codes are used for diagnoses. Everything from a common cold (J00) to a complex heart condition has a specific ICD-10 code.
- CPT (Current Procedural Terminology): These codes, maintained by the American Medical Association, represent the services and procedures a provider performs, like an office visit, a surgery, or an X-ray.
- HCPCS Level II (Healthcare Common Procedure Coding System): These codes are used for products, supplies, and services not included in CPT, such as ambulance services, durable medical equipment (DME), and specific drugs.
Accuracy is paramount. The wrong code can lead to a rejected insurance claim, underpayment for the provider, or even serious compliance issues and audits.
Medical Billing: This is the financial part of the job. Once the coder has assigned the codes, the medical biller takes over. They create a "superbill" or claim that lists all the services rendered and their corresponding codes. This claim is then submitted electronically to the patient's insurance company for reimbursement.
The biller's job doesn't end there. They are also responsible for:
- Claim Scrubbing: Reviewing claims for accuracy and completeness before submission.
- Payment Posting: Accurately posting payments received from insurance companies.
- Denial Management: Investigating why a claim was denied, correcting any errors, and resubmitting it in an appeal.
- Patient Billing: Creating and sending statements to patients for any remaining balance (deductibles, co-pays, co-insurance).
- Following Up: Communicating with insurance companies and patients to ensure timely payment.
In smaller practices, one person might handle both billing and coding. In large hospitals or healthcare systems, these are often separate departments with highly specialized roles.
### A Day in the Life of a Florida Medical Coder
To make this more tangible, let's imagine a typical day for "Maria," a Certified Professional Coder (CPC) working remotely for a large orthopedic group in Tampa, FL.
- 8:30 AM: Maria logs into her secure portal and accesses the electronic health record (EHR) system. Her queue is populated with patient charts from the previous day's appointments and surgeries. She starts with the straightforward office visits, quickly abstracting diagnoses (like "M17.11 - Unilateral primary osteoarthritis, right knee") and procedure codes (like "99213 - Office or other outpatient visit for the evaluation and management of an established patient").
- 10:00 AM: She moves on to a more complex case: a total knee arthroplasty (TKA). This requires intense focus. She carefully reads the surgeon's operative report, the anesthesiologist's notes, and the hospital discharge summary to ensure she captures every detail correctly. She codes the primary procedure, any additional procedures performed, and all relevant diagnoses, including post-operative conditions.
- 12:00 PM: Lunch break. A quick walk outside to enjoy the Florida sunshine.
- 1:00 PM: Maria joins a virtual team meeting. The practice manager discusses a new policy update from Blue Cross Blue Shield of Florida regarding reimbursement for a specific type of injection. The team discusses how to adjust their workflow to ensure compliance and proper payment.
- 2:00 PM: She receives a "query" from a biller. A claim was denied because a diagnosis code didn't support the medical necessity of a procedure. Maria re-reviews the chart, realizes the physician's documentation was slightly ambiguous, and sends a formal, compliant query back to the physician through the EHR to request clarification.
- 3:30 PM: Maria spends the rest of her afternoon working on her "denials" queue—claims that have come back from insurance companies. She analyzes the denial reasons, makes corrections, and prepares appeals with supporting documentation.
- 5:00 PM: She finishes coding her last chart, reviews her productivity report for the day, and logs off, knowing her work was essential to the financial health of the practice and the proper documentation of patient care.
Average Medical Billing and Coding Salary in Florida: A Deep Dive

Now for the central question: what can you actually earn in this profession in Florida? The salary for a medical biller and coder is not a single number but a spectrum, influenced by the key factors we'll explore in the next section. However, by looking at data from authoritative sources, we can establish a reliable baseline and understand the typical earning potential.
It's important to note that the U.S. Bureau of Labor Statistics (BLS) groups Medical Coders and Billers under the broader category of "Medical Records and Health Information Specialists." This provides a fantastic high-level view of the profession.
### National and State-Level Salary Benchmarks
- National Average: According to the May 2023 BLS Occupational Employment and Wage Statistics, the national median annual wage for Medical Records and Health Information Specialists was $48,780. The lowest 10 percent earned less than $34,640, and the highest 10 percent earned more than $77,930.
- Florida State Average: The BLS data for Florida from May 2023 shows a slightly more favorable picture. The statewide annual mean wage for this profession was $51,660. Florida is one of the states with the highest employment levels for this occupation, with over 15,500 professionals employed.
While the BLS provides a solid foundation, salary aggregators that collect real-time, user-reported data and job postings can offer a more granular look, often separating "coder" and "biller" roles.
- Salary.com, as of late 2023/early 2024, reports that the average salary for a Medical Coder in Florida is around $60,105, with a typical range falling between $52,884 and $68,963.
- Payscale.com indicates that the average base salary for a Medical Coder in Florida is approximately $53,000 per year, with significant increases based on certifications and experience.
- Indeed.com and Glassdoor.com data, based on job listings and user reports, generally align with these figures, showing average base pay in the $48,000 to $58,000 range across the state.
The key takeaway is that the a billing and coding salary in Florida typically starts in the low-to-mid $40s for entry-level positions and can comfortably exceed $70,000 to $80,000 for experienced, certified, and specialized professionals.
### Salary by Experience Level in Florida
Experience is arguably the most significant driver of salary growth. Here’s a breakdown of what you can expect at different stages of your career in Florida, synthesized from data from Salary.com, Payscale, and BLS percentile data.
| Experience Level | Typical Years of Experience | Typical Florida Salary Range | Characteristics of the Role |
| :--- | :--- | :--- | :--- |
| Entry-Level Coder/Biller | 0-2 Years | $40,000 - $52,000 | Recently certified (e.g., CPC-A). Often starts in data entry, payment posting, or coding for a single specialty in a physician's office. Focus is on learning systems and building speed/accuracy. |
| Mid-Career Coder/Biller | 3-7 Years | $53,000 - $65,000 | Holds a full certification (e.g., CPC). Works more independently on complex cases. May handle multiple specialties or work in a more demanding outpatient hospital or surgery center setting. Might start mentoring junior coders. |
| Senior/Lead Coder | 8-15 Years | $66,000 - $78,000+ | Holds multiple certifications (e.g., specialty credentials like CRC or auditing credentials like CPMA). Often works on the most complex cases (inpatient, surgical). Acts as a subject matter expert, audits other coders' work, and queries physicians. |
| Coding Manager/Auditor/Specialist | 10+ Years | $75,000 - $95,000+ | Moves beyond daily coding. Manages a team of coders, develops departmental policies, performs large-scale audits, or works in a highly specialized role like Clinical Documentation Integrity (CDI) or Revenue Cycle Management. Often holds advanced degrees or credentials like RHIA. |
### Beyond the Base Salary: Total Compensation
Your salary is just one piece of the puzzle. When evaluating a job offer, it's crucial to look at the total compensation package, which can add significant value.
- Bonuses: While not universal, some organizations, particularly for-profit hospital systems or large physician groups, offer annual performance bonuses or productivity bonuses. These can be tied to metrics like coding accuracy rates (e.g., maintaining a 95% or higher accuracy) and productivity (e.g., charts coded per hour).
- Profit Sharing: This is more common in smaller, privately owned physician practices. A portion of the practice's annual profits may be distributed among employees.
- Health Insurance: This is a huge factor. A generous employer contribution to your health, dental, and vision insurance premiums can be worth thousands of dollars a year.
- Retirement Savings: Look for a 401(k) or 403(b) plan, especially one with an employer match. An employer matching 50% of your contributions up to 6% of your salary is essentially a 3% raise.
- Paid Time Off (PTO): A generous PTO policy (vacation, sick days, holidays) is a valuable part of your compensation.
- Professional Development: Many employers, especially larger health systems, will pay for your annual certification maintenance fees (e.g., AAPC or AHIMA membership) and provide a budget for continuing education units (CEUs), which are required to keep your credentials active. This is a direct investment in your career growth.
When considering a billing and coding salary in Florida, always ask about these additional benefits. A job offering $55,000 with excellent benefits and a 401(k) match may be financially superior to a job offering $58,000 with poor benefits and no retirement plan.
Key Factors That Influence Your Salary
Why does one coder in Orlando make $48,000 while another in Miami makes $72,000? The answer lies in a combination of factors that create a unique salary profile for every professional. Understanding these levers is the key to maximizing your earning potential. This is the most critical section for anyone serious about building a high-income career in this field.
### ### 1. Certifications and Education
This is non-negotiable for serious earning potential. While it's technically possible to get a job without a credential, your salary and opportunities will be severely limited. Certification is the industry's way of verifying your expertise and competence.
The Power of Certification:
Professional certifications from respected bodies like the AAPC (American Academy of Professional Coders) and AHIMA (American Health Information Management Association) are the gold standard.
- Certified Professional Coder (CPC): Offered by the AAPC, this is the most recognized and sought-after credential for outpatient and physician-based coding. Earning your CPC can instantly increase your starting salary by thousands compared to a non-certified individual. Coders with a CPC consistently earn more than their non-credentialed peers. The AAPC's annual salary survey consistently shows that certified members earn over 20% more than non-certified professionals.
- Certified Coding Specialist (CCS): Offered by AHIMA, this is a highly respected credential, particularly for inpatient hospital coding. Because inpatient coding (using ICD-10-PCS and MS-DRGs) is generally more complex, CCS holders often command higher salaries, especially within large hospital systems.
- Specialty Certifications (The Salary Boosters): Once you have a core credential, earning specialty certifications is the fastest way to increase your value. Each one demonstrates deep expertise in a high-demand area.
- Certified Risk Adjustment Coder (CRC): This is one of the highest-paying non-managerial coding roles. CRCs work with Medicare Advantage plans to ensure patient diagnoses are accurately documented to reflect the patient's true health status. This is a booming field in Florida due to the large Medicare population. CRCs often earn $5,000-$15,000 more annually than general coders.
- Certified Outpatient Coder (COC): For hospital outpatient departments and ambulatory surgery centers.
- Certified Inpatient Coder (CIC): Demonstrates expertise in complex inpatient facility coding.
- Certified Professional Medical Auditor (CPMA): This credential moves you from doing to reviewing. Auditors check the work of other coders for accuracy and compliance, a role that comes with higher pay and responsibility.
The Impact of Formal Education:
While a four-year degree isn't required to become a successful coder, higher education opens doors to higher-level roles and salaries.
- Certificate/Diploma Program: This is the fastest path. A 9-12 month program from a reputable technical college or online provider can prepare you for your certification exam. This is perfect for entering the field quickly.
- Associate's Degree (AAS in Medical Billing and Coding or AS in Health Information Technology): An associate's degree provides a more comprehensive education, including general education courses and deeper dives into anatomy, physiology, and healthcare law. Graduates with an associate's degree, particularly those who earn their Registered Health Information Technician (RHIT) credential from AHIMA, are highly desirable and often start at a higher salary. They are qualified for both coding and health information management roles.
- Bachelor's Degree (BS in Health Information Management - HIM): This is the path to leadership. A bachelor's degree prepares you for the Registered Health Information Administrator (RHIA) credential from AHIMA. RHIAs don't just code; they manage entire health information departments, oversee revenue cycles, ensure data governance and compliance, and work in director-level roles. Their salaries are significantly higher, often starting in the $70,000s and reaching well over six figures.
### ### 2. Years of Experience
As shown in the table above, experience is a direct and powerful driver of salary.
- 0-2 Years (The Apprentice Phase): You are building your foundation. Your focus is on accuracy and speed. You are likely a "Coder I" and may have a CPC-A (Apprentice) designation until you gain enough experience.
- 3-7 Years (The Journeyman Phase): You are a trusted, independent professional. You've removed your "A" status, likely work on more complex charts, and may have earned a second certification. This is where you see the most significant jump from entry-level pay.
- 8+ Years (The Master/Expert Phase): You are a subject matter expert. You are the go-to person for difficult cases, you audit others, and you mentor juniors. Your salary reflects your deep institutional and industry knowledge. Many in this bracket transition to specialized roles like auditing, education, or compliance, pushing their billing and coding salary in Florida to the top of the scale.
### ### 3. Geographic Location within Florida
Not all cities in Florida are created equal when it comes to salary. Pay is often tied to the cost of living and the concentration of large healthcare employers. Data from the BLS and Salary.com reveals distinct regional differences.
| Metropolitan Area | Annual Mean Wage (BLS, May 2023) | Key Factors |
| :--- | :--- | :--- |
| Miami-Fort Lauderdale-West Palm Beach, FL | $55,590 | Highest cost of living in the state. High concentration of large, private, and for-profit hospital systems and specialty clinics. Very competitive market that drives salaries up. |
| Tampa-St. Petersburg-Clearwater, FL | $50,910 | A major hub for healthcare with numerous large hospital networks (BayCare, AdventHealth, HCA). Strong demand across a variety of settings. |
| Orlando-Kissimmee-Sanford, FL | $50,690 | Another massive healthcare market, home to AdventHealth and Orlando Health. A rapidly growing population fuels constant demand for healthcare services and the professionals who support them. |
| Jacksonville, FL | $52,020 | A strong market with major players like Mayo Clinic, Baptist Health, and UF Health. The presence of a prestigious academic medical center like Mayo Clinic can create high-paying, specialized opportunities. |
| Gainesville, FL | $53,730 | This salary is higher than in some larger metros, largely driven by the massive presence of UF Health Shands Hospital, a major academic medical center and employer that requires highly skilled, specialized coders. |
| Nonmetropolitan Areas (e.g., Panhandle, North Central FL) | $43,770 - $46,550 | Lower cost of living corresponds with lower average salaries. Fewer large hospital systems mean opportunities may be more concentrated in smaller clinics or critical access hospitals. Remote work is a game-changer for professionals in these areas. |
### ### 4. Company Type & Work Environment
Where you work has a profound impact on your daily tasks, the complexity of your work, and your paycheck.
- Large Hospital Systems (e.g., HCA Florida, AdventHealth, Cleveland Clinic Florida): These are often the highest-paying employers. They offer opportunities for specialization (inpatient, outpatient, trauma, cardiology) and clear career ladders. They also typically provide the best benefits packages and professional development support.
- Physician's Offices / Small Clinics: These are excellent entry points into the field. The work might be less complex (focused on one or two specialties), but you gain hands-on experience across the entire revenue cycle. Salaries may start lower than at hospitals but can grow as you become indispensable to the practice.
- Insurance Companies (Payers): Working for a company like Florida Blue or UnitedHealthcare offers a different perspective. You'll be on the other side, reviewing claims submitted by providers. These roles often involve auditing and ensuring payment integrity, and they can be quite lucrative.
- Third-Party Billing Companies: These companies handle billing and coding for multiple small practices that can't afford an in-house team. This can be a fast-paced environment where you are exposed to many different specialties, which is great for learning.
- Remote Work / Freelance: The rise of remote work has been a revolution for coding. Many Florida coders work for companies based all over the U.S. This allows you to access higher-paying jobs in different markets while enjoying the Florida lifestyle. Freelance or contract coding can also be highly profitable, with experienced coders billing by the hour or by the chart, but it requires self-discipline and business acumen.
### ### 5. In-Demand Skills and Specializations
The skills you possess beyond basic coding can set you apart and command a premium salary.
- Specialization in Complex Areas: As mentioned, inpatient coding (CCS) and risk adjustment coding (CRC) are highly valued. So is surgical coding, which requires an expert understanding of anatomy and complex procedures.
- EHR/EMR Proficiency: Being a power user of major Electronic Health Record systems like Epic and Cerner is a huge plus. Employers want someone who can hit the ground running with their specific technology stack.
- Revenue Cycle Management (RCM): Understanding the entire financial lifecycle of a patient encounter—from registration to final payment—makes you more valuable than someone who only knows how to assign a code.
- Auditing and Compliance: Skills in medical auditing (CPMA) are in high demand as healthcare organizations face increasing scrutiny. Knowledge of HIPAA, Stark Law, and other regulations is crucial for higher-level roles.
- Clinical Documentation Integrity (CDI): This is an advanced role for experienced coders, often with a clinical background (like nursing). CDI specialists work directly with physicians to improve the quality of documentation in the medical record. This ensures that the documentation accurately reflects the patient's severity of illness, which directly impacts reimbursement and quality metrics. CDI roles are among the highest-paid in the health information field, often exceeding $85,000-$90,000 in Florida.
- Soft Skills: Don't underestimate communication! The ability to write a clear, concise, and professional query to a physician is a skill that saves organizations thousands of dollars and is highly valued.
Job Outlook and Career Growth in Florida
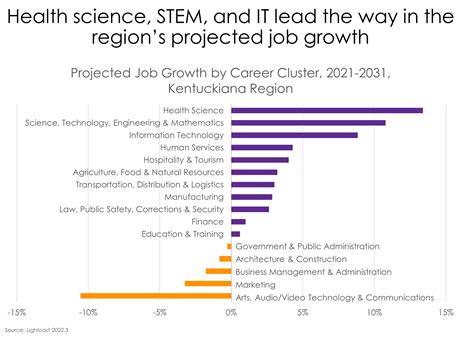
For those considering this career, the future is bright, both nationally and within the state of Florida. The demand for skilled medical billers and coders is not just stable; it's growing at a pace that outstrips many other professions.
### A Profession on the Rise
The U.S. Bureau of Labor Statistics' Occupational Outlook Handbook is the definitive source for job projections. For Medical Records and Health Information Specialists, the BLS projects a 7 percent growth in employment from 2022 to 2032. This is significantly "faster than the average for all occupations," which translates to approximately 15,200 new job openings each year across the country over the next decade.
Why such strong growth? Several powerful forces are at play, and they are particularly potent in Florida:
1. An Aging Population: Florida is a well-known destination for retirees. As the massive baby-boomer generation ages, they require more medical services, from routine check-ups to complex surgeries and long-term care. Every single one of these encounters needs to be coded and billed correctly, creating a sustained, long-term demand for your skills.
2
